Parasitism
advertisement

Host-parasite relationship
Stage 3, 2014-2015
Symbiotic associations
All living animals are used as habitats (place in which an animal or
plant naturally grows or lives) by other organisms, none is exempt
(free, released from obligation) from such invasion.
As evolution has produced larger, more complex and better
regulated bodies, it has increased the number and variety of
habitats for other organisms to colonize.
The most complex bodies, those of birds and mammals, including
humans, provide the most diverse environments, and are the most
heavily colonized.
The relationships between symbiotic associations, most species are
independent of other species or rely on them only temporarily for
food, exp. predators and their prey, (creature which hunts other
creatures for food).
As the normal flora demonstrates, pathogenesis is not the
inevitable (unavoidable, inescapable) consequence of host-microbe
associations. Many factors influence the outcome of a particular
association, and organisms may be pathogenic in one situation but
harmless in another.
To understand the microbiologic basis of infectious disease, hostmicrobe associations that can be pathogenic need to be placed
firmly in the context (background) of other symbiotic (interspecies)
associations, such as commensalism or mutualism, where the
outcome for the host does not normally involve any damage or
disadvantage.
1
Some species form closer associations termed 'symbioses' and
there are three major categories-commensalism, parasitism and
mutualism-though each merges (blend or combine) with the other
and no definition separates one absolutely from the others.
Commensalism
In commensalism one species of organism uses the body of a larger
species.
A commensal association is one in which one species of organism
uses the body of a larger species as its physical environment and
may make use of that environment to acquire nutrients.
Like all animals, humans support an extensive commensal
microbial flora on the skin, in the mouth and in the alimentary
tract. The majority of these microbes are bacteria, and their
relationship with the host may be highly specialized, with specific
attachment mechanisms and precise environmental requirements.
Normally such microbes are harmless, but they can become
harmful if their environmental conditions change in some way
(exp. Bacteroides, Escherichia coli, Staphylococcus aureus).
Conversely, commensal microbes can benefit the host:
1. Commensalism can prevent colonization by more pathogenic
species (exp. the intestinal flora).
2. Commensal microbes produce metabolites that are used by the
host (exp. the bacteria and protozoa in the ruminant stomach
(characterized by drawing back from mouth and re-chewing of food).
Mutualism
Mutualistic relationships provide reciprocal (mutual, joint,
common) benefits for the two organisms involved.
2
Frequently the relationship is obligatory for at least one member,
and may be for both. Good examples are the bacteria and protozoa
living in the stomachs of domestic ruminants, which play an
essential role in the digestion and utilization of cellulose, receiving
in return both the environment and the nutrition essential for their
survival.
The dividing line between commensalism and mutualism can be
hard to draw. In humans, good health and resistance to colonization
by pathogens can depend upon the integrity of the normal
commensal enteric bacteria, many of which are highly specialized
for life in the human intestine, but there is certainly no strict mutual
dependence in this relationship.
Parasitism
In parasitism the symbiotic relationship benefits only the parasite.
The terms 'parasites' and 'parasitism' are sometimes thought to
apply only to protozoans and worms, but all pathogens are
parasites.
Parasitism is a one-sided relationship in which the benefits go only
to the parasite, the host providing parasites with their
physicochemical environment, their food, respiratory and other
metabolic needs, and even the signals that regulate their
development.
In fact many 'parasites' establish quite innocuous (harmless)
associations with their natural hosts and are not at all pathogenic
under normal circumstances, when their natural host is in a good
health, like the rabies virus, coexists with many wild mammals but
3
can cause fatal disease in humans.
The above mentioned 'balanced pathogenicity' is sometimes
explained as the outcome of selective pressures acting upon a
relationship over a long period of evolutionary time.
The 'balanced pathogenicity' may reflect selection of an increased
level of genetically determined resistance in the host population
and decreased pathogenicity in the parasite (as has happened with
myxomatosis in rabbits).
Alternatively, it may be the evolutionary norm, and 'unbalanced
pathogenicity' may simply be the consequence of organisms
becoming established in 'unnatural' (new) hosts.
Like the other categories of symbiosis, parasitism is impossible to
define exclusively except in the context of clear cut and highly
pathogenic organisms.
The belief (opinion) that 'harmfulness' is a necessary characteristic
of a parasite is difficult to sustain (maintain) in any broader (wider,
extensive) view.
