2013 - 2016 - National Programme for Family Planning & Primary
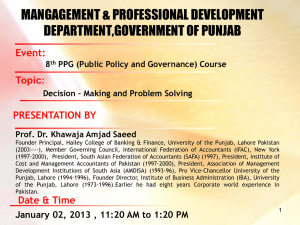
advertisement

PC-I PUNJAB Integrated Reproductive Maternal Newborn & Child Health (RMNCH) & Nutrition Program 2013 - 2016 Department of Health Government of the Punjab 1 ACRONYMS AIDS Acquired Immune Deficiency Syndrome ANC Ante Natal Care ARI Acute Respiratory Infection BHU Basic Health Unit CBR Crude Birth Rate CDD Control of Diarrhea Diseases CDR Crude Death Rate C-IMNCI Community based– Integrated Management of Newborn and Childhood Illnesses CMAM Community based Management of Acute Malnutrition CMT Community Midwifery Tutor CMW Community Midwife CPR Contraceptive Prevalence Rate DCHC District Community Health Council DCO District Coordinating Officer DEC District Evaluation Committee DFID Department for International Development DHQ District Headquarter Hospital DOH Department of Health DOTS Directly Observed Therapy Short Course DMU District Program Management Unit DSC District Steering Committee EDO Executive District Officer EDO (H) Executive District Officer (Health) EmONC Emergency Obstetric and Newborn Care ENC Essential Newborn Care EPI Expanded Program on Immunization FHT Female Health Technician FLCF First Level Care Facility FMT Female Medical Technician 2 FP Family Planning FWC Family Welfare Center HO Health Officer HEB High Energy Biscuits ICU Intensive Care Unit IDD Iodine Deficiency Disorders IMNCI Integrated Management of Newborn & Childhood Illness IMR Infant Mortality Rate IYCF Infant & Young Child Feeding IPC Inter Personal Communication ISO International Standards Organization CSG Community Support Group LHS Lady Health Supervisor LHV Lady Health Visitor LHW Lady Health Worker MIS Management Information System MMR Maternal Mortality Ratio MNCH Maternal, Newborn and Child Health MNT Maternal and Newborn Tetanus MO Medical Officer MS Medical Superintendent MSDS Minimum Service Delivery Standards MUAC Mid Upper Arm Circumference NEB Nursing Examination Board NGO Non-Government Organization NID National Immunization Day NNMR Neonatal Mortality Rate NTT Newborn Tetanus Toxoid Ob/Gyn Obstetrics Gynecology OPD Out Patient Department ORS Oral Rehydration Salt ORT Oral Rehydration Therapy 3 OTP Out Patient Therapeutic Program P&D Planning and Development Department PC-1 Planning Commission – Performa 1 PDHS Pakistan Demographic Household Survey PDS Pakistan Demographic Survey PHC Primary Health Care PIHS Pakistan Integrated Household Survey PMU Provincial Program Management Unit PNC Pakistan Nursing Council PSC Provincial Steering Committee PSDP Public Sector Development Program PSLM Pakistan Social and Living Standards Measurement survey PTS Principle Training Site RHC Rural Health Center RHP Reproductive Health Project RHSC Reproductive Health Service Center RUTF Ready to Use Therapeutic Food RUSF Ready to Use Supplementary Food TBAs Traditional Birth Attendants TCHC Tehsil Community Health Council THQ Tehsil Headquarter Hospital UC Union Council UNFPA United Nation’s Population Fund UNICEF United Nation’s Child Fund VCC Vehicle Condemnation Committee WB World Bank WHO World Health Organization WHP Women Health Project WMO Women Medical Officer 4 PC-1 PERFORMA Code Number for Project_____________ (To be filled in by Planning Commission) PART “A” PROJECT DIGEST Integrated Reproductive Maternal Newborn & Child Health (RMNCH) &Nutrition Program 1.1 Name of the Project 1.2 Location of the Project All 36 districts of Province of Punjab 1.3 Authorities Responsible for: i. Sponsoring. Government of Punjab Department of Health, Punjab and District Governments in ii. Execution. Punjab Department of Health, Punjab iii. Operation & maintenance. iv. Concerned Planning & Development Division federal ministry 1.4 (a) Plan provision i. If the project is The National Programs i.e. Lady Health Workers’ Program included in the (LHWP), National Maternal, Newborn and Child Health Medium Term/five- (MNCH) Program and Nutrition Program, were included in year plan, please the Ten-Year Perspective Development Plan 2001-11 and specify actual Medium Term Development Framework 2005-10. The allocation. Programs have also been identified as major health sector interventions in the Poverty Reduction Strategy Papers-I and II. The Government of Pakistan is a signatory to the Millennium Declaration and this effort is aimed to achieve health related goals. This Program will also contribute to all three key health & nutrition sector reform areas of the Economic Growth Framework announced by the Planning Commission in May 2012. 5 Total Block Provision: Rs. 40.28 Billion for PHC Programs for the period 2005-10. After the 18th Constitutional Amendment, the Federal Government committed to continue funding for vertical national health programs till 2014-15 i.e. by the announcement of the next National Finance Commission Award. ii. If the project is The Program will require federal funds. Some donor funding proposed to be may also be available in the form of grants, results based aid financed out of and technical assistance. block provision for a program indicate Punjab Government Share Rs.9424.006 (M) for 2013-2016. UNICEF Share for 2013-2014 Rs.260.155 (M) WFP Share for 2013-2016 Rs130.010 (M). (b) Provision in the Total Cost: Rs. 9814.171 Millions current year PSDP/ADP 1.5 Project Objectives and This program is inspired by the desire of the government to its relationship with reduce maternal, newborn and child morbidity and mortality, Sectoral Objectives promote family planning services and improve nutritional status of women and children. The achievement of this objective is also part of the government’s commitment to make speedy progress to achieve health related ‘Millennium Development Goals’ by 2015 and setting the roadmap towards achieving ‘Universal Coverage’ of health services in Punjab. This program will contribute in achieving health sectoral priorities in line with ‘Poverty Reduction Strategy Paper –II’. The salient features of the currently proposed program are that it adds on to what is already being done in the MNCH and LHWs Programs to achieve Millennium Development Goals 4 & 5. It will act as catalyst to assist ongoing initiatives. Additionally, new initiatives being proposed address malnutrition and aim to increase accessibility of MNCH services by provision of 24/7 service delivery at selected BHUS, all RHCs, THQs and DHQs. BHUs will be selected by a notified Provincial Management Committee (see Administrative Structure); the criteria for selection includes geographical distribution of and the community’s 6 accessibility to individual facilities. The program will contribute to all health& nutrition sectoral priorities set in the ‘Economic Growth Framework’ of the Planning Commission, i.e. 1: Revamping/management of primary, secondary and tertiary healthcare; 2: Healthcare Financing Reforms; and 3: Governance reforms in health sector (especially setting quality standards; essential services package; aid effectiveness, service structure; capacity; access to affordable medicine; etc.) Recently, the Government of Punjab has developed a draft ‘Punjab Health Sector Strategy (HSS) 2012-20’. Punjab HSS outlines six key areas of reforms in line with the six building blocks of the health system. Accordingly, implementation strategies have been defined to achieve these policy objectives. This program is contributing to all six outcomes of the Punjab Health Sector Strategy i.e. Outcome 1: Improved access and quality of healthcare; Outcome 2: An efficient system of health sector governance, accountability and regulation; Outcome 3: A management system that provides incentives for performance and ensures accountability; Outcome 4: Adequate and skilled workforce available to fulfill population health needs; Outcome 5: A comprehensive, timely, accurate and functional information foundation for health policy and planning decisions; and Outcome 6: Uninterrupted supply of quality essential drugs for healthcare facilities and outreach workers. Continuing and expanding services through national and provincial health programs and setting up an integrated system to be implemented in all districts of Punjab is the most important aspect of the agenda for change. This Program will constitute the main thrust of outreach and 7 facility based services in rural and less developed urban areas for provision of improved reproductive, maternal, newborn, child health and nutrition services in Punjab. GOAL: To improve maternal, new-born and child health in Punjab, especially of the poor thereby making real progress towards achieving health related MDGs and contribute to reduction in: maternal mortality ratio from 227/100,000 live births in 2006-07 to less than 140/100,000 live births by end 2016; under-five mortality rate from 104/1000 live births in 2011 to 52/1000 live births byend2016; total fertility rate from 3.6 in 2011 to 3.2 by end 2016; and prevalence of stunting from 36% in 2011 to 32% by end 2016 PURPOSE/OBJECTIVES: The Program objective is to improve access to Reproductive health, Child health and Nutrition services in the province especially for the poor through: improving contraceptive prevalence rate for modern methods from 23% in 2011 to 35 % by end 2016; increasing skilled birth attendance from 59% in 2011 to 80% by end 2016; increasing institutional deliveries from 53% to 70% by end 2016; increasing coverage of complete immunization from 35% in 2011 to 70% by end 2016; increasing percentage of children suffering from diarrhea treated with ORS and Zinc, up to 40% by end 2016; Increase in the proportion of severe acute malnourished (with complications) children 0-59 months successfully treated (for discharge) up to 75%by end 2016; Increasing percentage of early initiation of breast feeding from 15% in 2011 to 40% by the end of 2016; 8 Increasing percentage of exclusive breast feeding from 22% (0-5 months) in 2011 to 35% by the end of 2016; Increased percentage of utilization of adequately Iodized salt at household level from 34% to 50% increase in the distribution of iron & folate tablets among pregnant women from 20% in 2012 to 50% by end 2016; increase in proportion of children 6-23 months fed in accordance with all three infant and young child feeding (IYCF) practices (food diversity, feeding frequency, consumption of breast milk or milk), up to 40% in 2016 All district implementing MNCH related MSDS by end 2016 The principal sources for the verification of Program performance against set targets will be independent Program evaluations; National and Provincial surveys e.g. Punjab MICS, PDHS and PSLM, in addition to Program monitoring and supervisory systems. 