Request for Proposal
advertisement
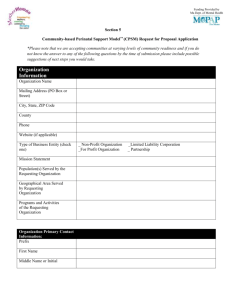
Community-based Perinatal Support Model© (CPSM) Request for Proposal Community Application for Participation in CPSM© March 6, 2014 Funding provided by: Funding provided by: 1 Request for Proposals Community-based Perinatal Support Model© (CPSM) Overview I. Request for Proposal Description MotherWoman is requesting proposals from qualified communities to participate in the statewide implementation of the Community-based Perinatal Support Model© (CPSM). The CPSM is an intervention that allows communities to address the issues of perinatal depression and ensures that multi-disciplinary partners throughout a community and across systems of care have the tools they need to identify mothers at risk and provide appropriate referral and treatment. No monetary support will be provided to participating communities through this RFP; however services provided to communities equal an estimated value of $65,000. Recipients should be able to define a “lead agency” (a champion in their community willing to take the lead on CPSM implementation), identify potential coalition partners, and be interested in addressing barriers to care for mothers with perinatal depression both within their own home agency/organization as well as across multiple systems (medical, mental health, human services) within the community. The CPSM will provide communities with: community readiness assessment, three-hour CPSM Community Training, the CPSM toolkit, three-day MotherWoman Group Facilitator Training© to develop and guide support groups, MotherWoman Support Group Model©, continuing education webinars, training for the leadership team, recommended community-specific action plan, mentorship, technical support, and online resources. CPSM Coalition Partners: Medical: obstetric, pediatric and primary care providers, nurses, hospitals, NICU, behavioral health, in-patient, psychiatric providers and any other medical providers caring for perinatal mothers Mental Health: psychologists, psychiatrists, counselors, social workers, crisis centers, and any other mental health providers caring for perinatal mothers Social Service: public health departments, WIC, early intervention, Department of Children and Families, parent educators, home visitors and any other social service providers caring for perinatal mothers Community Organizations: community centers, community organizations, religious organizations, family centers and any other community organizations caring for perinatal mothers Mother and Family Advocates: with lived experience Applicants may include but are not limited to; medical health centers, mental health agencies, public health departments, hospitals, community centers, community organizations, and social service agencies. Communities already receiving support or pre-existing coalitions may still apply but please provide justification for need of further assistance and how it will benefit the community. This may include expansion into new communities and/or deeper reach into unique communities within the preexisting catchment. Anyone in the community interested in pursuing greater resources for mothers experiencing perinatal depression is eligible to provide the letter of intent for this RFP. 2 The CPSM supports communities to meet the following goals: 1) Build the capacity of providers including medical, mental health, social service, and community support organizations 2) Develop community-based coalitions that will address the gaps in services and provide a clear pathway from identification and screening to treatment, between medical, mental health, and social service providers 3) Expand resources within communities through readily available culturally competent support groups to enhance and increase already existing mental health resources RFP recipients will receive the CPSM which includes the MotherWoman Support Group Model©. Recipients will receive: community readiness assessment, three hour CPSM Community Training, the CPSM toolkit, three day MotherWoman Support Group Facilitator Training© to develop and guide support groups, four continuing education webinars, two day CPSM training for your selected leadership team, expert support to guide in the formation of your working group, recommended community-specific action plan, mentorship and technical support, as well as numerous online resources. When applying to this RFP, please submit a letter of intent (LOI). The LOI should clearly state interest in the CPSM. The LOI does not need to be written by the lead agency, and can be an opportunity to begin a community conversation about the RFP as well as serve as a request for additional information. For the first phase of implementation of the CPSM, six communities will be selected to participate in the project activities. Additional communities may be put on a wait list and receive the CPSM in the months following the original implementation of the CPSM. Perinatal Emotional Complications: Description of Need MotherWoman’s approach to Postpartum depression is the leading complication of childbirth, communicating with mothers and providers affecting 10 – 20% of all mothers1 and 40 – 60% of low-income about perinatal depression mothers.2 Maternal depression can have a lasting negative impact on the behavioral, cognitive, and social-emotional functioning of Feelings and behaviors which cause children.4 Depression during pregnancy has been linked to poor birth mothers distress and interfere with their outcomes, such as low birth weight, pre-term delivery and obstetric functioning, including