Pathogenicity of Microorganisms
Characteristics and aspects
Pathogenic microorganism is defined as the one that is capable of causing
disease. Every infection is a race (contest of speed) between the capacity of
the microorganism to multiply, spread and cause disease from one side
and the ability of the host to control and finally terminate the infection
from the other side.
4
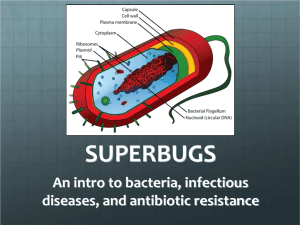
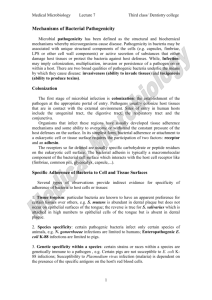
Bacterial pathogenesis
The pathogenesis of bacterial infection includes initiation of the
infectious process and the mechanisms that lead to the development of
signs and symptoms of disease. Characteristics of bacteria that are
pathogens include:
A. Transmissibility, B. Adherence to host cells, C. Invasion of host cells
and tissues, D. Toxigenicity, and E. Ability to evade the host's immune
system.
There are several important stages in the infectious process in order for
microorganism to establish its self as pathogen:
1. Entry into the host with evasion (avoidance) of host defenses.
3. Propagation (reproduction, generation) of microorganism.
4. Damage of the host tissues by bacterial toxins or an inflammatory
response of the host.
5. Evasion by microorganism the secondary responses.
Virulence: the term virulence and pathogenicity is exchangeable (similar)
and can be quantified by how many organisms (microorganisms) are
required to cause disease in 50% of exposed to infection by pathogen lab
animals {(ID50, where I = infection and D = dose)} or {(LD50, where L=
lethal and D = dose )} when 50% of animals were killed after inoculation.
5
I. Bacterial Virulence Factors
Many factors determine bacterial virulence, or ability to cause infection
and disease.
A. Entry into the host
The first step in the infectious process is the entry of
microorganism to the host using various ports: a. Respiratory tract,
b. Gastrointestinal tract, c. Urogenital tract, d. Cut, burned or
punctured skin.
Once the entry is happened, the pathogen must overcome different
host defenses before establishment of disease.
Host defenses may include a. Phagocytosis, b. Acidic
environments of the stomach, vagina, urinary tract as well as c.
Various hydrolytic and proteolytic enzymes found in saliva,
stomach and small intestine.
Bacteria that have an outer polysaccharide capsule, like
Streptococcus pneumoniae and Neisseria meningitidis, have a
better chance to survive these primary host defenses.
B. Adherence factors
Once bacteria enter the body of the host, they must adhere to cells
of surface of the target tissue and in case of their failure, they
would be swept away by mucus and other fluids that bathe (cover)
the tissue surface.
Adherence is only one step in the infectious process, then followed
by development of micro colonies and subsequent steps in the
6
pathogenesis of infection.
The interactions between bacteria and tissue cell surfaces, in the
adhesion process, are complex. Several factors play important
roles: surface hydrophobicity and net surface charge, binding
molecules on bacteria (ligands), and host cell receptor interactions.
Bacteria and host cells commonly have net negative surface
charges and, therefore, repulsive (driving away) electrostatic
forces.
The electrostatic forces are overcome by hydrophobic and other
more specific interactions between bacteria and host cells. In
general, the more hydrophobic the bacterial cell surface, the greater
the adherence to the host cell.
Different strains of bacteria within a species may vary widely in
their hydrophobic surface properties and ability to adhere to host
cells.
Bacteria also have specific surface molecules that interact with host
cells. Many bacteria have pili, hair-like structures as in E. coli and
fimbriae as in group A streptococci. These appendages extend
from the bacterial cell surface and help mediating adherence of the
bacteria to host cell surfaces.
E coli organisms that cause urinary tract infections commonly do
not have D-mannose-mediated adherence but have P-pili, which
attach to a portion of the P blood group antigen, the minimal
specifically recognized structure is the disaccharide Galα1-4Gal
sequence of globoseries glycolipids.
The E coli that cause diarrheal diseases by pilus-mediated
adherence to intestinal epithelial cells, therefore pili and specific
7
molecular mechanisms of adherence appear to be different
depending upon the form of the E coli that induce the diarrhea.
Importance of adhesion can be explained by the pathogenesis of
Neisseria gonorrhoeae in which strains of this bacteria that lack
pili are not pathogenic.