1.6 Description, Pakistan’s health MDGs’ targets have improved over last two Justification & decades but they still lag well behind other countries at Technical Parameters similar levels of income and it is unlikely that Pakistan will achieve its health targets by 2015.Challenges include huge social, cultural and economic barriers to health, particularly for women, and service delivery in rural and insecure areas of the country. Because of competing budgetary and security priorities, the Government of Pakistan currently invests only about 0.86% of its GDP in the health sector which is among the lowest in South Asia, other than Afghanistan. Punjab, being the largest province with a population of 95 million greatly skews national outcome indicators. Progress on achieving health MDGs in Punjab is slow, though comparatively better than other provinces. The maternal mortality ratio in Punjab is 227/100,000 live births (PDHS 2006-07), under five mortality rate is 104/1000 live births (MICS 2012) and total fertility rate is 3.6 (MICS 2012). Prevalence of nutritional disorders, infectious diseases and access to reproductive, maternal, newborn and child health care services, although better compared to other provinces 9 remains poor compared to other South Asian countries. Since Independence, public health financing in the country has given priority to curative healthcare. Although a considerable number of health facilities have been made, their rate of utilization is limited. Recognizing this, the government of Pakistan launched a number of national health program over the last two decades which were designed to improve health outcomes through cost effective interventions. Provinces, including Punjab proactively implemented these national health programs. However, as an implication of the 18thConstitutional Amendment, these programs have been completely devolved to the provinces from 30 June 2011. As per decision of the Council of Common Interest, the Federal Government agreed to continue funding of these national programs till the next Finance Commission Award (NFC) in 2014-15, except the LHWP which will be funded till 2017. The Punjab Government considers this as an opportunity not only to develop its capacity to play a new role in the health sector but also to deliver primary and preventive health care interventions through an integrated and cost effective approach. This will also help the provincial government to shift its priorities from curative care/private goods to predominantly primary and preventive health care/public goods. To meet the challenge, the Department of Health developed its Health Sector Strategy (HSS) 2012-20, to set a roadmap to ensure this paradigm shift in the health sector. One of the priority strategic areas of the HSS is to deliver ‘Essential Package of Health Services (EPHS)’ at primary, secondary and tertiary level. Recent devolution of the vertical national health programs will help the government in materializing the concept of delivery of EPHS at the district level initially for primary health services. However, a phased approach is required first to integrate primary and preventive health care services 10 through an integrated provincial program for a period of three years; in the meantime enabling Districts to take over all primary & preventive health care implementation responsibilities for the delivery of EPHS. Development of this program is a way forward not only to continue existing interventions through an integrated approach but to expand their scope and introduce new interventions. Some of the program/ interventions which will be integrated and implemented through this program are as following: 1: The National Program for Family Planning and Primary Health Care, also known as the Lady Health Workers Program (LHWP), launched in 1994. The Program objectives contribute to the overall health sector goals of improvement in maternal, newborn & child health and provision of Family Planning services. This country wide initiative extended outreach health services to rural populations and urban slum communities through deployment of over 100,000 Lady Health Workers (LHWs) and contributed to bridge the gap between health facilities and communities. 2: National Maternal, Newborn and Child Health (MNCH)Program (2006-2012) was lunched nationwide with a goal to improve maternal, newborn and child health of the population, particularly among its poor, marginalized and disadvantaged segments. The program is contributing to strengthen Emergency Obstetric care services at DHQ, THQ hospitals and RHCs. Further, this program has introduced a new cadre of Community-Midwives (CMWs) for skilled deliveries at community level. 3: A network of BHUs, RHCs, THQ and DHQ hospitals which are managed by the District Governments play a critical role in provision of reproductive, maternal, newborn and child health services. In Punjab, some of 11 the resource gaps related to MDG 4 and MDG 5 services are proposed to be filled by this Program. 4: Punjab is also moving towards functional integration of Family Planning services offered through the Department of Population Welfare. This initiative of functional integration will be strengthened through this proposed program. 5: The Chief Ministers’ Health Initiative for Attainment and Realization of MDGs 4 & 5 (CHARM) was launched in seven districts of Punjab, with the assistance of UNICEF & UNFPA, following severe floods in the year 2010. The program is helping in revival and utilization of the existing infrastructure of the Department of Health and expansion of round the clock Basic EmONC services through skilled paramedical staff in selected RHCs and BHUs. It is proposed to expand and upscale this initiative initially in 16 districts having poor health indicators related to MDGs 4 & 5.By 2016, the initiative will be expanded to 20 Districts. 6: The preventive nutrition interventions are being proposed for all 36 districts; additionally, curative component addressing malnutrition is proposed in 12 targeted Districts and urban peripheries of 9 megaDistricts of Punjab. In view of the compelling requirements to address health needs of women and children, the Government of Punjab, with support from development partners, implemented successfully above mentioned interventions in an integrated manner. But with new strategic responsibilities, the Department has decided to play a new role and integrate all above mentioned interventions to set up a roadmap for the delivery of EPHS at District level and strengthen the stewardship role at Provincial level. A two stage implementation mechanism will help the Department to gradually shift some of the interventions from development to recurrent budget, while generating more evidence on 12 what works. The integrated program will focus on reproductive, maternal, newborn and child health and nutrition services with improvements in governance, financing and M&E mechanisms. Integration of interventions will help the Government to avoid duplication of activities, effective use of meager resources and ensuring enhanced efforts in the province which would facilitate achievement of health MDGs. IMPLEMENTATION STRATEGIES: The program will strengthen the health system by integrating different interventions, improving service delivery and introducing innovative strategies. The program will: 1. Strengthen district health system through integration of quality reproductive, maternal, newborn, child health and nutrition services at community, BHU,RHC, THQ and DHQ level and focusing on rural areas and gradually move towards delivery of EPHS (primary) at the district level; 2. Strengthen linkages of community based health services with health facilities through LHWs and CMWs focusing on rural areas& urban slums; 3. Streamline and strengthen services for provision of Basic and Comprehensive Emergency Obstetric and Newborn care (EmONC); 4. Enhance comprehensive Family Planning services at community and facility level; 5. Enhance Nutrition services at community and facility level through multi-sectoral coordination mechanism 6. Increase coverage of micronutrient supplementation and fortified food through advocacy from consumer to production line; 7. Implementing a Woman Focused Approach by using the 1000 days Plus Model for nutrition, which focuses on the critical window of 1000 days from conception to the first 24 months of the child’s life; 8. Involve local communities at different levels to enable 13 them to participate in health improvement process; 9. Improve technical and managerial capacities at all levels of health care delivery system and expand accountability mechanism vis a vis performance based incentives in health care delivery system; 10. Introduce and implement e- monitoring and ereporting system 11. Increase healthcare demand services for preventive through and primary targeted, socially acceptable communication strategies 12. Strengthen referral linkages between community outreach staff, primary facilities and secondary facilities 13. Improve client/ patient satisfaction from provision of services 1.7 The Project Costs Date when capital expenditure estimates were prepared: February 2013. The costs have been estimated on the Local: prevailing rate of the market and based on previous work GOP: done. Punjab Government Share Rs.9424.006 (M) for 2013-2016. Foreign exchange cost: UNICEF Share for 2013-2014 Rs.260.155 (M) WFP Share for 2013-2016 Rs130.010 (M). Total: Total Cost: Rs. 9814.171 Millions 1.8 Annual Operating and Average Annual Operating Cost is Maintenance cost Rs. 3271.390 Millions for the FY 2013-16. after completion of the project: (Item wise annual Operating Cost) Employees Related Expenses Communication Utilities Occupancy Cost Training Domestic (All Trainings of LHWs, LHSs etc., TOT) TA/DA Transportation of Goods POL Local Conveyance Charges Stationary Printing & Publication 822.955 1.160 0.600 0.500 44.133 0.500 10.333 33.600 0.010 0.100 3.333 14 1.9 Sources of Financing: Conference/Seminars 0.600 Newspaper, Periodicals & Books 0.010 Advertisement & Publicity 2.000 Law Charges 0.005 Purchase of Drugs & Medicines 518.615 Others (Supplies for Nutrition Components & Consumables) 1.920 Pension Contribution. 0.313 Entertainment & Gifts 0.010 Software (Physical Assets) 1.267 IT Equipment (Physical Assets) 2.133 Medical Store(Contraceptives) 283.333 Others Store & Stock 1389.970 Machinery Equipment 150.850 Furniture & Fixture 2.192 Transport Repair 0.848 Soft Ware Repair 0.100 Total 3271.390 The source of funding will be the Provincial Government ( Provincial ADP) Funds may also be available from bilateral and multilateral donors and lending agencies. This project will direct available funds at the District level for providing services. 1.10 Demand and Supply The Government’s health expenditure in Pakistan is very low Analysis – only 0.85% of the Gross Domestic Product (GDP) and 38.5% of the total health expenditure (both public and private) for the year 20101. Government’s per capita health expenditure is $8 per person per year (increased from $4 in 2003).Though doubled in Us dollar terms since 2003,it remains very low compared to the recommended expenditure of $34 per person per year on essential health services by the Commission on Macroeconomic and Health. Total (both public and private) per capita health expenditure is $22 per person per year (2010 figures)1. Majority of the expenditure in the private sector is in the form of ‘out of pocket’ expenses of service users. In general, utilization of public health facilities is low, resulting into high per capita cost of service provision. 