depression and complications.4, 5 Postpartum depression is also correlated with a anxiety across a spectrum of severity. The mother’s inability to attend to health issues for her infant, such as spectrum includes normal pregnancy and decreased breastfeeding, missed well-child pediatric visits and postpartum adjustment and stress, as well inattentiveness to safety protocols for infants, such as car restraints and as baby blues, depression, anxiety, and Sudden Infant Death Syndrome prevention sleeping panic disorders. recommendations.2 Every year approximately 73,000 babies are born in Massachusetts.3 Postpartum depression may affect from 7,300 to 14,600 mothers in Massachusetts annually. Very few of these women receive effective treatment, many of them are low-income and a disproportionate number of mothers who do not receive appropriate treatment are women of color, teens and immigrants.3,6 In 2000 the cost of depression in the U.S. totaled $83.1 billion dollars.7 The specific costs of perinatal depression are unknown; however, pregnant women with untreated depression are at risk for costly 3 complications, such as preterm birth.8 In 2005, costs for all preterm births totaled at least $26.2 billion, or $51,600 for every infant born prematurely.9 Additionally, children of depressed mothers may also have higher lifetime medical spending due to the adverse effects of postpartum depression on the child’s own health. Research has demonstrated that children with depressed mothers are significantly more likely to experience poorer mental health and motor development. Postpartum depression in mothers is also linked to an increased risk for poor interpersonal connections, attachment issues, and behavioral problems in children.12 Children with depressed mothers have been found to use health care services, including office and emergency room visits, more frequently than children of healthy women.8 A previous study concluded that the cumulative effect of maternal depression and related risk factors impact percentage of children experiencing aggression, anxiety, depression, and hyperactivity.13 Communities that engage in coalitions may be able to make more efficient referrals to appropriate resources, like early intervention, and thus address overall costs. Research has demonstrated that for every $1 spent in early intervention services communities save approximately $9 in future costs.10 A recent program from Pennsylvania, Helping Families Raise Healthy Children, demonstrated the importance of cross-system networking opportunities, trust between providers and caregivers, the need for structure and support to accompany referral, and the need for cross-system training and organization, for success in assisting moms experiencing perinatal depression.11 All of these outcomes are the goals of the CPSM. CPSM Success Story: Franklin County, MA In 2009, mothers in Franklin County had nowhere to go and no systems in place to support them when struggling with perinatal depression. In August 2009, MotherWoman began a pilot project called the “Franklin County Pregnancy and Postpartum Support Coalition” which implemented the CPSM in response to the needs of area families and healthcare providers. Prior to implementation of the CPSM, there were no systems in place to support mothers’ with perinatal depression including no screening, no training, no referral network and no community support group. Over the first 18 months in which the CPSM was implemented there were marked improvements in: Coalition development – the establishment of a leadership team that comprised of key organizations, practices, and county hospital. Public education – various media and marketing strategies were successfully implemented and materials distributed at patient access points such as hospitals, family centers, mental health centers, and medical offices. Professional training – CPSM successfully trained 100 providers in the first 18 months of implementation from various professions such as: crisis, mental health, Department of Children and Families, WIC, social service, OB/GYN, nurses, psychiatry, pediatric, family practice and others who care for mothers and infants during pregnancy and the first year of life. Four years later, Franklin County has trained over 200 professionals to assist in providing mothers with the necessary care and treatment. Community resources and support groups – Support group for mothers with perinatal depression and Mother-to-Mother Support Program were developed. Additional community resources were linked to one another and identified through the process. Resource and referral guide for providers and mothers was developed and remains a cornerstone to success of the coalition efforts. 4 Referral and Triage Protocols – Site-specific triage protocols were established to develop integration of services for screening and referral with integration across systems of care. Triage protocols between systems were developed so that providers know how to connect mothers with appropriate resources like early intervention, support groups, and mental health services. For example, the leading mental health agency prioritized several perinatal mental health slots each week to triage crisis situations decreasing weight lists and increasing access to care. Screening and Policy Implementation for perinatal depression – In Franklin County, after 18 months of CPSM implementation, there was 90% universal screening at prenatal visits, 100% screening at postpartum hospital stay, and 90% universal screening at pediatric visits during the 1st year of child’s