the impact of haemoglobin on survival of haemodialysis patients
advertisement

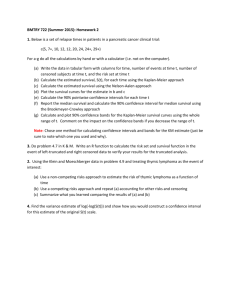
P170 THE IMPACT OF HAEMOGLOBIN ON SURVIVAL OF HAEMODIALYSIS PATIENTS McCrink, L.M. [1], Marshall, A.H. [1], Cairns, K.J. [1], Fogarty, D. [2] [1] Centre of Statistical Science & Operational Research, Queen’s University Belfast [2] Belfast Health and Social Care Trust, Belfast INTRODUCTION: With an ageing population, the analysis of chronic diseases is of increasing importance and predicting outcomes and treatment strategies is important for patients and limited resources. This research investigates the impact of haemoglobin (Hb) on haemodialysis (HD) patients’ survival whilst accounting for informative censoring due to dropout. The impact of various erythropoietin (EPO) drugs and a range of haematinic measurements, in particular Mean Corpuscular Volume (MCV) and Mean Corpuscular Haemoglobin Concentration (MCHC), on Hb levels are explored in this work. METHODS: To simultaneously analyse the factors that affect a HD patient’s Hb levels and the impact of this on their survival, a joint modelling approach to analyse longitudinal and survival data was utilised. A linear mixed effects model linked with a Cox PH model was used to represent the relationship between the repeated measurements of individuals and their survival respectively. In doing so, informative censoring due to dropout is taken into account to provide more precise results and thus interpretations. The data analysed in this research was obtained from the NI renal information service and contains 1,340 HD patients with a total of 27,113 observations (average 20 observations per patient) collected over a ten year period (2002-2011). RESULTS: This research highlights the large and significant impact between a patient’s MCV and MCHC levels and their Hb levels. An increase of 10fL in MCV levels is shown to increase Hb by 0.31g/dL whilst a 4g/dL increase in MCHC can cause Hb levels to increase by over 1g/dL. Aranesp is shown to be associated with significantly higher Hb levels on average than Epoetin Alfa (greater Hb by 0.23g/dL) or Epoetin Beta (greater Hb by 0.19g/dL). Patients with higher Hb levels three months after commencing HD tend to have better survival decreasing the hazard of death by 28% (Hazard Ratio=0.72). Greater decreases in Hb levels per year are shown to be detrimental to survival, with a 1g/dL decrease on average each year resulting in an increase in the hazard of death by 44% (Hazard Ratio=0.69). This research illustrates the benefits of joint models that enable individual-specific survival curves to be plotted, commencing at a patient’s last known measurement and changing dynamically over time with new patient information. CONCLUSION: This research presents evidence to encourage future research into anaemia in HD patients to investigate the impact of particular EPO drugs and a patient’s MCV and MCHC levels where patients with higher initial Hb levels and less change in Hb over time were shown to have better survival. Through such longitudinal techniques, individualised survival curves can be plotted that enable clinicians to predict the survival probabilities of patients as individuals instead of through analysis of population trends.