1WHO National Accounts for Pakistan 15 The proposed program will attempt to fulfill the unmet health needs of the general population in the province through provision of family planning, maternal, newborn and child health care, EmONC services and nutrition services. The program aims to achieve its objectives through strengthening health system through improving facility based and community based interventions and ensuring community participation at all levels. One of the important aspects that the program plans to address is to restore the trust of communities on public sector health services. The increased utilization of public sector, in turn, will reduce per capita costs of healthcare delivery, particularly with regard to general health and MNCH. A major constraint in improving availability and quality of health services is inadequate financial space available for provision of these services. The proposed program will increase cost-effectiveness and efficiency of health services by increasing their quality and access through synergistic action with the ongoing initiatives. The distribution of health services is disparate with a majority of skilled health personnel being concentrated in urban areas. This program will improve the quality, access, affordability and utilization of health services in the rural areas by providing 24/7 EMNOC services at selected BHUs, all RHCs. The number of deliveries conducted by skilled birth attendants has recently increased to 59% in Punjab but still significant deliveries are being conducted by unskilled traditional birth attendants or family members. In case of obstetric and newborn complications, the availability of emergency care is severely limited. There is a limited supply of technology intensive services limited to large urban conglomerates while on the other hand in the rural areas there is a shortage of qualified practitioners. The supply side of health services especially in the public sector is limited due to non-availability of trained human 16 resources, and appropriate equipment, in spite of availability of a vast network of health facilities throughout the country. Although at present the share of individual household’s out of pocket expenditure on health care is very high, the total expenditure on health is still below the optimum levels when compared internationally. This can only be improved through infusion of additional resources into health system either through Government expenditures, or alternative financing mechanisms. Given the level and distribution of poverty the need for a Government subsidy essentially remains and therefore the best mechanism would be targeting the subsidy to the poorer part of the population. This would create a healthier population base which has access to higher quality of care. The program targets rural areas and urban slums for provision of subsidized services and will lead to a decreased out of pocket expenditure on health care while providing improved quality of care to the population. 1.11 Financial Plan and 1. Punjab ADB mode of financing 2. Grants/Results Based Aid from WB and DFID are expected to cover the program. In this respect EAD has formally requested WB for financing in Punjab 3. In addition, TA support from DFID, USAID, UNICEF, WFP, UNFPA, WHO, WFP and other international agencies are also expected. 1.12 Project benefits and analysis: No direct financial gains are expected from the program. a) Financial, However, reduction in morbidity and mortality in the Social and population, control in population and improvement in environmental nutritional status would lead households to have more Benefits resources and spend on improving quality of their lives, better learning on children and health life styles. Financial Considering that health is a basic right of every human being, the program will improve access to health care to all individuals of the society, especially the poor and more deprived. Access to primary, reproductive and nutrition health care will improve health status of communities leading to improvement in the overall quality of life. Improvement in social benefits will be measured by reduction in: 17 Social Benefits with 1. Under five Mortality Rate; Indicators 2. Maternal Mortality Ratio; 3. Population Growth Rate; 4. Total Fertility Rate 5. Crude Birth Rate; and 6. Improvement in literacy rate. Employment Health and poverty are closely linked with each other; generation (direct already poor people who are also unhealthy and vice versa. It and indirect) is envisaged that health status improvements will enable individuals to avail more choices/opportunities that can help in improving quality of their lives like attaining education, competing for better employment opportunities and contributing towards their families and society’s betterment, hence enjoying their life. Improved health behaviors and ensured access to primary health care services will not only reduce the suffering at individual level but will also reduce the cost of treatment if preventive measures were taken on time or when treated at an early stage. In the end, investment on treatment of complicated cases will be decreased and would allow planning for the development projects. It is difficult to put these benefits in figures but their significance cannot be overlooked. Another feature of the program is to organize communities in such a manner that ensures their active participation in planning, administration and management of health care system in their area. This will facilitate the functioning of health delivery system on one hand and empowering the communities on the other hand. Moreover, in the process, the organized communities are expected to take other development initiatives to identify and solve their local issues. Program will build capacities of local communities by increasing their awareness regarding health issues and adopting healthy behaviors; of local staff by enhancing their skills and knowledge in health care services provision; of 18 community representatives in planning small projects, administering and managing health services; and district health management teams in management, supervision, target setting & better planning for health care delivery system. Although majority of service providers and management cadre are currently working, but over the program period effort would be made to absorb service providers in the DOH and District Health Office as part of the structural reforms. Indirect employment opportunities will also emerge related to the management/ organizational functions of the Program. The program will certainly have a positive impact on the environment, with improved reproductive health outcomes. Environmental impact The improved health behaviors will lead to healthy life styles which are not possible without maintaining self-cleanliness (including hand washing), cleanliness at the household, street and society level. The appropriate disposal of human, liquid and solid wastes will further help improving the environment. There is enormous amount of hospital waste which is not handled safely and generally leads to spread of killer diseases like hepatitis, etc. The program will make sure that, in all health facilities, hospitals and at community level, waste is adequately disposed of through implementation of infection control protocols. This program is a high priority for the government to make speedy progress on health & nutrition outcomes. Delays in Impact of delays on project cost and viability the undertaking will lead to increased cost in achieving health and nutrition MDGs. Majority of the interventions in the program are having very low cost per DALYs provided these are implemented on time. Delay in implementation will lead to continued high burden of mortality and morbidity and serious cost implication on the households. Currently, the government is indicating commitment to absorb different interventions as regular function of the public health sector. 19 b) Project The program will be having four major outputs: Analysis: 1: planning and nutrition services under Essential Quantifiable outputs of the project: Improved delivery of maternal, newborn, child, family Package of Health Services; 2: Increased demand side interventions for Reproductive health, Child health and Nutrition services; 3: Effective management of the Program at provincial and district level; and 4: Improved decision making through high quality information and research Please refer to the Logical Framework (next section) of the Program which includes indicators for each output along with milestones and targets. 1.13 Unit cost analysis: Average Cost of Married Women & Children Rs. 116/- Management The ultimate objective for implementation of the program at Structure & operational level will be through the current Government Manpower structure of the Health Department. Additional management Requirement staff will not be required as it is proposed to be implemented with integrated approach with MNCH & LHWS Program. For all practical purpose three programs will be implemented under one umbrella. Staff employed for the management of the program through development budget will be shifted to recurrent side as part of structural reforms at Provincial and District levels. The program management and manpower requirement is discussed in detail in the relevant section. The brief roles and responsibilities, qualification and remuneration are also discussed in the section of job descriptions. 20 PREPARED BY: Dr. AkhtarRashid Provincial Coordinator Lady Health Workers’ Programme Department of Health, Punjab CHECKED BY: Mr. FarasatIqbal Project Director Health Sector Reform Programme Department of Health, Punjab Dr. ZafarIkram Provincial Programme Manager MNCH Programme Department of Health, Punjab Dr.NisarCheema Director General Health Services Department of Health, Punjab APPROVED BY: Capt (R) ArifNadeem Secretary Health Department of Health, Punjab Dated: 25-02-2013 21 LOGICAL FRAMEWORK: PROGRAM NAME Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program GOAL Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 To improve maternal, new-born and child health in Punjab especially of the poor thereby making progress towards achieving health related MDGs Maternal Mortality Ratio (MMR) 227/100,000 lb – PDHS 2006-07 190/100,000 180 170 140/100,000 lb Assumptions Source Pakistan Demographic & Health Survey (PDHS) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Neonatal Mortality Rate (NMR) 58/1,000 lb (PDHS 2006-07) 52 50 48 44 Source Pakistan Demographic & Health Survey (PDHS) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Infant Mortality Rate (IMR) 82/1,000 lb – MICS 2011 80 75 70 40 Source Pakistan Demographic & Health Survey (PDHS) / MICS Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Under 5 Mortality Rate 97/1000 lb – PDHS 2006-07 102 98 92 52/1,000 lb 104/1000 lb - MICS 2011 Source Multiple Indicator Cluster Survey (MICS), Pakistan Demographic & Health Survey (PDHS) 22 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Total Fertility Rate (TFR) 3.9 – PDHS 06-07 3.5 3.4 3.3 3.2 3.6 - MICS 2011 Source Multiple Indicator Cluster Survey (MICS), Pakistan Demographic & Health Survey (PDHS) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Stunting (moderate & severe) prevalence 36% - MICS 2011 35 34 33 32% Source Multiple Indicator Cluster Survey (MICS) 23 PURPOSE Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Assumptions To improve access to quality Reproductive health, Child health and Nutrition services especially for the poor Contraceptive Prevalence rate (Modern methods) 23% – MICS 2011 26% 30% 35% 35% Macro-economic situation (both at national & provincial level) improves and economic growth accelerates Source Multiple Indicator Cluster Survey (MICS), Pakistan Demographic & Health Survey (PDHS) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Skilled Birth Attendance (SBA) 46% (37R, 64U) PSLM 10/11 65% 75% 80% 75% (72R, 80U) 59% - MICS 2011 Source Multiple Indicator Cluster Survey (MICS), Pakistan Social & Living Standard Measurement Survey (PSLM) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Institutional Deliveries 43% (34R, 63U) PSLM 10/11 56% 60% 70% 75% (70R,80U) 53% - MICS 2011 Source Multiple Indicator Cluster Survey (MICS), Pakistan Social & Living Standard Measurement Survey (PSLM) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Fully Immunized Children 34.6%-(Fully immunized with Measles 2)MICS 2011 45% 55% 70% 80% Source Multiple Indicator Cluster Survey (MICS), Pakistan Social & Living Standard Measurement Survey (PSLM) Political and security situation in the country improves No major humanitarian disaster in the province Institutional risks related to devolution and formation of new administrative areas are appropriately mitigated Improvement in literacy rate Health, Population and Nutrition programs, projects and 24 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Per cent of Children suffering from diarrhea treated with ORS and Zinc NA 15% 25% 35% 40% Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Percent of registered children, in the 12 priority districts, successfully treated for severe acute malnutrition (with complications). 