Pathology - Collegium Medicum UMK
advertisement

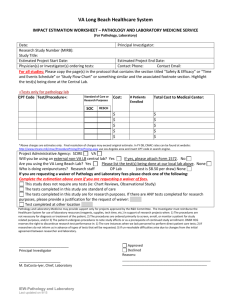
PATHOLOGY Pathology is a science which combines the basis fields of medicine and clinical medicine. Pathology is a study of causes, mechanisms, course and consequences of the disease. The pathology is classically divided into general and organ pathology. Proper clinical diagnosis is based on clear understanding etiology, pathogenesis, morphological and functional changes in specific diseases processes. The pathology course includes lectures, and tutorials. During tutorials and lectures cell injury and cell death, inflammations, hemodynamic disorders, neoplasms, genetic and environmental diseases will be discussed first. Next the changes of diseases in particular systems will be discussed. Each of the pathology issues will be illustrated by guided and self-performed microscopic slides studies. After 4 week pathology course students are obligated to pass written test exam to obtain a credit for whole pathology course. TEACHERS: Prof. dr hab. Andrzej Marszałek Dr Łukasz Szylberg lek. Joanna Maciejewska lek. Natalia Skoczylas-Makowska CONTACT: natalia.makowska@vp.pl asia_bielsk@wp.pl l.szylberg@cm.umk.pl magdaw@cm.umk.pl SYLABUS I. II. III. IV. V. VI. VII. Name of the unit offering the course: Department of Clinical Pathology Head of the unit/ course coordinator: Prof. dr hab. Andrzej Marszałek 3rd year, number of hours: 160 Form of classes: lectures :64, tutorials: 96 Form of crediting: Exam, Number of ECTS points: 13 Aim of the course: After completing the pathology course student has to know causes, pathomechanisms, clinical course and consequences of the disease and understand morphological and functional changes in specific diseases processes. IX. Topics of tutorials (THE SCHEDULE FROM PATHOMORPHOLOGY INCLUDING A LIST OF SLIDES) X. Topics of lectures IX. THE SCHEDULE FROM PATHOMORPHOLOGY INCLUDING A LIST OF SLIDES. I WEEK 1. Monday: Introduce to pathology + autopsy Łukasz Szylberg MD, PhD Topics: Legal issue related to autopsy and to the pathologist. Rules of writing a pathological diagnosis. Audiovisual presentation of autopsy techniques Autopsy demonstration with discussion of autopsy techiques. Signs of death. Autopsy techniques for haed, neck, chest, abdominal and pelvis examination. Autopsy in special cases – e.g. emphysema, embolisms, poisoning etc. Practical performed by students. Neonatal autopsy techniques 2. Tusday: a) Adaptive changes. Natalia Skoczylas-Makowska, MD Topics to prapare: Atrophy, hyperplasia, hypertrophy, metaplasia – definition, division, causes, examples Dystrophic and metastatic calcification Fatty change and cellular swelling Necrosis – definition, types, morphology Topics of tutorials: Adaptive changes Intracellular accumulations Pathologic calcification Slides: 1. Brown atrophy of the heart atrophia fusca myocardii 2. Cardiac muscle hypertrophy (hypertrophia musculi cordis) 3. Endometrial hyperplasia (hyperplasia glandularis endometrii) 4. Vacuolar degeneration (hydropic change) of hepatocytes (degeneratio parenchymatosa hepatis) 5. Epidermal hyperkaratosis (hyperkeratosis epidermis) 6. Corpus albicans ovarii 7. Liquefactive necrosis (brain encephalomalacia) (necrosis colliquativa; na przykładzie rozmiękania mózgu [encephalomalatio cerebri]) 8. Coagulative necrosis (liver and lung tuberculosis) (necrosis coagulativa; na przykładzie: gruźlicy płuc i wątroby [tuberculosis pulmonum et hepatis]) b) Hemodynamic disorders. Łukasz Szylberg, MD, PhD Topics to prapare: Pulmonary thrombosis Infarction pale and red Hyperemia passive Topics of tutorials: Edema 146 138,150 085, 085a, 085c, 085d 134 135 143 152 026 Slides: 1. 2. 3. 4. 5. 6. 7. 8. 