C. Invasion of host cells and tissues
Invasive bacteria are those that can enter host cells or penetrate
mucosal surfaces, spreading from the initial site of infection.
"Invasion" is the term commonly used to describe the entry of
bacteria into host cells, implying (indirectly suggest) an active role
for the organisms and a passive role for the host cells.
In many infections, the bacteria produce virulence factors that
influence the host cells, causing them to engulf (ingest) the bacteria.
The host cells play a very active role in the process.
Invasiveness is facilitated by several bacterial enzymes, that
degrade components of the extracellular matrix, providing the
bacteria with easier access to host cell surfaces.
Invasion is followed by inflammation, which can be either
pyogenic (involving pus formation) or granulomatous (having
nodular inflammatory lesions) depending on the organism.
D. Bacterial toxins
Bacteria cause disease by producing two types of toxins, the
exotoxins and the endotoxins.
Exotoxins are proteins secreted by both gram-positive and gramnegative bacteria.
Endotoxins are not secreted lipopolysaccharides. They are integral
8
(part of a whole) components of the cell walls of gram-negative
bacteria.
Exotoxins: These include some of the most poisonous substances known.
Exotoxin proteins generally have two polypeptides components,
one is responsible for binding the protein to the host cell, and one
is responsible for the toxic effect.
In several cases, the precise (exact) target for the toxin has been
identified.
Most toxins are rapidly inactivated by moderate heating (60 ᵒC).
Toxin treatment with diluted formaldehyde destroys the toxic
activity of most exotoxins, but does not affect their antigenicity.
Exotoxins are, in many cases, encoded by genes carried on
plasmids or temperate (repress, suppress) bacteriophages.
Corynebacterium diphtheria that carry this phage are pathogenic,
whereas those that lack the phage are nonpathogenic.
Diphtheria toxin is an enzyme that blocks protein synthesis.
Endotoxins:
Endotoxins are heat-stable, lipopolysaccharides (LPS) components
of the outer membranes of gram-negative, but not gram-positive
bacteria.
They are released into the host's circulation following bacterial
lysis.
LPS consist of polysaccharide O (somatic antigen), which
protrudes (stick out, project ) from the exterior cell surface, then a
core polysaccharide, and a lipid component called lipid A that
faces the cell interior.
The lipid A moiety (part) is responsible for the toxicity of the LPS
molecule.
The main physiologic effects of LPS endotoxins are fever, shock,
hypotension (low blood pressure) and thrombosis (coagulation of the
blood in the heart or a blood vessel) (septic shock).
Gram-positive can cause shock-syndrome by their cell wall
peptidoglycan, which is less severe than LPS of gram-negative due
9
to a big chemical difference between them, therefore they are not
considered to be endotoxins.
II. Antigenic switching
A successful pathogen must evade the host's immune system that
recognize bacterial surface antigens. In this manner, the expressed surface
antigen can assume (suppose) many different antigenic structures.
Capability of pathogen to avoid attack by immune system is to
change its own surface antigens, antigenic switching.
One of the antigenic switching mechanisms is called "phase
variation", which is a genetically reversible phenomenon of certain
bacteria to turn on or turn off the expression of genes coding for
surface antigens.
A second mechanism in this manner, called "antigenic variation",
which involves the modification of the gene for an expressed
surface antigen by genetic recombination (creation of new
combinations of genes) with one of many variable unexpressed DNA
sequences.
III. Characterization of the pathogen
An apportunistic pathogen is an organism that is unable to cause
disease in healthy individuals, but can infect people whose
defenses have been impaired.
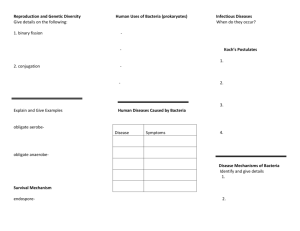
According to the KOCH'S CRITERIA (Koch's postulates) :
1. The microorganism must always be found in similarly diseased
animals but not in healthy ones.
2. The microorganism must be isolated from diseased animal and
grow in pure culture.
3. The isolated microorganism must cause the original disease
when inoculated into a susceptible animal.
4.The microorganism can be reisolated from the experimentally
10
infected animal.
IV. Infection in human populations
Bacterial disease may be communicable from person-to-person or
noncommunicable. Cholera is highly communicable, because the
causative agent (pathogen) is easily spread, whereas botulinum
exotoxin is noncommunicable, because only those people who
ingest the toxin are affected.