20% 40% 50% 60% 75% Indicator Baseline Milestone 3 2015-16 Target 2017 Percentage of identified SAM children enrolled for treatment in 12 priority districts interventions are harmonized provincial and district level Source Multiple Indicator Cluster Survey (MICS), Pakistan Social & Living Standard Measurement Survey (PSLM) Source Multiple Indicator Cluster Survey (MICS) 2011 Milestone 1 2013-2014 - Milestone 2 2014-15 50% 55% 60% 80% Source Program Database Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Percentage of registered pregnant women receiving iron folic acid tablets 20 30% 40% 50% 60% in 2016 Source National Nutrition Survey (NNS) 25 INPUTS (HR) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 No of districts implementing MNCH related Minimum Services Delivery Standards 18 districts 30 districts All districts MSDS reviewed All districts implementing MNCH related MSDS Source Third party assessments FTEs 48,000 LHWs deployed 9,000 CMWs trained Required staff in health facilities (BHUs, RHCs, THQ & DHQ hospitals Required Management staff at provincial and district level OUTPUT 1 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Assumptions Improved delivery of maternal, child, family planning and nutrition services under Essential Package of Health Services Average number of FP clients per month per primary and secondary level facilities Average 60FP clients per month per facility in 2011 – DHIS Average 80FP clients per month per facility Average 100FP clients per month per facility Average 120FP clients per month per facility Average 120FP clients per month per facility Increased and sustained political commitment to reproductive, maternal and child health service delivery reflect increased government investment in health sector Source District Health Information System (DHIS) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Average FP users per month per LHW catchment population Average 50 FP users per month per LHW catchment population – LHW-MIS 2011 Average 53 FP users per month per LHW catchment population Average 56 FP users per month per LHW catchment population Average 60 FP users per month per LHW catchment population Average 60 FP users per month per LHW catchment population Funding support from federal government continues/ enhanced and fiduciary risks mitigated Source Program Management Information System Provincial funding and 26 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 DHQ, THQ hospitals and RHCs providing Comprehensive EmONC services 28/36 DHQ and 40/84 THQ hospitals and Nil/291 RHCs providing 24/7 Comprehensive EmONC services in 2011 – HFA 2011 32/36 DHQ and 50/84 THQ hospitals and 10/291 RHCs providing 24/7 Comprehensive EmONC services 34/36 DHQ and 60/84 THQ hospitals and 20/291 RHCs providing 24/7 Comprehensive EmONC services 36/36 DHQ and 70/84 THQ hospitals and 36/291 RHCs providing 24/7 Comprehensive EmONC services 36/36 DHQ and 75/84 THQ hospitals and 36/291 RHCs providing 24/7 Comprehensive EmONC services Health Facility Assessment Surveys, Program Management Information System Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 RHCs and BHUs providing Basic EmONC services (24/7) 150/291 RHCs and 88/2454 BHUs providing 24/7 Basic EmONC services in 2011 200/291 RHCs and 300/2454 BHUs providing 24/7 Basic EmONC services 250/291 RHCs and 500/2454 BHUs providing 24/7 Basic EmONC services 275/291 RHCs and700/2454 BHUs providing 24/7 Basic EmONC services All RHCs and 425/2454 BHUs providing 24/7 Basic EmONC services (Served on) Effective coordination between IntegratedPrograms and effective joint coordination and supervision mechanism. Milestone 1 2013-2014 Regular and uninterrupted supply of essential medicines and contraceptives to districts. Source Program Database Baseline Establishment of Stabilization Centers (SC) for Nutrition 5 Source Appropriate skilled human resource (particularly female) available/ deployed especially in hard to reach/ remote areas Devolution of powers does not have negative impact on service delivery Source Indicator donor assistance is available to fill the funding gaps 12 in priority districts Milestone 2 2014-15 30 (21 in priority districts) Milestone 3 2015-16 36 Target 2017 36 Districts ownership to the program and reforms. Program Database 27 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Establishment of OTP sites at 30% BHUs and all RHCs 111 OTP sites established Establishment of OTP sites in 179/291 RHCs and 438/2466 BHUs in 12 priority Districts and 9 peri-urban areas of megacities Establishment of OTP sites in 228/291 RHCs and 572/2466 BHUs in 30 Districts Establishment of OTP sites in 291/291 RHCs and 640/2466 BHUs in 30 Districts Target 2017 Source Program Database Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Exclusive breastfeeding till age of 6 months 22% 25% 30% 35% 40% in 2015 Source MICS 2011 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Early initiation of breastfeeding 15% 20% 30% 40% 50% Source MICS 2011 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Proportion of registered children 623 months fed in accordance with all three infant and young child feeding NA 10% 20% 30% 40% Source Program Management Information System 28 (IYCF) practices (food diversity, feeding frequency, consumption of breast milk or milk) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Iodized salt consumption 34% - MICS 2011 40% 46% 50% 50% 25% of community members able to identify at least 2 danger signs in childhood illness 40% of community members able to identify at least 2 danger signs in childhood illness 50% of community members able to identify at least 2 danger signs in early childhood illness Source Multiple Indicator Cluster Survey (MICS) Increased demand side interventions for Reproductive health, Child health and Nutrition services % of mothers able to identify at least 2 danger signs in early childhood illness (e.g. Pneumonia) 7% of mothers able to identify at least 2 danger signs in childhood illness 20% of mothers able to identify at least 2 danger signs in childhood illness Source Multiple Indicator Cluster Survey (MICS) Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 % of mothers aware of at least two benefits of exclusive breast feeding NA 30 35 40 50% Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 % of district implementing awareness interventions during NA 10% 40% 80% 100% Increased and sustained political commitment to reproductive, maternal and child health service delivery reflect increased government investment in demand side interventions Human resources (particular women) required available, deployed and retained Source Community-based survey Source District Communication Intervention reports Private sector facilitates the public sector in creating awareness and changing behaviors related with RCN Effective coordination 29 World Health Day, World Population Day, World Midwifery Days, World Child Day, Mother & Child health week and World Hand Washing Day between program and projects for coordinated communication interventions Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 % of patients/ clients visiting health facilities who are very satisfied with provision of RCN services 20% very satisfied and 75% satisfied 35% 45% 55% 60% very satisfied patients/ clients System of regular monitoring/ assessment functional Source Health Facility Assessment Surveys 2011 30 OUTPUT 3 Indicator Baseline Effective management of the Program at provincial and district level Office of Integrated Implementation Unit established Source Indicator Baseline - Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 100% 100% 100% Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 1 LHV at every health facility and all LHWs and LHS in 7 Districts 1 LHV at every health facility and all LHWs and LHS in 12 Districts 1 LHV at every health facility and all LHWs and LHS in all 36 Districts Atleast 15,000 LHWs trained on Training Package Administrative data No of Health Care providers Trained on Training Package (IYCF & HTSP) - Assumptions Strong strategic leadership at provincial and district level reflected through performance of steering committee and DHMTs Required competent health managers/ staff available and deployed at appropriate level Source Administrative data Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Days out of stock for contraceptive methods (minimum 4 at health facilities and CMW level and minimum 3 at LHW level), ORS, Zinc, Amoxicillin, Tab Iron/Folic acid/ B12 and Tab Paracetamol at all levels. 