9. Hyperemia Embolism Thrombosis Hemmorhage Hemorrhagic cerebral infarction (focus haemorrhagicum cerebri) Hemosiderosis whitish ovarian body (haemosisderosis corporis albicantis ovarii) Passive congestion of liver (hyperaemia passiva hepatis) Chronic venous stasis in the lungs (venostasis chronica pulmonum) Pale infarction of kidney (infarctus pallidus renis) Hemorrhagic intestinal infartion (infarctus haemorrhagicus intestini) Adhering thrombus (thrombosis parietalis) Recanalization of thrombus (thrombosis recanalisatus) Pulmonary edema 127, 133 154 + żelazo 155 153, 157 059 160 097, 193 233 062/256 3. Wednesday: Chronic and acute inflammation. Joanna Maciejewska, MD Topics to prapare: Definition of acute and chronic inflammation Characteristics of cells and processes with their participation in acute and chronic inflammation. Outcome of acute inflammation systemic and local symptoms of acute inflammation Granulomatous inflammation - definition Types of granulomas Topics of tutorials: Morphology of inflammation Vascular changes in acute inflammation Lymphatic vessels and lymph nodes in acute inflammation Pathogenesis, morphology and clinical changes in syphilis and tuberculosis Slides: 1. 2. 3. 4. Lymphnode sinus histiocytosis (histiocytosis lymphonoduli) Nonspecyfic lymphadenitis Lymphonodulitis reactiva Fibrinoid necrosis on the example of chronic peptic ulcer (degeneratio fibrinoidea; na przykładzie przewlekłego wrzodu trawiennego żołądka [ulcus chronicum pepticum ventriculi]) Lung abscess 188 226 144 034 5. 6. 7. 8. 9. 10. 11. 12. 13. (abscessus pulmonis) Serum acute appendicitis, appendicitis with lymphoid follicles hyperplasia, suppurative appendicitis, gangrenous appendicitis (appendicitis; [acuta serosa] [follicularis], [purulenta], [phlegmonosa], [gangrenosa],[obliterativa]) meningitis purulenta Miliary tuberculosis of lung (tuberculosis miliaris pulmonis) Adrenal tuberculosis (tuberculosis glandulae suprarenalis) Tuberculous meningitis (meningitis tuberculosa) Lymph node sarcoidosis (sarcoidosis lymphonoduli) Leprosy (lepra) Inflammatory granulation tissue, foreign body reaction (granulatio, granuloma) Scarring after myocardial infarction Cicatrisatio post infarctum myocardii) 262, 027, 266, 268 167 025 151 102 111 229 069 4. Thursday: Diseases of immunity. Natalia Skoczylas-Makowska, MD Topics to prapare: Organ changes in systemic lupus erythematosus, rheumatoid arthritis, amyloidosis. Polyarteritis nodosa Topics of tutorials: Systemic lupus erythematosus Scleroderma Rheumatoid arthritis Inflammatory myopathies Sjogren syndrome Vasculitides Slides: 1. 2. 3. 4. Renal amyloidosis (amyloidosis renis) Rheumatoid nodule (nodulus rheumathoideus) Rheumatoid arthritis (ang. rheumatoid artritis) Periarteritis nodosa (polyarteritis nodosa) 077 + amyloid 174 082 124 5. Sclerodermia (scleroderma localisata) 6. Lupus erythematosus – renal changes (lupus erythematosus) Helictotrichon (oxyuriasis) 7. 173, 196 Włókna sprężyste 033, PAS 276 5. Friday: Neoplasms. Joanna Maciejewska, MD Topics to prepare: Morphological and clinical characteristic of benign and malignant neoplasms. Precancerous lesions. Metaplasia.Dysplasia. Carcinoma in situ. Microinvasion and early cancer. Pareneoplastic syndromes and kachexia Grading i stading. Tumor markers. Topics of tutorials: Abnormal differentiation and maturation of tissues. Intraepithelial neoplasia. Benign epithelial neoplasms Malignant and locally malignant tumors. Epidemiology and diagnostic of neoplasms. Clinical features of neoplasms. Slides: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Epidermal actinic keratoses (keratosis senilis) Lichen sclerosus; (kraurosis) Benign mammary dysplasia (mastopathia fibroso-cystica; dysplasia benigna mammae) Seborrheic skin whart (verruca seborrhoica) Eversion in the cylindrical epithelium of the vaginal cervix, glandular erosion of the vaginal cervix (ectropion) Neoplasia intraepithelialis cervicalis CINI/ LSIL (neoplasia intraepithelialis cervicalis; ang. CIN – cervical intraepithelial neoplasia) CIN I/ LSIL Neoplasia intraepithelialis cervicalis CIN III/HSIL 177 Bowen’diseases (morbus Boweni) Basal cell carcinoma of the skin (carcinoma basocellulare cutis) Squamous cell carcionoma of the skin (carcinoma planoepitheliale/ carcinoma sinocellulare cutis) Urothelial carcinoma of the bladder (carcinoma urotheliale) 166 168 050, 179 243 237 178 176 110 022 186 12. 13. 14. 