life. Initial findings show that in communities in which the CPSM is implemented, providers are more prepared to address perinatal depression in the office, to be informed on how to refer mothers when necessary, and have the relationships and connections to mental health and other services to ensure success with referral. Additionally, early intervention, social services and mental health providers have the training necessary to treat mothers with perinatal depression and have relationships with medical providers to ensure successful linkage of mothers from screening to treatment. “The CPSM made all the difference in our ability to meet the needs of mothers with perinatal depression. We are grateful for their training and support. Now we can do it ourselves!” Linda Jablonski, RN, MSN, Assistant Nurse Manager, Franklin Baystate Medical Center Today, the Franklin County Perinatal Support Coalition is fully functional just celebrated their fourth anniversary. They have over 30 member organizations, have continued to address perinatal depression, and take on new challenges regarding perinatal mental health utilizing the CPSM model. Description of Grantor The mission of MotherWoman is to empower mothers to make positive personal and social change by building community safety nets, impacting family policy and promoting the leadership and resilience of mothers. MotherWoman serves mothers, families and thereby the community by: • Supporting and Empowering Mothers by training community leaders and professionals to lead MotherWoman Support Groups across the region • Building Community Safety Nets for women and families in the perinatal period by supporting communities in the implementation of the CPSM • Impacting Family Policy by engaging mothers, fathers and caregivers to take action on policies that impact families MotherWoman seeks to create a culture that understands and de-stigmatizes screening and treatment of perinatal depression. MotherWoman promotes evidence-informed models in prevention, detection, and treatment of perinatal depression by addressing barriers to care. Funding for this RFP has been made possible by the Massachusetts Child Psychiatry Access Project (MCPAP). MCPAP is funded by the Department of Mental Health. MCPAP for Moms is an expansion of the successful Massachusetts Child Psychiatry Access Project (MCPAP), which has improved child 5 mental health care in Massachusetts by offering pediatric primary care providers rapid access to child psychiatry consultation, education, and care coordination. MCPAP for Moms aims to promote maternal and child health by building the capacity of providers serving pregnant and postpartum women and their children up to one year after delivery to effectively prevent, identify, and manage depression. Providers working with fathers and other caregivers experiencing perinatal depression can also access MCPAP for Moms. MCPAP for Moms is partnering with MSPP Interface Referral System and MotherWoman to ensure that mothers receive the care and treatment they need. MSPP INTERFACE Referral Service will recruit providers with experience in perinatal treatment and provide a database of vetted professionals, groups, and organizations with experience in perinatal concerns. In addition, MSPP INTERFACE will develop and provide guides for women and families as they seek access to care, and provide training to care coordinators and other community members in best practice for resource and referral for mental health. The Community-based Perinatal Support Model© (CPSM) will provide communities with the infrastructure, training and support necessary to develop unified community-wide goals for systemic change and implement protocols across systems to enhance delivery of treatment to women in need. II. Eligible Communities You may submit an application if your community has any of the following characteristics: • • • III. One primary leader who is committed to addressing perinatal depression within the community. We understand that change takes time and community buy-in is a process. The CPSM has been successfully implemented in communities with wide provider participation even when the original inception was not based on broad support across systems of care. One organization or “lead agency” that will submit the RFP and guide implementation. This organizations may consist of any of the following: o Public institution o Non-profit private institution o Academic entity o Unit of local or State government o Eligible agency of the Federal government Minimum of 3-5 community entities (agencies/organizations) committed to participating in the RFP as evidenced by Memorandum of Agreement. These entities should represent some of the following: o Medical health centers (pediatric, obstetrical, psychiatric, behavioral health, inpatient) o Hospitals o Mental health agencies o Social Services (WIC, Early intervention, Department of Children and Families, etc.) o Community organizations (Family Centers, Community centers) o Other Key Dates 6 Table 1. Proposal Key Dates Activity Due Date Announcement and Distribution of RFP March 6, 2014 Letter of Intent* March 19, 2014 RFP Informational Webinar March 26, 2014 at 12p.m. This will be recorded and available after live presentation. Proposal Electronic Submission April 18, 2014 Selection Notification April 28, 2014 Signed Contract May 5, 2014 Contract Start Date May 15, 2014 PHASE 1 Trainings CPSM Community Training Thursdays in May and June from 1pm – 4pm Facilitator Training June 4th-7th PHASE 2 Trainings Mentorship, Technical Assistance, Additional July 2014-May 2015 Training, Continuing Education for MotherWoman Support Groups, Toolkit, etc. * Note: A letter of intent must be submitted electronically by March 19, 2014 by 5:00pm EST to attend the RFP Informational Session; Due dates are best estimates and may be subject to change *Phase 2 Trainings are contingent on available funding. However, MotherWoman is confident in receipt of additional funding. IV. Table of Contents Section 1 – Background…………………………………………………………………..pg 8 Provides applicants with background information on the task to be performed and defines deliverables Section 2 – Administrative and Submission Information…….