100% in 2011 – HFA 2011 50% 30% 25% 10% Source Health Facility Assessments, District Health Information System (DHIS) Macro-economic stability and availability of appropriate funds Fiduciary and institutional risks appropriately mitigated Effective system of performance of managers functional 31 Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Days out of stock for Inj Magnesium Sulphate, Injection Oxytocin, Inj Ampicillin and Mesoprostol at health facility level 100% in 2011 – HFA 2011 50% 30% 20% 5% Indicator Baseline Milestone 1 2013-2014 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 e-monitoring and complaint mechanism established and made functional Under piloting 7 districts 12 districts All districts Accountability and complaint mechanism established in all districts Source Health Facility Assessments, Program database Source Progress Reports 32 OUTPUT 4 Indicator Baseline Milestone 1 2012-13 Milestone 2 2013-14 Milestone 3 2014-15 Target 2017 Assumptions Improved decision making through high quality information and research Performance review of districts organized at provincial level using information data Quarterly review held Quality review meetings Quality review meetings Quality review meetings Quality review meetings Annual performance review Annual performance review Annual performance review Strong commitment at provincial level to integrate health information systems with strong leadership Annual District performance disseminated through DOH website Annual District performance disseminated through DOH website Annual District performance disseminated through DOH website Annual performance review Annual District performance disseminated through DOH website Source Minutes Indicator Baseline Milestone 1 2013-14 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Improved quality of data LQAS in DHIS only Internal validation of data External validation review Internal validation of data Regular validation data Source Validation results Indicator Baseline Milestone 1 2013-14 Milestone 2 2014-15 Milestone 3 2015-16 Target 2017 Verbal autopsy system functional for maternal deaths Irregular implementation 10 districts having functional system 25 districts having functional system All districts having functional system All districts having functional Verbal autopsy system Availability of effective organizations able to produce quality evidence and influencing policies Effective strategic partnership among development partners and the government to generate demand and provision of quality RCN services Security situation conducive to research and advocacy in all provinces/ areas. Annual provincial report published 33 Annual provincial report published Annual provincial report published Annual provincial report published Source Verbal autopsy reports INPUTS (Rs.) INPUTS (HR) Total Cost Rs. 9814.171 Millions Total Rs. 9814.171 Millions FTEs 34 PROGRAM DESCRIPTION Introduction and Rationale The global community under auspices of United Nations assembled in the year 2000 to identify and propose targets and indictors to improve the lives of people everywhere. At the culmination of this “Millennium Summit”, a joint charter for improving lives of people, especially marginalized segments including the poor, disabled and women and children was announced. This charter outlined eight goals/action points addressing poverty, health, food security and environment; these goals are referred to as Millennium Development Goals (MDGs), with two goals, MDGs 4 and 5 specifically addressing health of women and children. Millennium Development Goals thus define a contemporary framework for gauging success of a country/region toward achieving development and uplift for its people. Current Health Situation Pakistan houses the world’s seventh largest population, currently estimated at 180 million people2. Punjab is the most populated province; it is also considered an affluent region of the country. This is largely attributed to the rich agricultural base of the region, which remains the main source of employment for inhabitants of the province. Despite relative affluence, analysis reveals a dismal picture of woman and child health in Punjab. The province houses an estimated population of 92 million3, growing at an annual rate of 1.9 percent. Total Fertility Rate (TFR) is a health indicator reflecting a woman’s reproductive burden and risk of related morbidity and mortality associated with child birth; Punjabs’ TFR is currently reported at 3.64. Skilled Birth Attendant (SBA)5 play a crucial role in protecting lives of mothers and newborns by ensuring clean and medically sound delivery practices, early identification and prompt management of complications6. According to MICS 2011, 74% of women in Punjab receive only one Antenatal Care (ANC) visit from SBAs during pregnancy; this reflects missed opportunities for identifying and managing high risk pregnancies. Additionally, with more than 41%7of births attended by unskilled attendants, the risk of delivery-related complications among mother and child are compounded. The MMR for Punjab (227 per 100,000 live births8) is lower as compared to other regions of the country; however, it is still high when compared with neighboring countries of South Asia. The High TFR and MMR in the province are also indicative of the fact 2 State of the World’s Children, UNICEF, 2011 www.statepak.gov.pk 4 MICS 2011 3 5 6 Healthcare professional trained in pregnancy, delivery and newborn care http://wbln0018.worldbank.org/news/pressrelease.nsf. MICS 2011 7 35 that the experience of pregnancy and other reproductive health related aspects among women in Punjab predispose them to a high risk of morbidity and mortality. Adequate nutrition influences the health status of women and children to a great extent. The prevalence of anemia is significantly high amongst pregnant women9; this coupled with low caloric intake during pregnancy has a negative impact on the growth of the foetus, resulting in nearly 28% of births being low weight. Globally 26% of children under the age of five years are moderately or severely malnourished10. The prevalence of underweight, stunted and wasted children is higher in South-eastern Asia as compared to other regions of the world, in Pakistan, 37% of children under the age of five years are underweight for age, among which 12% suffer from severe malnutrition; 37% are stunted and 13% suffer from wasting11. In Punjab every third child below the age of five is estimated (34%) to be underweight. Women and children in Punjab also suffer from high rates of deficiencies in essential vitamins and minerals. To understand the health status of children (those less than 5 years of age), the Infant Mortality Rate (IMR) and Under 5 Mortality Rate (U5MR) are considered to be the key indicators for assessing the health in this age group in a population. The infant mortality rate is 82 per 1,000 live births for Pakistan and 77 for Punjab as compared to 41 in Indonesia and 15 in Sri Lanka12.These indicators reflect the rates of mortality among those less than one year and those less than 5 years of age respectively. In Punjab, the IMR and U5MR have steadily declined since 1990; however, the rate of decline over the last fifteen years has been considerably slower than its South Asian neighbors. The U5MR for the Punjab is estimated to be 94 per 1,000 live births. These translate as one in every thirteen children born in the province does not survive till the first birthday, while one in eleven newborns does not make it to the fifth birthday. This data reflect the abysmal conditions of health among the more vulnerable segments of the population that include the women and children of the province. This snapshot of health status indicates that Punjab is far from achieving the health related MDG targets. Such health indicators on the part of the provincial health department also warrant a comprehensive and effective plan of action on a war footing, to improve the existing deplorable health conditions and indictors for the women and children. Keeping in view the state of health conditions among women and children of the province, the Government of Punjab is currently implementing a wide range of initiatives focused towards the health of women and children. These include the Nutrition Program for Mothers and Children, Chief Minister’s Health Initiative for Attainment & Realization of MDGs (CHARM), National Program for Family Planning and Primary Health Care (i.e. the Lady Health Workers Program), Maternal Newborn and Child Health Program (MNCH), and the People’s Primary Health Care Initiative. 8 The Pakistan Demographic and Health Survey 2006-07 National Nutritional Survey, Government of Pakistan, 2001-2; 10 State of the World Children, UNICEF, 2006; 11 UNICEF - Global Database on Child Malnutrition http://www.childinfo.org/areas/malnutrition/underweight.php 12 World Development Indicators, 2002; 9 36 In their respective domains, all of these initiatives focus on various dimensions of health, healthcare and services use among women and children. The presence of multiple programs which function in silos leads to low levels of integration at the basic health facility and the community level. It is proposed that LHW Program, MNCH Program and Nutrition Program may be implemented under a single management structure. The Government of Punjab envisages to achieve measurable impact on MDGs through improving the performance of health management system; improving access and quality of trained manpower, enhancing medicines and technology in health services system, reviewing existing policy framework; improving infrastructure; creating health mass awareness; introducing public private partnerships and broadening health financing mechanisms. Introduction & rationale to upscale CHARM pilot project In the month of July & August 2010, floods affected millions of people in Pakistan. Unfortunately, the flood affected districts in Punjab were those where indicators of maternal, newborn and child health were not good even before they became flood-hit. The situation would have been aggravated if extra ordinary measures were not taken to improve reproductive health services in these areas. Taking into this consideration the entire situation, there was an urgent need to implement a comprehensive strategy at community and health facility level in order to prevent and reduce excess maternal and newborns mortality and morbidity. The Government of Punjab, with financial and technical support from UNICEF and UNFPA, started provision of 24/7 EmONC services and ensured primary health care services during the day time at BHUs and RHCs of the flood affected districts. By December 2011, 81 BHUs and 60 RHCs were equipped and started functioning round the clock, providing Basic EmONC services and reporting regularly on a monthly basis. The progress shown by converting almost nonfunctional BHUs to round the clock maternal and child care centers is remarkable and community feedback to these services is extremely positive. BHUs where not more than one delivery was conducted every month now boast of an average of over 40 verifiable deliveries per BHU. A strong referral system has also been established for referral of high risk and complicated pregnancies from house hold to basic health facility and onward to district hospitals to avert mortality and morbidity. 38 ambulances have been provided at the BHUs to provide emergency transport services to pregnant women from community to higher centers of care; these pick and drop pregnant women from the community to health facility on a phone call and in case of complications and high risk pregnancies, women are transferred to DHQ/ Tertiary care hospitals without any delay. By December 2012, 24/7 services are being provided at 89 BHUs and 60 RHCs in seven districts. Significant and sustained improvements in service provision and utilisation of services have been recorded at these facilities compared to baseline and provincial average monthly utilization. 