15. 16. 17. Colorectal adenocarcinoma (adenocarcinoma coli) Lipoma (lipoma) Liposarcoma (liposarcoma) Astrocytoma (astrocytoma) Glioblastoma multiforme (glioblastoma multiforme) Sarcoma synoviale – lung metastasis (sarcoma synoviale) 279 195 049 053, 244 204, 260 214 II WEEK 1. Monday : Pathology of the gastrointestinal tract. Łukasz Szylberg.MD, PhD Topics to prapare: Gastritis. Peptic chronic ulcer. Colon cancer – morphologic and clinical features Topics of tutorials: Congenital anomalies of gastrointestinal tract Esophagitis and tumors of esophagus Inflammation of gastrointestinal tract Peptic ulcer disease Neoplasms of stomach Intestinal vascular disease Diverticular disease Intestinal obstruction Tumors of the large and small intestine Slides: 1. 2. 3. 4. Ulcerative colitis (colitis ulcerosa) Crohn disease (morbus Lesniowski-Crohn; także: ileitis terminali, ang: Crohn disease) Celiac disease (celiakia) Adenomatous polyp of the sigmoid colon (polypus adenomatosus) 003, 008 228 165 042 5. 6. 7. 8. 9. 10. Gastric adenocarcionoma (adenocarcinoma ventriculi) Mucous degeneration on the example of mucinous adenocarcionoma Carcinoid of the appendix (carcinoidum appendicis) Colorectal leyomyosarcoma (leyomyosarcoma coli) Hemorrhagic intestinal infarction (infractus haemorrhagicus intestini) Barret esophagus 041 068 + śluz 270 006 160 283 2. Tusday: Pathology of the liver, bile ducts and pancreas. Łukasz Szylberg, MD, PhD Topics to prepare: Patterns of hepatic injury Acute and chronic viral hepatitis Drug and toxin-induced liver disease. Cirrhosis. Hemochromatosis Primary sclerosing choalngitis Circulatory disorders Malignant tumors of liver Cholelithiasis Acute pancreatitis Topics of tutorials: Infectieous disorders Autoimmune hapatitis Alcoholic liver disease. Insufficiency of liver. Impaired blood flow into and through the liver. Metabolic liver diseases Cholestasis and disorders of the intrahepatic bile ducts Nodules and tumors of liver Fine and core needle biopsy Cholecystitis Tumors of the gallbladder Pancreatitis Neoplasms of pancreas Slides: 1. 2. 3. 4. Intrahepatic cholestasis (stasis bilis intrahepatica) Viral hepatitis (hepatitis viralis) Alcoholic cirrhosis (cirrhosis hepatis alcoholica) Postinflammatory cirrhosis (cirrhosis hepatis postinfectiosa) 148 227 105, Masson, vanGiesson 162 5. 6. 7. 8. Centrilobular necrosis (necrosis centrolobularis hepatis) Liver cancer (carcinoma hepatocellulare) Cholecystitis (cholecystits) Gallbladder cancer infiltrating the liver 070 277 280 269 3 Wensday.: Pathology of the respiratory tract part I. Joanna Maciejewska, MD Topics to prapare: Pneumonia – morphology and clinical features Pulmonary vascular diseases Chronic obturative disorders of lung. Pathology changes in pleura Topics of tutorials: Etiology, pathogenesis, division and morphology mouth, throat, nose and trachea mucosa inflammations Bronchiectases Pneumonia – etiology, pathogenesis, morphology Pneumoconioses Obturative and restrictive disease of lung Cor pulmonale Slides: 1. 2. 3. 4. 5. 6. 7. 8. Pulmonary artery embolism (embolia thrombotica ramorum arteriae pulmonalis) Hemorrhagic lung infarction (infarctus haemorrhagicus pulmonis) Lobar pneumonia (pneumonia lobaris) Bronchopneumonia (bronchopneumonia) Chronic bronchitis (bronchitis chronica) Fungal pulmonary infection (pneumonia mycotica) Mixed salivary gland tumor (tumor mixtus; edenoma pleomorphum) Pnemoconioses (pneumoconioses) 4. Thursday: Pathology of the respiratory tract part II. Joanna Maciejewska, MD Topics to prapare: Lung cancer Cancer of larynx Malignant tumors of the salivary glands Nosopharyngeal cancer Topics of tutorials: 156 060 198 067, 058 076 115 031 272 Precancerous lesions and neoplasms of respiratory tract (including nasal cavity, larynx, trachea, bronchus, pleura) Slides: 1. 2. 3. 4. 