…………………………. pg 13 Describes the administrative grant process and submission requirements to applicants. Section 3 – Proposal Evaluation…………………………………………………………pg 15 Describes how the proposals will be evaluated. Section 4 – Attachments…………………………………………………………………pg 17 Provides list of documents required from applicants. Section 5 – Application Form……………………………………………………. (See attachment) Provides application form that must be completed by applicants. Section 5 is a separate attachment available as a word document to input text directly. Section 1 7 Background I. Introduction A. Overview MotherWoman has developed the Community-based Perinatal Support Model© (CPSM) to ensure that mothers experiencing perinatal depression receive the necessary care and treatment by developing and enhancing resources available within the community. Our goal is to support community capacity by expanding resources, increasing provider competence and promoting mothers' inherent resilience at all points of provider contact from first prenatal visit through the one-year well-child check. CPSM maximizes the collective impact that committed leaders across diverse sectors of the maternal care and mental health community can have in addressing perinatal depression. There is general consensus that even when there is screening and referral, unless there is "community-readiness," which includes an understanding of the health risks of perinatal depression for mothers, infants and families, professional training for providers across sectors, and the development and identification of resources, a community will not reach the goal of ensuring that women receive the care and treatment that they need. Through the CPSM, communities will implement key components necessary to provide every mother with the support to address her mental health needs during pregnancy and the first year with baby. The key elements of the CPSM include: Mothers and their families at the center of community solutions through engagement of mothers as key members in all of the following elements. Ongoing community readiness assessment to identify stage(s) of community readiness and inform implementation of system-wide perinatal depression policies. Specific community strategies will be identified and modified based on community readiness level. This will include training, toolkit, technical assistance and action plan. Leadership team and network development. Leadership team of cross-disciplinary partners will be identified and support will be provided for collaboration across systems. Formation of coalition including engagement of all community partners: health care providers (including obstetric, pediatric and psychiatric providers), mental health and social service agencies, crisis services, early intervention specialists, home visiting providers, parent educators, WIC workers, hospital based care, mothers with lived experience, etc. Development of a community-specific action plan for the necessary intervention strategies to decrease barriers to care and increase mothers’ access to identification and treatment of perinatal depression (including but not limited to addressing the following goals: public education, professional training, development and identification of resources, triage and referral protocols and universal screening.) Toolkit, training, technical assistance and resources provided by MotherWoman for communities to meet the identified action plan Implementation of MotherWoman Support Group Model© within the community including training, mentorship, and continuing education 8 II. Primary Products A. The Community-based Perinatal Support Model© (CPSM) Community coalitions will engage providers in an intervention that promotes change through a multimodal model that encourages agencies and systems to work together. The entire pediatric and perinatal health community will be invited and included in the community-wide coalitions; including child birth educators, medical provider representatives (obstetrical providers, pediatric providers, PCPs), early intervention specialists, home visitors, as well as social service providers such as WIC and the Department of Children and Families, mental health providers, domestic violence support services and addiction recovery providers. Greatest success comes when key partners are working together to develop and implement the CPSM. The content of the Community-based Perinatal Support Model© that MotherWoman will provide awardee communities includes: 1. CPSM Community Training a. Training will include: One three-hour community training based on the CPSM and community readiness assessment. This training is intended for cross-disciplinary participation and will be appropriate for diverse providers. i. Overview of perinatal depression and de-stigmatizing framework ii. Risk factors and how to support maternal/family resilience iii. Screening and therapeutic interviewing iv. Evidence-based treatment options and approaches to care, including the