37 Baseline (Nov 2010) Provincial Average (Aug-2012) CHARM Average (Aug 2012) 172 76 43 25 40 1 ANC 6 9 2 Delivery PNC It is a common observation that the existing management system at district level has failed in delivering the desired outputs expected out of it. Thus, an innovative approach for management and supervision of the health services using e-monitoring and e-reporting is being implemented and tested, resultantly absentee rate of staff even at remotest facility is nearly zero percent. Thus, an innovative approach for service delivery with e-tech management system and incentivizing staff is tested and showed unbelievable results. The cost – benefit analysis has shown that minor interventions done with dedication can lead to unbelievable performance. Rather than creating new vertical structures, strengthening of the existing systems and covering the gaps is the key to success of CHARM Program. Up-scaling the CHARM model across other districts of Punjab would be a major leap towards achievement of MDGs 4 and 5. Cost Benefit Analysis ( BHU) Baseline @Rs. 240,000 per month Current Running Cost @Rs. 85,000 per month (additional) 1150 400 172 25 ANC 1 40 Delivery 2 76 PNC OPD The manifold improvement in service uptake is due to an innovative implementation model, major factors are pay for performance, provision of free of charge ambulance services and use of E-monitoring and reporting system. Looking at the successful implementation and progress 38 of the pilot project in the seven districts, it is imperative to scale up the venture and spread it across the province, including all the 36 districts of Punjab. It is proposed to scale up the initiatives across the province in phased manner. In year 2013 initially in 16 districts at 300 BHUs , then 200 BHUs in 2014, then 200 BHUs in 2015 and almost all RHCs will be included in this initiative to ensure provision of services to the vast majority of the rural areas. The selection of BHUs will be on the basis of geographical distances, ensuring maximum coverage in each district. 39 PROGRAM COMPONENTS AND DESCRIPTION The proposed program aims at reducing newborn, infant, child mortality and maternal mortality in line with Government’s commitment of achieving health related MDGs. The program has seven main strategic components: 1. Improving Basic and Comprehensive EmONC services at primary and secondary level health care facilities 2. Mainstreaming family planning services and interventions as a maternal health improvement strategy 3. Prevention and management of malnutrition by implementing Pakistan Integrated Nutrition Strategy 4. Strengthening of community-based outreach services focusing on PHC, MNCH, RH/FP and Nutrition through improved performance of LHWs and CMWs 5. Strengthening linkages between community outreach health workers with health facilities 6. Establishing e-monitoring and e-reporting system and a web-based program MIS with linkages to DHIS 7. Strengthening linkages between community and health facilities Each program component is discussed in detail in the following sections of this document. 1. IMPROVING BASIC AND COMPREHENSIVE EMONC SERVICES AT PRIMARY AND SECONDARY LEVEL HEALTH CARE FACILITIES Direct obstetric causes such as postpartum hemorrhage, sepsis and complications of abortion are responsible for close to 50% of maternal deaths. A majority of these maternal and early newborn deaths can be avoided by provision of prenatal, delivery, postnatal and newborn care services within reasonable travel distance& travel time. According to UN process Indicator for a population of 500,000, there must be 4 Basic EmONC facilities and one Comprehensive EmONC health facility. According to an estimated figure, 85 % of the pregnancies end up normally while 15 % of them undergo complications. It is imperative that every district should be mapped accordingly taking into account the problem of scattered population and hard terrain (travel time) at various places and in those cases within a travel time of one hour there must be a Comprehensive EmONC health facility apart from the population size. Under this program all DHQs and 70/84 THQs and selected RHCs (36/297) would be equipped/upgraded to provide Comprehensive EmONC services, while all remaining RHCs and 700/2454 BHUs would provide Basic EmONC services. 40 Key activities: a) b) c) d) e) f) g) h) Availability of minimum agreed staff at the identified health facilities by the year 2013 for provision of 24/7 Basic and Comprehensive EmONC services Availability of logistics, equipment, medicines and supplies for all HF designated for provision of 24/7 Basic and Comprehensive EmONC services Strengthening of neonatal units at the Comprehensive EmONC health Facilities Implementation of MSDS and SOPs relevant to provision of Basic and Comprehensive EmONC services at the health facilities like protocols for antenatal, normal delivery, surgical procedure and postnatal procedures Training &Capacity building of staff at Basic and Comprehensive EmONC facilities on Basic and Comprehensive EmONC, IYCF and Nutrition, IMNCI, ENC, HTSP/FP and Infection Prevention and Control Development and implementation of transport services, including Provision of ambulances at the 24/7 Basic EmONC facilities Ensure availability of POL and other logistics for transport Provision of drivers for ambulances Strengthening of health facilities for the provision of Basic and Comprehensive EmONC services Provision of conducive environment for female HCPs by provision of separate waiting area, wash room and ensuring safety Monitoring and supervision of Health Facilities for the provision of Basic and Comprehensive EmONC services in terms of accessibility, availability and quality of EmONC services Preventive and Basic EmONC Services at BHUs The course of nature gives adequate time of nine months to the woman, family and the healthcare delivery system to timely identify potential risks to mother and child during this normal physiological process, to correct them and to plan for the delivery accordingly. The network of LHWs, CMWs and BHUs working as a team in this program will be enabled to effectively perform these functions through provision of regular antenatal care and advice on nutrition and supplements. The Basic EmONC services include but are not limited to: intravenous and intra-muscular administration of medicines such as antibiotics, oxytocin and anticonvulsants; assisted vaginal delivery; manual removal of placenta; manual removal of retained products of an abortion or miscarriage; and stabilization, referral and transferring the patients of obstetric emergencies not managed at the basic level to referral facility. In terms of newborn care, the required services at the basic EmONC level include resuscitation, management of neonatal infection, very low birth weight infants, complications of birth 41 asphyxia and severe neonatal jaundice. Furthermore, skills and supplies for intravenous fluid therapy, thermal care including radiant warmers, Kangaroo mother care, oxygen supply, parenteral antibiotics, intra-gastric feeding, oral feeding using alternative methods to breast feeding and breast feeding support. Under this program preventive and basic EmONC services will be provided at a total of 700 BHUs (28%) in all 36 districts but with phased manner, to start with 16 districts having poor health indicators will be selected for implementation of a specifically designed less resource intensive package, replicating the CHARM model. Selection of BHUs for Basic EmONC Services The selection of 28% BHUs (700 BHUs) will be done on the basis of geographical spread, distance from existing basic and comprehensive EmONC facilities, accessible by the community and secure for female staff and patients during evening and night rotations. The notified Provincial Management Committee will determine selection of BHUs for program implementation. Table 1 below shows program implementation in a phased manner. 42 Year Wise Implementation of Phasing 24/7 EmONC facilities Phase 1 Implementation of 24/7 in Phasing in 2013-14 Phase 2 Implementation of 24/7 in Phasing in 2014-15 Sr. NO 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Total Sr. NO 1 2 3 4 5 6 7 8 9 District Rajanpur DG Khan Muzafargarh Bahawalpur Bahawalnagar Rahim Yar Khan Khanewal Layyah Bhakkar Narowal Pakpatan Hafizabad Sargodha Mianwali Multan Jhung District Faisalabad Lahore Rawalpinidi Sialkot Khushab Chakwal Vehari T. T. Singh Sahiwal Total Sr. District NO 1 Attock 2 Chiniot 3 Gujrat 4 Jhang 5 Jhelum Implementation of 24/7 in Phasing in 6 Kasur 2015-16 7 Lodhran 8 Naknaka 9 Okara 10 Sheikhupura 11 M. B. Din Total Grand Total Phase 3 12 6 10 7 5 9 14 6 10 Total BHU 31 52 71 73 103 104 82 40 40 56 53 32 122 40 77 58 1064 Total BHU 168 36 98 88 41 65 74 66 76 24/7 BHU 15 16 21 22 31 31 23 12 10 16 15 11 30 11 18 16 300 24/7 BHU 47 10 27 25 11 19 21 18 21 26 79 712 200 DHQ THQ RHC 1 1 1 1 1 1 1 1 2 1 1 12 34 5 2 1 2 2 2 2 0 2 1 1 20 84 5 3 10 9 5 12 4 7 10 9 9 83 295 Total BHU 60 36 90 58 45 82 48 48 96 79 49 691 2467 24/7 BHU 17 10 26 17 13 24 14 14 28 23 14 200 700 DHQ THQ RHC 1 1 1 1 1 0 1 1 1 1 1 1 1 1 0 1 14 2 1 2 4 4 3 3 3 3 1 1 1 4 1 2 2 38 6 9 13 10 10 19 4 4 3 7 4 5 14 9 7 9 133 DHQ THQ RHC 0 1 0 2 1 1 1 1 1 5 2 4 3 3 3 2 2 2 8 SBA Rate 17 26 36 37 42 44 49 49 50 55 57 70 61 65 65 52 SBA Rate 70 82 79 72 61 75 50 58 26 SBA Rate 61 58 73 52 80 53 43 60 51 65 52 43 Human Resource Requirement &Staff Incentives at BHU The already appointed staff at BHUs i.e., health officer, LHV, midwife and dispenser will be given financial incentives to ensure 24/7 preventive and basic EmONC services. In addition, to ensure basic EmONC services on 24/7 basis, skilled birth attendants, aya, Guards and driver will be appointed on contract basis to complement the efforts of existing facility staff at selected BHUs. It will be ensured that each health facility has at least 4 skilled birth attendants deployed, one for each of the three shifts and one as a reliever. In case of overburdened health facilities, a fifth SBA maybe appointed for additional support during the morning shift only. Equipment & Supplies The equipment and supplies required to ensure preventive and refined basic EmONC package include contraceptives, medicines, IMNCI package of medicines, basic newborn care kit, clean delivery kits, and other basic equipment. Physical Infrastructure At BHUs no additional construction will be required as most of the BHUs are already renovated under health sector reform program in Punjab. However, minor repairs may be required for delivery rooms, and LHV and midwife residences. Basic & Comprehensive EmONC Services at RHCs This program proposes to ensure complete package of basic EmONC services at all the RHCs and comprehensive EmONC at 36 RHCs (15%) in the province. Basic EmONC at RHCs The program proposes to provide basic EmONC services at each of 297 RHC on 24/7 basis. This will be done by ensuring the presence of existing HR. The 162 RHCs that come within the 20 low indicator districts may be provided temporary support in the form of missing equipment and/or supplies, etc. on a need basis as identified by the DHMT. However, efforts will be made to ensure the availability of services from the existing budget and resources allocated for the RHCs by the Department of Health through the DHMT and the PHSRP. Human Resource Requirement The existing staff will be trained in provision of EmONC services. The requirement of additional staff may be fulfilled through temporary contract on a need basis. Physical Infrastructure The provision of basic EmONC services in the facility requires a functioning labor room/operation theater and indoor ward. The RHCs may be provided with funds for minor repairs but not for new construction. Most of the RHCs already have provision for 20 beds for treatment of indoor patients, an operation theater, laboratory and X-ray facility. 