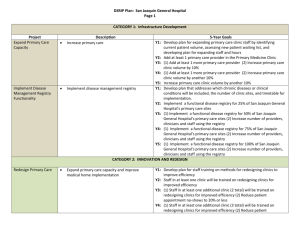
DSRIP Plan: Kern Medical Center Page CATEGORY 1
advertisement

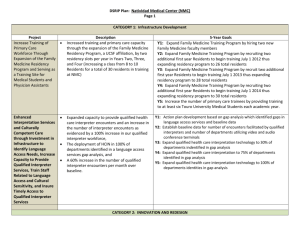
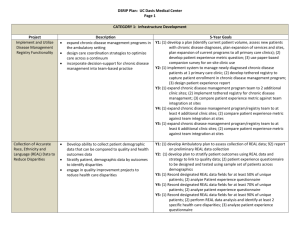
DSRIP Plan: Kern Medical Center Page 1 CATEGORY 1: Infrastructure Development Project Increase Primary Care Capacity Description Increase clinic hours to evenings and weekends Triage patient appointments to ensure that same day appointment slots are available for the most urgent patients Provide urgent appointments within 3 calendar days of request Y1: Y2: Y3: Y4: Y5: Implement and Utilize Disease Management Registry Functionality Design disease registry reporting plan and structure Train at least 10 champions on populating and using the registry functionality Expand the use of the registry to all areas of KMC with diabetic patients, including the primary care clinics, diabetic clinic, eye clinic, podiatry clinic and inpatient floors Y1: Y2: Y3: 5-Year Goals Develop a plan to expand the hours of primary care clinic to include evenings and weekends, as measured by (a) identification of current patient volume (b) Assessment of new patient waiting list (c) development of plan to expand the hours and (d) a plan to re-integrate urgent appointments into primary care clinics, including triaging patients so that patients can be seen by their primary care provider teams (1) Implement a nurse triage software system to assist nurses in determining the acuity of patients; (2) Hire and train at least 2 additional primary care nurses; (3) Provide 20% of patients that request urgent appointments, an appointment in the primary care clinic (instead of having to go to the ED or an urgent care clinic) within 3 calendar days of request (1) Expand the hours of the primary care clinic by at least 8 hours per week; (2) Provide 40% of patients that request urgent appointments, an appointment in the primary care clinic (instead of having to go to the ED or an urgent care clinic) within 3 calendar days of request (1) Expand the hours of the primary care clinic by at least 16 hours per week; (2) Patient access to primary care by reducing days to third nextavailable appointment within 30 calendar days Patient access to primary care by maintain 30 calendar days to third next-available appointment Demonstrate and design registry reporting ability to track and report on patient demographics, diagnoses, patients in need of services or not at goal and preventive care status (1) Expand registry report services to provide on-demand, operational and historical capabilities, inclusive of reports to care providers, managers and executives; (2) Conduct staff training for at least 10 staff on populating and using the registry (1) Spread registry functionality and training to inpatient floors and 6 outpatient clinic site that provide continuity of care for the diabetes population; (2)Enter patient data into the registry for at least 50% of patients with diabetes who are assigned to a KMC primary care clinic as their medical home Enhance Urgent Medical Advice Expand Specialty Care Capacity DSRIP Plan: Kern Medical Center Page 2 Y4: Enter patient data into the registry for at least 65% of patients with diabetes who are assigned to a KMC primary care clinic as their medical home Y5: Enter patient data into the registry for at least 65% of patients with diabetes who are assigned to a KMC primary care clinic as their medical home Y1: (1) Establish baseline and metrics of the 24/7 Nurse Line and Health Provide urgent medical advice so that patients Information Library. Includes at least the following metric baselines: (a) who need it can access it telephonically so that number of patients that access the nurse advice line and (b) number of avoidable utilization of urgent care and the ED patients that called the nurse advice line and reported intent to go to can be reduced the ED for non-emergency conditions; (3) Inform and educate 5,000 patients on the nurse advice line Y2: (1) Inform and educate an additional 5,000 (10,000 total) patients on the nurse advice line; (2) Increase the number of patients that accessed the nurse advice line by 10% over baseline established in Year 1; (3) Develop and distribute 5,000 patient-focused newsletters with proactive health information and reminders based on nurse advice line data / generated report identifying common areas addressed by the nurse advice line and topics searched for in the Health Information Library Y3: (1) Increase in the number of patients that accessed the nurse advice line by 25% over baseline established in Year 1; (2) Develop and distribute 10,000 patient-focused newsletters with proactive health information and reminders based on nurse advice line data / generated report identifying common areas addressed by the nurse advice line and topics searched for in the Health Information Library; (3) Increase the number of patients that called the nurse advice line with intent to go to the ED for non-emergency conditions who were redirected to non-ED resources by 10% over baseline established Year 1. Y4: (1) Increase in the number of patients that accessed the nurse advice line by 40% over baseline established in year 1; (2) Increase the number of patients that called the nurse advice line with intent to go to the ED for non-emergency conditions who were redirected to non-ED resources by 25% over baseline established Year 1. Y5: Increase the number of patients that called the nurse advice line with intent to go to the ED for