necessity of support groups v. Introduction to the CPSM vi. Community-readiness assessment process 2. Community-based Perinatal Support Model© Tool-Kit to assist in delivering the CPSM to community and sustaining change. Toolkit will include: a. Leadership team building and sustaining resources; including tips for facilitating a successful coalition meetings, educational resources for mothers, resource and referral process and template, triage process, support group materials, screening tools, and provider packets. b. Identification and expansion of maternal mental health resources c. Perinatal Community Change Road Map: This is an action plan developed with community leaders that specifically outlines the plan for implementation 3. Training for leadership team – to define and develop the Perinatal Community Change Road Map 4. Technical support and consultations, not to exceed five hours per and tailored to fit community need 5. Online and state-wide resources B. MotherWoman Support Group Model© 9 The second core product that MotherWoman will provide recipient communities in the delivery of MotherWoman Support Group Model©. MotherWoman Support Groups are an evidence-informed, psycho-educational support group model, which integrates leading clinical theories and modalities in the treatment of perinatal depression, including cognitive behavioral and interpersonal therapies. The MotherWoman Support Group Model© is trauma informed, with a strong emphasis on traditional group dynamics and a sensitivity to issues of social and economic inequality. MotherWoman Support Groups provide mothers with effective, culturally competent, easily accessible emotional support during the critical perinatal period. Key elements of MotherWoman Support Groups are inclusive, de-stigmatizing support and psychosocial education. Group facilitators are selected from community organizations and have varying professional degrees and areas of specialization including but not limited to: nursing, psychology, psychiatry, mental health, social work, early intervention, social services, and mothers with lived experience of perinatal depression. Research suggests: 1) Support Groups reduce the burden of identifying an appropriate referral treatment option and expedite referrals to other community providers. Physicians are more confident in screening when they know how and where to refer mothers. 2) Mothers who attend Support Groups receive additional referrals in a de-stigmatizing environment thus increasing the likelihood of follow-through and promoting the appropriate utilization of specialized resources. 3) Support Groups are cost-effective, community-based interventions providing a first level mental health resource to mothers, which we predict will reduce the need for emergency services and overall costs of mental health care delivery. 4) Support Groups have the potential to provide culturally appropriate mental health resources within communities, especially important when available mental health resources may be scarce. Empirical and preliminary research indicates that MotherWoman Support Groups help women experiencing perinatal depression to regain their stability, resilience and more easily connect with necessary community-based mental health resources. MotherWoman will provide recipient communities with the following: Three-day MotherWoman Group Facilitator Training© (for two attendees to be designated by lead community agency/coalition) Mentorship program, which provides regular consultation with an experienced mentor/facilitator to identify areas of concern, increase knowledge and develop goals towards a successful support group in the community. MotherWoman Group Facilitator Manual, MotherWoman Perinatal Support Group Curriculum and toolkit for successful implementation Webinar continuing education to support fidelity and quality assurance to be provided to facilitators. These will address issues of high concern for new facilitators. C. Target Population 10 PLEASE NOTE: The CPSM is designed to assist communities in increasing community readiness. MotherWoman is interested in engaging with communities at varying levels of readiness, from early stages of awareness of this issue to those with higher levels of engagement. For the first phase of implementation of the CPSM six communities will be selected to participate in the project activities. Additional communities may be put on a waitlist and receive the CPSM in the months following the original implementation of the CPSM. The target for this proposal is communities, which have an interest in improving community standards of care in addressing perinatal depression. The community should be defined thoroughly by applicant (i.e. county, town, city, hospital centered, neighborhood, community health center catchment area, etc.) The applicant should be able to specify a “lead-agency” that will initiate implementation of CPSM activities and show responsibility for the project. Applicant should be able to specify 3-5 committed partners from diverse segments of the service provider community. If committed partners are not identified in time to submit application, please provide pathway to engage committed partners and plan for recruitment. RFP recipients should also be able to report hospital commitment to engage in the CPSM. If hospital engagement is not available at the time of submission, please provide pathway to engage hospital. Submissions are recommended, but not required to have some or all of the following qualifications. If commitment is not available by the time of the application for any of the following, please provide a brief explanation for pathway to commitment. 