5. Squamous cell lung cancer (carcinoma planoepitheliale pulmonis) Lung adenocarcinoma (adenocarcinoma pulmonis) Lung small cell carcionoma (carcinoma microcellulare pulmonis) Laryngeal squamous cell carcinoma (carcinoma planoepitheliale laryngis) Bronchial carcinoid and carcinoid of the appendix. (carcinoidum bronchit et appendicis) (barw.chromograniną A) 245 046 040 210 090, 249 5 Friday.: Childhood and infancy diseases. Łukasz Szylberg, MD Topics to prapare: Neonatal respiratory distress syndrome Fetal hydrops Necrotizing enterocolitis Wilms tumor Neuroblastoma Rethinoblastoma Rhabdomyosarcoma Topics of tutorials: Congenital anomalies Respiratory distress syndrome Tumors of infancy and childhood Prasotic infections Slides: 1. 2. 3. 4. 5. Testicular hypoplasia (hypoplasia testis) Neonatal respriratory distress syndrome (membranae hyalinae pulmonum) Trichinosis (trichinellosis) Echonococcosis (echinococcosis cystica pulmonum) Cerebral toxoplasmosis 145 159 164 106 139, PAS toxoplasmosis cerebri) Craniopharyngioma (craniopharyngeoma) 7. Retinoblastoma (retinoblastoma) !! TEST (exercises 1-10 and lectures 1,2) 6. 208 202 III WEEK 1. Monday : Pathology of heart and vascular diseases Natalia Skoczylas-Makowska, MD Topics to prapare: Morphology of infarction Hypertensive heart disease Bacterial endocarditis Topics of tutorials: Atherosclerosis Aneurysms and varicoses Ischemic heart disease Myocardial infarction Right sided heart failure Endocarditis Slides 1. Arteriosclerosis (arterioclerosis centralis) 2. Arteriosclerosis of renal arteries (renes arteriosclerotici) 3. Myocardial infarction (infractus myocardii) 4. Myocardial scarring (cicatrisatio postinfractosa myocardii) 5. Heart valve endocarditis (endocarditis valvularis) 6. Fibrinous pericarditis (pericarditis fibrinoidea) 7. Acute myocarditis (myocarditis acuta) 8. Hemorrhoids (varices haemorrhoidales ani) 9. Hemangioma (haemangioma) 2. Tusday : Pathology of the urinary tract. Natalia Skoczylas-Makowska, MD Topics to prapare: Nephritic syndrome Acute and chronić pyelonephritis Vascular lesions in benign and malignant hypertension Urolithiasis Hydronephrosis Renal cel carcinoma 128, 131, 132 212 +PAS 255 069 216 096 163, 250 251 099 Urothelial carcinoma of bladder Topics of tutorials: Nephritic syndrome and associated glomerulonephritis Tubulointestinal nephritis induced by grugs and toxins Nefropatia poanalgetyczna. Acute tubular necrosis Diseases of blood vessels Cystic diseases of kidney Tumors of the kidney and urinary tract Slides: 1. 2. 3. 4. 5. 6. 7. Changes in diebetic kidney (degeneratio glycogenica renum) glomerulosclerosis intercapillaris Glomerular sclerosis (glomerulonephritis sclerosans) Pyelonephritis (pyelonephritis) Renal cell carcinoma (carcinoma clarocellulare renis) Urothelial carcinoma of the bladder (carcinoma urotheliale) Kidney transplant – rejection (ang. Kidney rejection) 092, glikogen 030, PAS 169, PAS 199, PAS 002, 247, PAS 186 273, PAS 3. Wensday: Hemopathology. Joanna Maciejewska, MD Topics to prapare: Reactive lymphadenitis Definition of lymphoma and leukemia Clinical manifestations of proliferative diseases of the lymphatic system Hodgkin lymphoma – definition, types, morphology, clinical manifestation Topics of tutorials: Non-neoplastic diseases of lymphatic system Hematological malignances – leukemias and lymphomas Neoplasms of histiocytes Slides: 1. 2. 3. 4. 5. 6. 7. 8. acute myelogenous leukemia; AML Lymphoma (lymphoma malignum) Hodgkin lymphoma, lymphocyte depletion type Hodgkin lymphoma, mixed cellularity type Hodgkin lymphoma, nodular sclerosis type Multiple myeloma (myeloma multiplex) Solitary myeloma- rib tumor (plasmocytoma; plasma cel myeloma) Disseminated Intravascular Coagulation DIC 063 180,183 220 089 007 055 231 211 (microangipatia thrombotica, ang. DIC) 4 Thursday.: Pathology of the endocrine system. Łukasz Szylberg, MD Topics to prapare: Graves diseases Hashimoto thyroiditis Neoplasms of the thyroid Pheochromocytoma Neuroblastoma Topics of tutorials: Morphological causes of hypothalamic-pituitary axis failure Morphological causes of failure of anterior and posterior lobe of the pituitary gland Nowotwory przedniego płata przysadki mózgowej Tumors of the anterior pituitary gland Parathyroid glands – hyperparathyroidism and hypoparathyroidism Thyroiditis Benign and malignant tumors of thyroid Acute and chronić adrenal insufficiency Adrenocortical neoplasms Neoplasms of adrenal medulla Morfologiczne przyczyny niewydolności części endokrynnej trzustki Diabetes - pathogenesis and morphology Pancreatic endocrine neoplasms Multiple endocrine neoplasia syndromes Slides: 1. 