non-emergency conditions who were redirected to non-ED resources by 25% over baseline established Year 1. Conduct a gap analysis to determine the specialty Y1: (1) Collect baseline data for wait times, backlog and now show rates in at least 8 specialty clinics; (2) Train 25 primary care providers and/or care needs of the community Enhance Interpretation Services and Culturally Competent Care DSRIP Plan: Kern Medical Center Page 3 staff on processes, guidelines and technology for referrals and Implement specialty care guidelines for the consultations; (3) Launch a musculoskeletal clinic highest demand specialties. Expand the number of current specialty providers Y2: (1) Conduct a specialty care gap analysis based on community need by assessing specialty clinic supply and demand, capacity and productivity; and/or specialty clinic hours for the highest need (2) Based on results of gap analysis, increase the number of specialist specialties to expand the supply of specialty care providers and/or clinic hours available for at least 2 high impact / most impacted medical specialties identified in the gap analysis; (3) Establish 3 specialty care guidelines for the high impact / most impacted medical specialties identified in the gap analysis Y3: (1) Establish 3 additional (6 total) specialty care guidelines for the high impact / most impacted medical specialties identified in the gap analysis; (2) Based on the results of gap analysis, increase the number of specialist providers and / or clinic hours available for at least 1 additional (3 total) high impact / most impacted medical specialties Y4: Based on results of gap analysis, increase the number of specialist providers and/or clinic hours available for at least 1 additional (4 total) high impact / most impacted medical specialties Y5: No milestones identified Y1: (1) Conduct an analysis to determine gaps in language access through a Identification of language access needs and/or survey to determine availability of interpretative equipment within the gaps in language access hospital and its outpatient clinics; (2) Expand capacity of qualified Addition of interpreter technology in inpatient healthcare interpretation workforce to 2 full time staff on HCIN; (3) and outpatient areas Establish baseline data of qualified interpreter encounters and number Expansion of certified qualified healthcare of video or audio conferencing points of access and/or units within interpreters by 50% inpatient and outpatient areas of the hospital. Increased training related to language access Y2: (1) Train 50% of direct patient care staff and/or providers in patient Training of staff “ champions” related to cultural areas to appropriately utilize health care interpreters (via video, phone competency / sensitivity or in person); (2) Develop and implement a training program for 10 Improving language access through an increase in “champions” to improve cultural competency; (3) Develop a plan to qualified healthcare encounters expand the interpreter technology to additional patient care areas within the hospital and its outpatient clinics; (4) Improve language access through a 5% increase from baseline in qualified interpreter encounters per month Y3: (1) Train 50% of direct patient care staff and/or providers in outpatient care areas to appropriately utilize health care interpreters (via video, phone, or in person; (2) Train 10 additional (20 total) designated champions / staff to improve cultural competency in outpatient areas; (3) Expand the interpreter technology (video or audio units) by 5% over baseline in year 1; (4) Improve language access through a 10% increase DSRIP Plan: Kern Medical Center Page 4 from baseline in qualified interpreter encounters per month. Y4: (1) Expand the interpreter technology (video or audio units) by 5% from previous year; (2) Improve language access through a 15% increase from baseline in qualified interpreter encounters per month Y5: (1) Improve language access through a 20% increase from baseline in qualified interpreter encounters per month CATEGORY 2: INNOVATION AND REDESIGN Expand Medical Homes Redesigning Primary Care 60% of new patients assigned to county medical homes that are contacted for their first patient visit within 120 days 75% of patients per year who need to receive a screening exam will be provide with reminders for Chlamydia screenings, cancer screenings and cholesterol screenings Increasing efficiency in clinics through the implementation of the patient visit redesign model Improving appointment access and convenience through patient-centered scheduling Improving scheduling and registration efficiency through the implementation of a practice management system Y1: Determine the appropriate panel size for primary care provider teams, potentially based on staff capacity, demographics and disease Y2: (1) Put in place policies and systems to enhance patient access to the medical home; (2) Assign at least 1,500 of eligible patients(where eligible is defined as eligible for Kern County’s LIHP program) to medical homes; (3) At least 40% of new patient assigned to medical homes will be contacted for their first patient visit within 120 days Y3: (1) Assign at least 2,500 of eligible patients(where eligible is defined as eligible for Kern County’s LIHP program) to medical homes; (2) At least 60% of new patient assigned to medical homes will be contacted for their first patient visit within 120 days Y4: Medical home provides population health management