44 Equipment and Supplies The equipment and supplies required to ensure basic EmONC package at RHCs include laboratory support and equipment for a minor operation theatre. The supplies include contraceptives, medicines, IMNCI package of medicines, basic newborn care kit, clean delivery kits, and other basic equipment. Comprehensive EmONC at Selected RHCs The Comprehensive EmONC Services include all of the services provided at the basic level, in addition to cesarean section, blood transfusion services and newborn special care. In case of acute obstetric emergency, the case may be referred to DHQ hospital. Human Resource Requirement and Strategy In addition to staff required to ensure basic EmONC services at RHCs, some additional staff will be required to provide comprehensive EmONC services at selected RHCs or existing staff may be trained. The program proposes following ways to engage professionals in provision of comprehensive EmONC services at selected RHCs: i. Engaging public sector specialists on need basis: The specialists working at THQ and DHQ hospitals may be called on need basis on as and when required. They may be compensated on a case to case basis on already agreed upon terms and conditions. ii. Engaging private sector specialists on need basis: The specialists practicing nearby may be contracted to provide services on as and when required basis on mutually agreed upon terms and conditions. They shall be paid on market rates for their services. iii. Appointment of postgraduate trainees at RHCs, THQs and DHQs on rotation basis. iv. The attachment of RHC staff for hands on training in gynecology, anesthesia, pediatrics and neonatology. The program will ensure services of specialists through implementing a mix of these strategies or developing another more workable strategy for the purpose. The lab technician will be trained in blood transfusion techniques and relevant equipment will be made available at each of 36 RHCs. Equipment and Supplies The equipment and supplies required to ensure comprehensive EmONC package at RHCs include laboratory support, blood transfusion services, and equipment for operation theatre and a functioning ambulance/vehicle. The supplies include contraceptives, medicines, IMNCI package of medicines, newborn care kit, clean delivery kits, and other basic equipment. 45 Physical Infrastructure The provision of comprehensive EmONC services in the facility requires a functional labor room/operation theater and inpatient ward. The RHCs will be provided with funds for minor repairs and not for new construction. Most of the RHCs have provision for 20 beds for treatment of indoor patients, an operation theater, laboratory and X-ray facility. At each of these RHCs beds will be allocated for EmONC services in the inpatient wards. Comprehensive EmONC Services at THQ and DHQ Hospitals This program proposes that at each of 80 THQ and 35 DHQ hospitals in Punjab, complete package of comprehensive EmONC services shall be offered. At THQs and DHQs the referrals from BHUs and RHCs as well as from the field will be catered for. Human Resource Requirement and Strategy In order to ensure comprehensive EmONC services at THQ and DHQ hospitals, no additional staff will be required. However the gynecologist, anesthetist and pediatrician may not be available at all the THQs and DHQs in the province. The program proposes similar ways to engage these specialists as are suggested above under human resource requirement for RHCs. The program will ensure services of specialists through implementing a mix of these strategies or developing other workable strategies for the purpose. Equipment and Supplies The hospitals in Punjab have a majority of equipment available for EmONC services therefore only some additional equipment will be provided to these hospitals. The THQ and DHQ hospitals will be dealt with on a case to case basis. It is also proposed to provide these hospitals with incinerators for adequate disposal of hospital wastes through the Hepatitis control program. However for chemical disposal of hospital waste the recurrent costs shall be met from the regular budget of the hospital. All hospitals will need to be equipped with laboratory support, X-ray, Blood Bank, Operation Theatre and Anesthesia facilities. The list of equipment (Table 8) covers all the essential equipment for DHQ/THQ hospitals for comprehensive EmONC services. It is anticipated that majority of the THQ and DHQ hospitals would not require complete set of equipment, as it is provided through regular provincial budget and other sources. Similarly, the hospitals will conduct a review of available equipment in comparison with the list of equipment proposed and categorize it into three parts i.e., available and functional, available but repairable, and not functional/available and required. It is envisaged that this exercise should not take more than three months to complete and the detailed compilation of this information should be available with the district program 46 management unit and then with the program management unit within six months of launch of the program. The equipment will be provided under warranty and service contract will be made with the supplier to perform at least one maintenance visit every four-six months. Provision has been made for service contracts for electrical equipment. Physical Infrastructure The infrastructure at the THQ and DHQ hospitals has sufficient capacity to enable provision of EmONC services. These facilities have recently undergone repairs therefore it is anticipated that immediate repairs will not be required. However the need for minor repairs and maintenance may be carried out from District Government funds. 47 Table 2 List of equipment for DHQ and hospitals providing comprehensive EmONC services Pediatric Ward Gynae/Obst. Ward Items Pediatric Nursery Medical equipment General Equipment Neonatal Resuscitation Suction machine Air conditioner Mucus extractor disposable Infant BP apparatus (Cuff 2.5 cm) Cabinet Instrument large Infant face mask (2 different sizes-each) Stethoscope Pediatric Littman type Fowler bed (Iron ) Infant ambo bag Nebulizer Refrigerator 10 cubit Suction catheter Ch10 &12 Oxygen cylinder complete Screen folding complete Infant laryngoscope Glucometer Weight machine adult Endotracheal tubes no. 3.5 Infusion pump Medical Equipment Suction apparatus: Ophthalmoscope Artery forceps 7 inch Miscellaneous equipment Emergency medicine trolley B P Apparatus mercury – Desk type Infant Incubators Pulse oxymeter Dissecting forceps plain 7 inch Phototherapy unit Lumber puncture Kit Fetal Monitor Baby Resuscitation Kit Disposable syringe cutter Infant B.P apparatus& weight machine Disposable oxygen mask Disposable syringe cutter Baby cot ē heating facility Perineal/Vaginal/Cervical Repair Furniture Baby warmer Sponge forceps Baby Cot Operation Theatre Needle holder Infant BP apparatus (Cuff 2.5 cm) Labour Room UPS power supply system Stitch scissors General Equipment Air conditioner ē heating system Dissecting forceps, toothed UPS power supply unit Room thermometer Sim's speculum large& medium Basic Equipment Disposable syringe cutter Vacuum Extraction or Forceps Delivery Infant weight machine Baby cot Vacuum extractor Fetal stethoscope Steam inhaler Obstetric forceps Electric instrument sterilizer 12 x 6 Obstetric Laparotomy/Caesarean Section Jar for forceps General Equipment Rectangular instrument tray ē lids Spring type dressing forceps (ss) Refrigerator 10 cbft Towel clips Insertion and Removal of IUD Air conditioner Sponge forceps, 22.5 cm Sim's Speculum right angle, small, medium Miscellaneous equipment Straight artery forceps, 16 cm Sim's Speculum right angle, large Incubator Uterine hemostasis forceps, 20 cm Sponge forceps Spin Machine Hysterectomy forceps, straight, 22.5 cm Long straight artery forceps Chemistry Analyzer Mosquito forceps, 12.5 cm Uterine sound Water Distillation unit Tissue forceps, 19 cm Vulsellum forceps Hematology analyzer Needle holder, straight, 17.5 cm Scissors dissecting blunt pointed Computer System with UPS+Printer Surgical knife handle& blades Normal Vaginal Delivery Furniture Triangular point suture needles Artery forceps Steel Almirah large& Lab cabinet Round-bodied needles No. 12, size 6 Blunt-ended scissors General Hospital Equipment Abdominal retractors, Neonatal Resuscitation Defibrillator Curved & straight operating scissors, Mucus extractor UPS power supply system Anesthesia Infant face mask (2 different sizes) Computer system ē UPS& printer Anesthetic face masks Infant ambo bag Electric Water Cooler ē water filter Anesthesia Machine Suction catheter Ch10 &12 Power Generator 50 Kva (Diesel), or Laryngoscopes Miscellaneous equipment OPD / Gynecologist office Epidural sets ECG Machine General Equipment Miscellaneous Equipment Portable Light ē rechargeable batteries (OT) Weight machine adult& infant X-Ray illuminator Sterilizing Drum Screen folding complete General &Gynae Instrument set Vacuum Extractor Ultrasound machine Adult ambo bag and mask Pulse oxymeter Miscellaneous equipment D & C instruments set C.T.G. machine Steam inhaler& nebulizer Air conditioners Laboratory Examination lamp 48 Strengthen Specialized Services at RHCs, THQs and DHQs The targets of MDGs and ensuring services to improve communities’ health will be hard to achieve if the specialized services, specifically in gynecology, anesthesia and neonatology, are not made available at health facilities which are set to providing comprehensive EmONC. This program proposes following strategies to strengthen specialized services at RHCs, THQ and DHQ hospitals: i. Attachment of doctors from RHC, THQ and DHQ hospitals at tertiary hospitals specifically for gynecology, anesthesia and neonatology training; ii. Appointment of post graduate trainees at RHCs, THQ and DHQ hospitals for threemonths on rotation basis through an institutionalized mechanism; iii. Engaging private sector specialists in providing services on need basis at RHC, THQ and DHQ hospitals; Each of these strategies is discussed in the following paragraphs. Attachment of Doctors from RHCs, THQs &DHQs at Tertiary Hospitals Table3:Distribution of trainees by hospital S # Health Facility No Trainees 1 RHC 2 2 THQ Hospital 3 3 DHQ Hospital 4 Total Total Trainees Keeping in view the paucity of 578 avenues for practical training and 240 an expected delay/ shortfall in 140 958 finding the number of specialists required at the facilities providing comprehensive EmONC services, a short term proposed solution is to train the doctors already working at these facilities. For each facility being setup for Comprehensive EmONC services, it is proposed that one to three woman medical officers may be trained in Obstetrics (C-section), two woman medical officers or medical officers in pediatrics/neonatology and one medical officers in anesthesia and one additional according to the need of the hospital. It is estimated that a total of 958 doctors will be trained (Table 3). For facilities providing Basic EmONC services it is proposed to train two woman medical officers in obstetrics and one to two medical officers in pediatrics/neonatology. These trainings can be imparted by providing three months attachment at the nearest teaching hospital or at a DHQ hospital having a qualified specialist. These trainees shall be entitled for an allowance of Rs 15,000 per month for the period of attachment. The lodging should be arranged by the program, preferably at doctors’ hostels, for the length of training period. The trainer shall be entitled for an allowance of Rs. 40,000 per month for a group of 5-7 trainees. This means each trainer will receive an allowance of Rs. 120,000 for training 5-7 49 doctors in their respective