1. Defined “lead agency” or organization willing to take charge of CPSM activities and report back to CPSM staff and mentors on community progress. Responsibilities of lead agencies include but are not limited to: organize meetings, take minute notes, oversee process, ensure implementation of community support group, etc. Lead agency should expect to devote approximately 1-5 hours per week/month to tasks related to the CPSM. 2. Experience, or be willing to, provide outreach to the community. 3. Experience, or be willing to, work with diverse members of the community. 4. Capacity to communicate within the community (ability to recruit members, promote trainings, and engage community members in coalition activities). 5. Commitment from hospital for participation in the CPSM. 6. Familiarity with the community as defined by the community. 7. Relationship with 3-5 committed partners from diverse segments of the service provider community who will be engaged in monthly meetings, engage in implementation of the action plan at the agency level and at the community level, and support of leadership to implement change (demonstrated in the MOA). Can include but are not limited to: religious organizations, law enforcement, mental health and treatment services, social services, health care centers (including obstetric, pediatric and psychiatric providers), hospitals, community organizations, public health departments, etc. 8. Preference will be shown to applicants with a relationship to the community birthing centers and hospitals. 9. Familiarity with resources available within the community to include in and inform the CPSM. Resources may include: agencies, organizations, service providers, support groups, triage and referral protocol, screening, and health and wellness services. 11 10. Ability to identify and/or provide a location for CPSM Community Trainings and Support Groups. Contract Period The expected term of this contract is from May 15, 2014 – May 15, 2015. The length of contract may vary by community depending on current level of readiness and ability to perform related activities. The contract may be extended. MotherWoman depends on state funding which is expected to continue through the next fiscal year. Length of contract is contingent on receipt of funding. Section 2 Administrative and Submission Information 12 I. Submission of Letter of Intent (LOI) Anyone in the community interested in creating greater resources for mothers experiencing perinatal depression is eligible to provide the Letter of Intent for this RFP. The LOI should clearly state your interest in the CPSM. The LOI does not need to be written by the lead agency, and can be an opportunity to begin a community conversation about the RFP as well as serve as a request for additional information. The letter of Intent may be submitted by email to cpsm@motherwoman.org no later than March 19th 5p.m., 2014. II. RFP Informational Webinar Session The RFP Informational Webinar Session is limited to applicants who submit a letter of intent. Date: March 26th at 12pm, 2014 A recording will be available following the live presentation. Upon receipt of letter of intent, you will be sent information on how to register for the online webinar. Applicants are encouraged to submit written questions prior to the informational session. A section of the Webinar will be focused on participant questions. Submission of Questions Applicants may submit questions to cpsm@motherwoman.org at any time before April 18, 2014 at 5:00 p.m. All questions will be answered within 48 hours of receipt. A summary of questions and answers will be distributed and emailed to all applicants who submit a letter of intent. III. Discussion with Applicants Prior to Submittal Deadline - Discussions may be conducted with potential applicants to promote understanding of the requirements. Please email and/or call MotherWoman: cpsm@motherwoman.org or call at 413-387-0703. After Proposal Submittal Deadline - Discussions may be conducted with applicants whose proposals are determined to have reasonably met the award selection criteria. However, proposals may be considered without discussions at the discretion of MotherWoman. Confidential Information – If an applicant believes that any portion of a proposal contains information that should be withheld as confidential, the applicant shall request in writing nondisclosure of designated proprietary data to be confidential and provide justification to support confidentiality. Such data shall accompany the proposal, be clearly marked, and shall be readily separated from the proposal to facilitate eventual public inspection of the non-confidential sections of the proposal. IV. SUBMISSION OF PROPOSALS All proposals must be submitted electronically via e-mail to cpsm@motherwoman.org no later than April 18, 2014 by 5:00 p.m. Supplementary information will not be accepted after the deadline, unless requested by MotherWoman to clarify the proposal. We will confirm receipt of proposals via e-mail within 24 hours of receipt. 