2. 3. 4. 5. 6. 7. Diffuse toxic goiter (degeneratio colloidea glandulae thyreoideae) Lymphocytic thyroiditis (thyreoiditis lymphocytaria) Invasive thyroiditis with fibrosis (struma Riedl) Thyroid adenoma (adenoma glandulae thyroideae) Papillary carcinoma of thyroid gland (carcinoma papillare glandulae thyroideae) Follicular carcinoma of thyroid gland (carcinoma folliculare glandulae thyroideae) Parathyroid carcinoma (carcinoma glandulae parathyroideae) 141 175 189 021 035 274 281 5. Friday: Pathology of the female reproductive system, part I Natalia Skoczylas-Makowska, MD Topics to prapare: Cervical neoplasia Risk factors in cervical carcinoma and carcinoma of the endometrium Carcinoma of the endometrium – pathogenesis, morphology and clinical aspects Leiomyomas of uterus Topics of tutorials: Neoplasms and inflammations of cervix Neoplasms and inflammations of uterus Endometriosis Dysfunctional endometrial bleeding Slides: 1. 2. 3. Invasive cervical cancer (carcinoma colli uteri) Uterine adenocarcionoma (adenocarcinoma endometrii) Purulent salpingitis (salipingitis purulenta) 101 010 038 IV WEEK 1. Monday: Pathology of the female reproductive system part II. Natalia Skoczylas-Makowska, MD Topics to prapare: Tumors of ovary epithelium Topics of tutorials: Inflammations and neoplasms of ovaries Inflammation and neoplasms of fallopian tube Slides: 1. 2. 3. Simple ovary cyst (cystis simplex ovarii) Ovary cystadenoma (cystadenocarcinoma ovarii) Ovary cystadenocarcinoma (cystadenoma ovarii) 2 Tuesday.: a) Pathology of the breast Łukasz Szylberg, MD, PhD Topics to prapare: Fibroadenoma – morphology and clinical featurs Phyllodes tumor - morphology and clinical featurs Histioklinika brodawczaka wewnątrzprzewodowego Breast cancer - morphology and clinical featurs Topics of tutorials: Inflammation of the breast Fibrocystic changes and prolifarative disease of breast Benign neoplasms of breast Malignant neoplasms in situ and infiltrate Stromal tunors 142 019 181 Slides: 1. 2. 3. Infiltrating ductal carcinoma of the breast (carcinoma ductale invasivum mammae) Mucinous carcinoma (carcinoma gelatinosum mammae) Intraductal papilloma of the breast (papilloma intraductale mammae) 048 219, śluz 224 b) Pathology of the skin. Natalia Skoczylas-Makowska, MD Topics to prapare: Basal cel carcinoma and squamous cel carcinoma of the skin – morphology and clinical features Melanocytic nevus Melanoma – morphology, pathogenesis and clinial characteristic Topics of tutorials: Neoplasms and tumor-like conditions of the skin Slides: 1. 2. Pigmented nevus (nevus pigmentosus) Melanoma malignum (melanoma malignum) 109 122, 057, 242 melanina 3 Wednesday.: Pathology of the male genital system. Natalia Skoczylas-Makowska, MD Topics to prapare: Neoplasms of testis – morphology and clinical features Prostate – adenocarcinoma and hyperplasia Topics of tutorials: Congenital anomalies and tumors of penis Congenital anomalies, vascular disturbances and tumors of testis Tumors of prostatę and prostatic benign enlargement Slides: 1. 2. 3. 4. Embryonal carcinoma of testis (carcinoma embrionalne testis) Seminoma (seminoma) (seminoma) Benign prostatic hyperplasia (hyperplasia nodularis prostatae) Prostate cancer (carcinoma prostatae) 051, 230 271 264 282 4. Thursday: Central nervous system Joanna Maciejewska, MD Topics to prapare: Bacterial meningitidis – causes, morphology Cerebral infarction Glial neoplasms of CNS Topics of tutorials: Trauma of central nervous system Edema and hernation Cerebrovascular diseases Infections Slides: 1. 2. 3. 4. 5. 6. 7. 