by identifying and reaching out to 50% of patients who need to be brought in for preventive and ongoing care Y5: Medical home provides population health management by identifying and reaching out to 75% of patients who need to be brought in for preventive and ongoing care Y1: Establish implementation plan and collect baseline data for patient appointment “no show” rates, days to third-next available appointment, and primary care visit cycle time Y2: (1) Implement patient visit redesign in primary care clinics; (2) Implement the patient-centered scheduling model in primary care clinics; (3) Implement practice management system Y3: (1) Reduce patient appointment no-show rate to 25%; (2) Reduce average visit cycle time for at least 2 primary care clinics to 60 minutes or less – without reducing the time a patient spends with his/her provider from baseline Year 1 Y4: (1) Reduce patient appointment no-show rates to 15%; (2) Reduce average visit cycle time for at least 2 additional (total 4) primary care clinics to 60 minutes or less – without reducing the time a patient spends with his/her provider from baseline Year 1 Integrate Physical and Behavioral Health Care Establish a Patient Care Navigation Program DSRIP Plan: Kern Medical Center Page 5 Y5: (1) Maintain patient appointment no-show rates at 15%; (2) Maintain average visit cycle time for primary care clinics to 60 minutes or less – without reducing the time a patient spends with his/her provider from baseline Year 1 Y1: (1) Train at least 15 primary care clinicians on primary care management 60% of patients discharged from an inpatient of behavioral health conditions; (2) Establish, implement and distribute psychiatric unit will be assigned a medical home referral guidelines for referring to the behavioral health care provider 45 % increase in patients who have access to behavioral health services amount those patients Y2: (1) Train at least 20 additional (35 total) primary care clinicians on primary care management of behavioral health conditions; (2) Co-locate identified as having a behavioral health need behavioral health and primary care, as measured by at least 2 behavioral health providers in primary care clinics; (3) Development of a tracing mechanism of referrals from primary care providers to on-site behavioral health professionals Y3: (1) Establish policies and procedures for a more robust inpatient discharge coordination with outpatient medical home providers for patients with behavioral health needs; (2)Increase from baseline 15% of patients with a behavioral health care need as identified by the primary care provider, who have access to behavioral health care (e.g. , visits with social workers, case managers or psychiatrists), as needed Y4: (1) Assign 40% of patients discharged from the inpatient psychiatric unit to a medical home; (2) Increase from baseline 25% of patients with a behavioral health care need as identified by the primary care provider, who have access to behavioral health care (e.g. visits with social workers, case managers or psychiatrists), as needed Y5: (1) Assign 60% of patients discharged from the inpatient psychiatric unit to a medical home; (2) Increase from baseline 45% of patients with a behavioral health care need as identified by the primary care provider, who have access to behavioral health care (e.g. visits with social workers, case managers or psychiatrists), as needed Y1: (1) Establish care navigation program to provide support to patient Implement a navigation program with 2 care populations who are at most risk of receiving disconnected and navigators for populations most at risk of fragmented care; (2) Provide care management and navigation services receiving disconnected care (patients with high to 60 targeted patients who are high utilizers of the Emergency past utilization of inpatient and emergency Department and/or inpatient services services) Y2: (1) Increase patient engagement by completing 5 patient engagement Implement an ED navigator program to educate initiatives; (2) Expand program to include ED navigator who educates patients on the importance of primary care and patients on the importance of primary care; connects patients to a new coordinate with other community clinics and the Primary Care Clinic and/or assists patient in getting following county primary clinics to provide appointment appointment with established PCP. slots for patients upon discharge from the ED DSRIP Plan: Kern Medical Center Page 6 Y3: (1) Provide navigation services to patients using ED for episodic care; (2) Measure ED visits and/or avoidable hospitalizations for patients enrolled in the care management / navigator program for high utilizers of the Emergency Department and/or inpatient services Y4: (1) Provide navigation services to patients using ED for episodic care; (2) Measure Ed visits and/or avoidable hospitalizations for patients enrolled in the care management / navigator program for high utilizers of the Emergency Department and/or inpatient services Y5: Provide a primary care appointment to 30% of the patients who need a follow-up primary care appointment after being discharged from the ED CATEGORY 4: URGENT IMPROVEMENT IN CARE Improve Severe Sepsis Detection and Management Central Line Associated Blood Stream Infection (CLABSI) Prevention implement Sepsis Management and Resuscitation Bundle Reduce avoidable harm or deaths due to severe sepsis to patients receiving inpatient services improve compliance with central line