13 Format – All proposals should be submitted electronically in a word document typed using Times New Roman 11 point font, single-spaced, and with one inch margins. Applications should be no longer than 10 pages. V. ADDITIONAL MATERIALS AND DOCUMENTATION Upon request from MotherWoman, applicant shall submit any additional materials and documentation reasonably required by MotherWoman in its evaluation of the proposals. VI. CONTINGENCIES MotherWoman reserves the right to accept or reject any or all submitted proposals, in part or in entirety, as a response to the Request for Proposal. MotherWoman has the right to amend this RFP at any time prior to the closing submission date. All organizations that submit a letter of intent will be notified via email of changes to the RFP. VII. NOTICE OF AWARD The selected recipient will be notified by e-mail approximately two weeks after proposal close date. Section 3 Proposal Evaluation 14 I. Introduction The evaluation of proposals received in response to this RFP will be conducted comprehensively, fairly, and in an unbiased manner. Structured quantitative scoring techniques will be utilized to ensure and maximize the objectivity of the evaluation. Each applicant will be objectively scored based on the following categories: (1) Engagement –community recognition and understanding of perinatal depression, community vision for change, available resources, and leadership for implementation of the CPSM. (2) Relationships – dedicated community partners and collaboration with community leaders to implement CPSM. (3) Commitment – state of dedication to supporting mothers’ and families’ health by implementing the CPSM. Availability for trainings, support groups, and mentorship. Resources devoted to CPSM activities (i.e. location for training or support groups, time to dedicate to the CPSM). (4) Vision – organization’s focus on the potential of the community, including an outline of how you envision the community’s future and the pathway to turning that vision into a reality. Be innovative in thinking about your plan. (5) Capability - ability to perform, engage, and achieve CPSM activities through community partnerships, agency/organization leadership, and community commitment utilizing CPSM toolkit, resources, and training, as well as community innovation, skills, and current resources. II. Evaluation Process An evaluation committee with a background and knowledge of the CPSM program responsibilities and program service will review and evaluate proposals. Evaluation Categories Possible Points Administrative Requirements Pass or Fail Proposal Application 100 Points Engagement 20 points Relationships 20 points Commitment 20 points Vision 20 points Capability 20 points Total possible points 100 Points 15 Section 4 16 Attachments The applicant’s proposal must contain the following components when submitting their application. Attachment A. Letter of Intent Attachment B. Request for Proposal Application Attachment C. Memorandum of Agreement (MOA) Please include in the MOA Identified “lead agency” – champion organization that will take lead over CPSM activities List of 3-5 agencies/organizations which will serve as key members of the community coalition/taskforce and the proposed role they will play in implementation of the CPSM and MotherWoman Support Groups. If 3-5 agencies are not available at time of application please provide description of plan to recruit agencies for implementation of the CPSM. List of 3-5 individuals with decision-making capabilities within each agency or organization that can participate in CPSM activities for 1-5 hours per month to the implementation of the CPSM/Support Groups and are able to provide information for the community readiness assessment. If individual are not available at the time the application is due please provide outreach strategies for these individuals. References 17 1. Gaynes B. Gavin N. (2005).Meltzer-Brody S et al. Perinatal depression: Prevalence, Screening Accuracy, and Screening Outcomes. Agency for Healthcare Research and Quality, Evidence Report/Technology Assessment, Number 119. 2. Isaacs M.(2008). Maternal Depression: The Silent Epidemic in Poor Communities. Baltimore, MD, Annie E. Casey Foundation. 3. Massachusetts Births 2010. Boston, MA: Division of Research and Epidemiology, Bureau of Health Information, Statistics, Research, and Evaluation, Massachusetts Department of Public Health. 4. Deave T. Heron J. Evans J. Emond A. (2008). The Impact of Maternal Depression in Pregnancy on Early Child Development. British Journal of Obsterics and Gynecology. 5. Chung E.K. et.al. (2004).Maternal Depressive Symptoms and Infant Health Practices Among Low-Income Women, Pediatrics,. 6. Feinberg E. Smith M. Naik R. (2009). Ethnically Diverse Mothers’ Views on the Acceptability of Screening for Maternal Depressive Symptom During Pediatric Well-Child Visits, J Health Care Poor Underserved,.. 7. National Business Group on Health (NBGH). (2005). Preventing, Identifying and Treating Maternal Depression: Tools for Employers. Issue Brief, March 2005. 8. Ibid. 9. March of Dimes. Premature Birth. Help Reduce Cost: The Economic Costs. Available at: http://www.marchofdimes.com/prematurity/21198_10734.asp. 10. Landry, S.H., (2005). Effective Early Childhood Programs: Turning Knowledge into Action. Available at http://www.childrenslearninginstitute.org/library/publications/documents/EffectiveEarly_Childhood-Programs.pdf o. 11. Schultz, D., Reynolds, K.A., Sontag-Padilla, L.M., Lovejoy, S.L., Firth, R., Pincus, H.A., (2013). Transforming Systems for Parental Depression and Early Childhood Developmental Delays: Findings and Lessons Learned from the Helping Families Raise Healthy Children Initiative. RAND Health. 12. Murray, L., Cooper, P.J., (1997). Effects of Postnatal Depression on Infant Development. Archives of disease in Childhood. 77: 99 – 101. 13. Knitzer, J., Theberge, S., Johnson, K. (2008). Reducing Maternal Depression and Its Impact on Young Children: Toward a Responsive Early Childhood Policy Framework. National Center for Children in Poverty. 18