8. Neurilemmoma, Schwannoma (neurilemmoma; Schwannoma) Malignant epipheral nerve sheat tumor 184 Oligodenroglioma (oligodenroglioma) Ependymomoma (ependymoma) Ganglion cells tumor (ganglioneurocytoma) 209 045 206 Meningioma (meningeoma) meningeoma malignum Medulloblastoma (medulloblastoma) 5. Friday: Classes in the laboratory. Sections. !! TEST (exercises 11-20 and lectures 3,4) Practical skill chart in Pathology Year of study ……… group ………. Academic year ……………………. After graduation Pathomorphology course student should: 235, Masson, vanGiesson 246 074 207 Type of practical skills date Signature of the authorized person Know the pathological terms and the knowledge of the basic mechanism of cell and tissue damage Describe the processes of regeneration of tissues and organs Recognize the pathological images of diseases of the immune system, genetic diseases, infectious and environmental disorders Define the clinical course of specific and nonspecific inflammation Know the etiology of hemodynamic, progressive and regressive changes, Recognize the pathological images of diseases of the immune system, genetic diseases, infectious and environmental disosders Recognize the pathological images of childhood diseases Know the issues of specific organ pathology, images of macro-and microscopic, and clinical course of pathological changes in various organs Replace and pathogens internal and external, modifiable and unmodifiable Replace the clinical forms of the most common diseases of particular organs and systems, metabolic diseases and disorders of water-electrolyte and acidbase Be able to link images of tissue and organ damage with symptoms of the diseases, a history and results of laboratory determinations and to describe the consequences of developing lesions to adjacent organs topographically Analyze the phenomenon of reactive, defensive and adaptive control and disturbance caused by an etiological factor Lectures: 1. Introduction to pathology. Pathology as a basis for therapeutic decisions. Apoptosis. Processes of cel aging. 2. Basics of immunopathology. Amyloidosis. Sarcoidosis. Comments 3. Molecular basis of carcinogenesis and correlation with morphological image. Morphological features of tumor-host reaction. 4. Morphological characteristics: thromboembolic disease, shock, and disseminated intravascular coagulation syndrome (DIC). Haemorrhagic diathesis. Anemia. 5. Pathology of genetically determined diseases. 6. Pathology of environmental diseases. 7. Pathology of infectious diseases (with discussion about hepatitis) 8. Pathology of heart and vascular part 1 (congenital heart disease, pericarditis, myocarditis, etiopathogenesis of atherosclerosis) 9. Pathology of the heart and blood vessels part 2 (vasculitis, neoplasms of the heart and blood vessels). 10. Pathology of interstitial lung diseases. Atypical pneumonia. 11. Pathology of oral cavity and esophagous 12. pathology of the upper respiratory tract. Tumors of salivary gland and larynx. 13. Non-neoplastic diseases of the lymphatic system. Pathology of the spleen and thymus. Classification system of proliferative diseases. 14. Test includes lectures 4-14 15. Idiopathic inflammatory bowel disease. 16. Pathology of glomerulonephritis - general issues. 17. Pathology of the vulva and vagina. Non-neoplastic gynecological pathology. 18. Pathology of pregnancy and placenta. Pathology of the fetus and newborn. 19. Pathology of the genitourinary system (malformations, inflammation, and cancer of penis). Pathology of sexually transmitted diseases. 20. The pathology of selected diseases of the breast (inflammatory, proliferative lesions of the breast, selected aspects of the molecular basis of breast cancer and their significance). 21. Pathology in daily practice - clinical cases. 22. Pathogenesis and histopathology of diabetes. 23. Pathology of endocrine system. Neuroendocrine tumors. 24. pathology of inflammatory skin diseases. Bullous skin disorders. 25. Pathology non-neoplastic diseases of the muscles, joints, and bones. 26. Aspects of soft tissue pathology 27. Malformations of the central nervous system. 28. The pathology of selected diseases of the nervous system (CNS viral infections, spongiform encephalopathies, primary myelin diseases and neurodegenerative diseases). 