insertion bundle Reduce avoidable harm or deaths and costs of care due to central-line associated blood stream infections Y1: Implement a sepsis bundle data collection and reporting method Y2: (1) Complete a gap analysis of current processes re: sepsis; (2) Develop a formalized inter-professional protocol based on Sepsis Resuscitation Bundle; (3) Participate in Patient Safety First Collaborative of Sacramento and Central Valley Region for Sepsis; (4) Implement education on treatment of sepsis in both critical and non-critical patient care settings; (5) Report at least 6 months of data collection on Sepsis Resuscitation Bundle to SNI for baseline / benchmarks; (6) Report results to the state Y3: (1) achieve TBD% compliance with sepsis resuscitation bundle; (2) share data and practices with SNI for benchmarking across public hospitals; (3) Report results to the state Y4: (1) achieve TBD% compliance with sepsis resuscitation bundle; (2) share data and practices with SNI for benchmarking across public hospitals; (3) Report results to the state Y5: (1) achieve TBD% compliance with sepsis resuscitation bundle; (2) share data and practices with SNI for benchmarking across public hospitals; (3) Report results to the state Y1: Implement a central line insertion practice (CLIP) data collection and reporting method Y2: (1) Complete a gap analysis of current processes; (2) Develop a formalized inter-professional “Central-line Treatment Protocol”; (3) Participate in Patient Safety First Collaborative of Sacramento and Central Valley Region; (4) Implement education on treatment and management of CLIP; (5) Report at least 6 months of data collection on CLIP to SNI for baseline / benchmarks; (6) Report at least 6 months of data collection on CLABSI to SNI for baseline / benchmarks ; (7) Report Surgical Site Infection Hospital-acquired Pressure Ulcer (HAPU) Prevention Stroke Management Venous Thromboembolism (VTE) Prevention & Treatment DSRIP Plan: Kern Medical Center Page 7 CLIP results to state Y3: (1)achieve TBD% compliance with CLIP; (2) share data and practices with SNI; (3) report CLIP and CLABSI results to State Y4: (1) achieve TBD% compliance with CLIP; (2) reduce central line bloodstream infections by TBD%; (3) share data and practices with SNI; (4) report CLIP and CLABSI results to State Y5: (1) achieve TBD% compliance with CLIP; (2) reduce central line bloodstream infections by TBD%; (3) share data and practices with SNI; (4) report CLIP and CLABSI results to State Not a selected intervention by Kern Medical Center improve surgical site infection prevention Y1: Implement a HAPU data collection and reporting method Use a multi-disciplinary team approach to the Y2: (1) Share data, promising practices and findings with SNI to foster prevention of pressure ulcers using evidenceshared learning and benchmarking across the California public hospitals; based recommendations from the national (2) Report HAPU prevalence results to the state Pressure Ulcer Advisory Panel Y3: (1) Achieve HAPU prevalence of less than 5.5%: (2) Share data, promising practices and findings with SNI to foster shared learning and benchmarking across the California public hospitals; (3)Report HAPU prevalence to the state. Y4: (1) Achieve HAPU prevalence of less than 3.2%: (2) Share data, promising practices and findings with SNI to foster shared learning and benchmarking across the California public hospitals; (3)Report HAPU prevalence to the state. Y5: (1) Achieve HAPU prevalence of less than 1.1%: (2) Share data, promising practices and findings with SNI to foster shared learning and benchmarking across the California public hospitals; (3)Report HAPU prevalence to the state. Not a selected intervention by Kern Medical Center Prevent VTE by checking patients for risk of blood Y1: Implement a VTE data collection and reporting method Y2: (1) Complete a gap analysis of current processes for assessment and clots and taking appropriate steps to prevent prophylactic treatment of VTE; (2) Develop a formalized interthem professional VTE Prevention Treatment Protocol based on AHRQ; (3) Implement education on VTE prevention and treatment; (4) Report at least 6 months of data to SNI for baseline / benchmarks; (5) Report the 5 VTE process measures to the state Y3: (1) increase by TBD rate the rate of patients who received VTE prophylaxis or documentation why no VTE prophylaxis given the day of or day after hospital admission or surgery end date; (2) increase by TBD rate the rate of patients who received VTE prophylaxis or Falls with Injury Prevention DSRIP Plan: Kern Medical Center Page 8 documentation why no VTE prophylaxis given the day of or the daty after initial admission to ICU or surgery end date; (3) increase by TBD rate the rate of patients diagnosed with confirmed VTE who received and overlap of parenteral IV or subcu anticoagulation and warfarin therapy; (4) increase by TBD rate the rate of patients diagnosed with confirmed VTE who received IV UFH therapy dosages AND had platelet counts monitored using defined parameters; (5) increase by TBD rate the rate of patients diagnosed with confirmed VTE that are discharged to home, home care, court/law enforcement or home on hospital care on warfarin with written discharge instructions that address all criteria; (6) share data and findings with SNI; (7) report 5 VTE process measures to State Y4: Same as Y3 with adjusted rates Y5: Same as Y4 with adjusted rates Not a selected intervention by Kern Medical Center