Highly communicable diseases like cholera are called contagious,
which means the frequency and tendency of localized epidemics
of disease is higher than normal.
When an epidemic becomes worldwide is called pandemic.
A nosocomial infection is any infection acquired while in
hospital
Presence of a large number of sick people together under one roof
has many advantages, but some disadvantages, notably the easier
transmission of infection from one person to another.
Hospital infection-also known as nosocomial infection-is defined
as any infection acquired while in hospital (e.g. occurring 48 hours
or more after admission and up to 48 hours after discharge).
Most of these infections become obvious while the patient is in
hospital, but some (as many as 50% of postoperative wound
infections) are not recognized until after the patient has been
discharged (leave the hospital).
Earlier discharges, encouraged to reduce costs, contribute to these
unrecognized infections, although a shorter preoperative stay
reduces the chance of acquiring hospital pathogens.
11
Hospital infection may be acquired from:
An exogenous source (exp. from another patient-cross-infection-or
from the environment).
An endogenous source (exp. another site within the patient-self- or
auto-infection).
An infection that is incubating in a patient when they are admitted
into hospital is not a hospital infection. However, communityacquired infections brought into hospital by the patient may
subsequently become hospital infections for other patients and
hospital staff.
Common hospital acquired infections
Urinary tract infections are the most common hospital-acquired infections
The infections most commonly acquired in hospitals are:
Surgical wound infection,
Respiratory tract infection,
Urinary tract infection (UTI),
Bacteremia (bacteria in the blood).
Each may be acquired from an exogenous or endogenous source,
and even the 'self-source' may be derived from outside by the
patient who becomes colonized with pathogens during his or her
stay in hospital.
Bacteremia may arise from a variety of sources and may be
primary-due to the direct introduction of organisms into the blood
from, for example, contaminated intravenous fluids.
Secondary to a focus of infection already present in the body (exp.
UTI).
Other infections that may cause outbreaks in the hospital setting
include gastroenteritis and hepatitis.
12
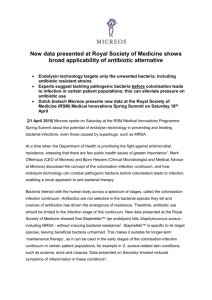
Strategies for control
by the use of drugs (chemotherapy),
by vaccines (immunization),
by improving the environment (e.g. better sanitation, nutrition).
* In general, chemotherapy is used to control infectious diseases in
individuals, whereas immunization and environmental improvements are
used for control in populations.
* Understanding the ways in which these diseases arise, spread and can
be controlled requires detailed epidemiologic studies to provide an
accurate basis for assessment of risks and for planning intervention.
* These studies are based on knowledge of the infectious agents and their
patterns of association with their hosts, but require the collection and
analysis of data, in conjunction with the use of mathematical models, to
produce useful pictures of disease transmission and control.
* When the causal links between a clinical condition and an infectious
agent or its mode of transmission are unknown, epidemiologic
investigations can establish this link and thus determine appropriate
control strategies.
Definitions
Adherence (adhesion, attachment): The process by which
bacteria stick to the surfaces of host cells. Once bacteria have
entered the body, adherence is a major initial step in the infection
process. The terms adherence, adhesion, and attachment are often
used interchangeably (exchangeable).
13
Carrier: A person or animal with asymptomatic infection that can
be transmitted to another susceptible person or animal.
Infection: Multiplication of an infectious agent within the body.
Multiplication of the bacteria that are part of the normal flora of the
gastrointestinal tract, skin, vagina and other part of body, is
generally not considered an infection, on the other hand,
multiplication of pathogenic bacteria (exp. Salmonella species)
even if the person is asymptomatic is deemed (believed) an
infection.
Invasion: The process whereby bacteria, animal parasites, fungi,
and viruses enter host cells or tissues and spread in the body.
Nonpathogen: A microorganism that does not cause disease, may
be part of the normal flora.
Opportunistic pathogen: An agent capable of causing disease
only when the host's resistance is impaired (like when the patient is
"immunocompromised").
Pathogen: A microorganism capable of causing disease.
Pathogenicity: The ability of an infectious agent to cause disease.
Toxigenicity: The ability of a microorganism to produce a toxin
that contributes to the development of disease.
Virulence: The quantitative ability of an agent to cause disease.
Virulent agents cause disease when introduced into the host in
small numbers. Virulence involves adherence, invasion, and
toxigenicity .
14