29. Pathology in daily practice - clinical cases. 30. Test includes lectures 16-30 RULES AND REGULATIONS A. Department of Clinical Pathomorphology Collegium Medicum Nicolaus Copernicus University, Skłodowskiej-Curie 9, 85-094 Bydgoszcz B. Head of the unit: Prof. Andrzej Marszałek MD, PhD C. Faculty of Medicine, Medical Program of Pathomorphology, 3rd year I. Form of study The pathomorphology course includes tutorials and lectures. Tutorials take place in classrooms in Pathomorphology Department for 4 weeks. Tutorial starts at 8:00 am to 11:45 am. Each groups has a specified date of tutorials, according to the Schedule. Tutorials and lectures are obligatory and performed according to topics described in Syllabus. Tutorials include knowledge testing, microscope exercises , autopsy practicals and laboratory exercises in histopathology lab section. During laboratory exercises, students learn how to collect samples from postoperative specimens, perform cytology tests, intraoperative frozen section and using special techniques (e.g. histochemistry, immunohistochemistry, etc.). During autopsy, students learn how to perform autopsy and understand particular case through discussion. II. Form of testing knowledge and evaluation of the course Students are evaluated in grading points system. There is no retakes of tests. Students’ achievements (scores points) are available online on the website (http://patologia.cm.umk.pl/eng.html) At the beginning of each tutorial, students write entrance test (open questions form) from topics specified in course schedule. Students do not have entrance test on the first tutorial. Students can get from 0 to 5 points for each tutorial test. After 2 weeks of the course (on tutorial number 10), students have partial test from the first part of tutorials (20 multiple choice test and 4 open questions). The material for the colloquium include tutorials from 2 to 10 and lectures number 1 and 2. After 4 weeks of the course, students have partial test from the second part of tutorials (20 multiple choice test and 4 open questions). The material for the colloquium include tutorials from 11 to 20 and lectures number 3 and 4. Students can get maximum 40 points for each colloquium. In presence of a teacher students have right to view their colloquiums, but only open questions part. This is possible during 1st week after announcement of the results. On lectures number 16 and 31, students have lecture tests (multiple choice test). The material for the lecture test include topics discussed on lectures. From each lecture test students can gain maximum 40 points. Reminder! Topics of tutorials which were not carried out because of rector’s or dean’s hours or an excused absence of student are valid on the colloquium and exam. III. Points system scale: Maximum points to gain from whole pathomorphology course is 245 (85 points for tutorials, 80 points for colloquiums and 80 points for lecture tests). To complete the pathomorphology course student needs to achieve in total 60% of points from all tutorials, colloquia and lecture tests (147 points out of 245 points). Student who achieve the minimum 60% of points from each tutorials‘ entrance tests and other tests and 80% of points in total from all tutorials, both colloquiums and both lecture tests ( 196 points out of 245 points ) will be released from the final exam. In the particular cases there is an opportunity to be released from the exam. The final decision about it and about tests or exam ranges is always made by the Head of the Department of Clinical Pathomorphology Collegium Medicum Nicolaus Copernicus University. In case of obtaining the unsatisfactory amount of points, in total (less than 60% needed to complete the course), student must write the additional test (multiple choice test + open questions) from the material of the whole course (tutorials + lectures). This have to be done before the start of the repeating exam session in September (only one chance will be set for all 3rd year students). It equals with failing 1st term of the exam. If student fails the additional test, one won’t be able to write the final exam, which means repeating the pathomorphology course in the next academic year. IV. Terms of crediting tutorials in case of excused absence or tutorials not passed from other reasons: If student is late for classes more than 15 minutes, one cannot participate in tutorial on that day and his absence is recorded. In case of the excused absence (sick – leave) student has to submit the medical certificate given by an academic physician, not later than 3 working days after the date of the tutorial an which he/she was absent. Maximum 7 working days after completed pathomophology course student who had excused absence on any tutorial is obliged to sign to that tutorial with other group. This can be done in the Secretary Office of our Department. Once student sets the date of missed tutorial it cannot be changed. Points achieved on entrance test on tutorials and on colloquium with another students’ group will be divided by 2. For students of the last group (who are not able to participate in tutorials with other group) there will be set one date to write all missing entrance tests after finished course. The unexcused absence on the tutorial is unacceptable and will be treated as non – classified tutorial. This means repeating the pathomorphology course in the next academic year. V. Form and terms of the examination: After completing the pathomorphology course students write the final exam. The exam lasts 120 minutes. It consists of two parts: multiple choice test (80 questions), which lasts 80 minutes and open questions (5 questions, 5 points for each), which lasts 40 minutes. Obtaining of an unsatisfactory note from the exam is possible in situations: 1) Failing the multiple choice test, 2) Passing the multiple choice test, but failing the open questions part. The date of the final exam is set for whole year in summer semester (the exact date will be decided by the Head of the Department). The absence during the exam should be justified at the Secretary Office of the Department on the exam day or, in the particular cases, during three working days after the exam. In case of excused absence on the exam, the first exam term is on the day of exam retake. The unexcused absence at the exam is equivalent with receiving an unsatisfactory grade. VI. The general and specific health and safety regulations required during the teaching process in Department of Pathology At the autopsy room, students wear additional protective aprons and protective footwear, in the case of performing autopsies wear additional protective clothing (shoes, glasses and disposable gowns) During laboratory exercises students watch the activities carried out under a glass fume hood With the appearance of the harmful chemicals at work is mandatory ventilation enabled. All medical devices must be operated in accordance with the applicable instructions, after explaining the principles of service and demonstrating by the teacher, and only under the strict supervision (especially for microtomes and cryostats) Due to contact with harmful chemicals: formaldehyde, xylene, acetone, absolute alcohol and 96% denatured alcohol, students are required to familiarize yourself with the characteristics of these harmful chemicals. Due to the threat of biological (HCV, HBV, HIV) all laboratory activities should be carried out in disposable protective gloves Because your safety and that of others, the work of reagents should be performed according to an instruction (instruction posted in the histopathology lab). All dangerous events ie. cuts, burns, etc. immediately must be reported to conducting classes On exercises students bring white coats, undertake to comply with health and safety regulations and medical confidentiality. Bydgoszcz, 1 September 2014 ……………………………………………………. signature of the Head of the Didactic …………………………………………………… representative of students ……………………………………………………… signature Director of the Centre for Medical Education in English