specialties for three months against minimum acceptable targets set for trainers. The selection of doctors for this training program will be done by the respective hospital in consultation with district program management unit and EDO (H) and approved by provincial program management units. The minimum criteria shall include six months service at that hospital and a commitment to continue working after the training for at least 2 years. It is proposed that a mechanism should be developed and institutionalized with College of Physicians and Surgeons of Pakistan (CPSP) to recognize this period in regular PG training afterwards. Each district program management unit (DMU) will figure out its requirements for staff and will make a yearly plan in coordination with EDO (H). The plan will be submitted to provincial program management unit (PMU). The PMU will consolidate district requirements and will arrange for training of doctors from the districts in coordination with health department and teaching hospitals. This component shall be operational within six months of commencement of the program. Rotation of Post Graduate Students in Institutionalized Manner In majority of the DHQ and THQ hospitals the specialists staff positions can be supplemented by appointment of post graduate (PG) students in specialties of gynecology, anesthesia and neonatology on a three-month rotation basis at these hospitals.The PG students will be given an additional incentive of Rs. 20,000 per month for working in addition to their regular remunerations. It is proposed to develop institutionalized mechanism within the health system by the Government of Punjab with the CPSP to regularize this three-month rotational appointment as a compulsory part of the post graduate training during their third and fourth years of training. At RHC, THQ and DHQ hospitals the PG trainees will be provided with decent accommodation from respective hospital resources. Each district program management unit (DMU) will figure out its requirements for specialist service and will make a yearly plan in coordination with EDO (H). The plan will be submitted to provincial program management unit (PMU). The PMU will consolidate district requirements and will arrange for appointment of PG trainees in coordination with health department and teaching hospitals. This program component shall be operational within one year of commencement of program. Engaging Local Private Sector Specialists In areas where specialists are practicing locally in the private sector they may be engaged to provide services at Government health facilities on need basis. The terms and conditions may be developed and finalized which will include a retainer fee and service fee. For example if at a THQ anesthetist is not available however there is one practicing in the private sector S/he will be engaged to provide services at THQ on as and when required and 50 priority basis. For these services s/he will be paid a retainer fee of Rs 20,000 per month so that his/her availability on priority basis could be ensured. In addition he will be paid a service fee on case to case basis for providing anesthetist services. It is estimated that specialist services through private sector specialists will be required at 10% of total health facilities. Each district program management unit (DMU) will figure out its requirements for specialist services through private sector and will make a yearly plan in coordination with EDO (H). The plan will be submitted to provincial program management unit (PMU). The PMU will consolidate district requirements and will arrange for appointment of private sector specialists in coordination with health department. This program component shall be operational within one year of commencement of program. Establish Referral System The establishment of a functional and efficient referral system is considered as the key to ensuring adequate access to healthcare delivery services for the program area population. Under this program, the referral system will be established through creating functional links between ‘Household-Outreach staff-BHU-RHC-THQ-DHQ’ i.e., linking all health service providers and services operating at various levels of health care delivery system. The Government of Punjab will notify the implementation of referral system and roles and responsibilities of health care providers at various levels of the service provision. The referral system will essentially have four functional levels of referral system: 1. First Level: Household to CMW and BHU 2. Second Level: BHU to RHC and THQ Hospital 3. Third Level: RHC to THQ and DHQ Hospital; and 4. Fourth Level: THQ to DHQ and Tertiary Care Hospital The functioning of these levels is described in detail in the following paragraphs. First Level of Referral System – “Household – BHU” At the household level, this program has community based staff members i.e., LHW, CMW and LHS. Each household is registered with the respective LHW as well as with the BHU. Each LHW is linked with CMW and the BHU. Moreover each CMW is linked with LHS and the BHU. Therefore each household is functionally connected with the BHU in case a referral is made by the LHW or CMW. The LHW, CMW and the BHU i.e., the primary functionaries of PHC system constitute the first level of referral system for the population residing within the catchment area of a BHU. 51 In order to establish functional first level of referral system, the program will take the following essential steps: 1. Each LHW, being the first direct link between the health care delivery system and the household, will have a detailed knowledge of services being provided by the CMW of her area and the BHU. She will have a chart displayed at her health house showing this information. This chart will be modified with any change in services, even if that occurs for a short duration. For example if the LHV at BHU proceeds on leave for two months or has been transferred without any replacement or has resigned, the chart will be accordingly modified. Such changes will be timely conveyed to all LHS for onward transferring of this information to LHWs and CMWs. 2. The LHW will refer cases to CMW or BHU that are beyond her capacity on prescribed “LHW Referral Form”. She, for example, will refer pregnant women for antenatal, natal and postnatal care to CMWs; 3. On receiving a referral from the LHW, the CMW providing services will give feedback to LHW on the same referral form; 4. Similarly the health care provider at BHU, on receiving referrals from LHWs or CMWs, will provide feedback to respective LHW or CMW. 5. This communication between referring and referral facilities will be part of records at corresponding levels of the referral system. Second Level of Referral System – “BHU – RHC & THQ” The second level of referral system will be established between BHU and RHC/THQ level. The patients presented at or referred to BHU will be managed at that facility or will be referred to RHC or THQ depending upon the nature of requirement. The health care providers at BHU i.e., health officer, LHV, medical technicians and dispenser and health care providers at RHC and THQ constitute the second level of referral system. In order to establish functional second level of referral system, the program will take the following essential steps: 1. The health care providers at BHU will have detailed knowledge of services being provided by the RHC and THQ hospital. Each BHU will have a chart displayed showing this important information. This chart will be modified with any change in services at RHC and THQ hospital, even if that occurs for a short duration. For example if a gynecologist deputed at RHC or working at THQ proceeds on leave for two months or has been transferred without any replacement or has resigned, the chart will be accordingly modified. Such changes will be timely conveyed to all concerned levels of health facilities; 2. The BHU will refer patients to RHC or THQ hospital that are beyond its capacity on prescribed “BHU Referral Form”; 52 3. On receiving a referral from BHU, the health care providers at referral facility i.e., RHC or THQ after providing services will give feedback to the BHU on the same referral form. 4. This communication between referring and referral facilities will be part of records at the corresponding levels of the referral system. Third Level of Referral System – “RHC – THQ& DHQ” The third level of referral system will be established between RHC and THQ/DHQ level. The patients presented at or referred to RHC will be managed at that facility or will be referred to THQ or DHQ depending upon the nature of requirement. The health care providers at RHC i.e., health officer, woman medical officer, LHV, nurse, medical technician and dispenser and the health care providers at THQ and DHQ constitute the third level of referral system. In order to establish functional third level of referral system, the program will take the following essential steps: 1. The health care providers at RHC will have detailed knowledge of services being provided by the THQ and DHQ hospitals. Each RHC will have a chart displayed showing this important information. This chart will be modified with any change in services that takes place at THQ and DHQ hospitals, even if that occurs for short duration. For example if a surgeon deputed at THQ or working at DHQ proceeds on leave for two months or has been transferred without any replacement or has resigned, the chart will be accordingly modified. Such changes will be timely conveyed to all concerned levels of health facilities; 2. The RHC will refer patients to THQ and DHQ hospitals that are beyond its capacity on prescribed “RHC Referral Form”. If that patient is already referred from BHU on BHU Referral Form, that will be attached to RHC referral form; 3. On receiving a referral from RHC, the health care providers at referral facility i.e., THQ and DHQ hospitals will provide feedback to RHC on the same referral form. 4. This communication between referring and referral facilities will be part of records at corresponding levels of the referral system. Fourth Level of Referral System – “THQ – DHQ& Tertiary Care Hospital” The fourth level of the referral system will be established between THQ and DHQ/Tertiary Care Hospital. The patients presented at or referred to THQ will be managed at that facility or will be referred to DHQ or Tertiary Care Hospital depending upon the nature of requirement. The health care providers at THQ and the health care providers at DHQ and Tertiary Care Hospital constitute the fourth level of referral system. In order to establish functional fourth level of referral system, the program will take the following essential steps: 1. The health care providers at THQ will have detailed knowledge of services being provided by the DHQ and Tertiary Care Hospital. Each THQ will have a chart displayed on at least 53 two places showing this important information. This chart will be modified with any change in services that takes place at DHQ or Tertiary Care Hospital, even if that occurs for short duration. For example if a neurosurgeon working at Tertiary Care Hospital proceeds on leave for two months or has been transferred without any replacement or has resigned, the chart will be accordingly modified. Such changes will be timely conveyed to all concerned levels of health facilities; 2. The THQ will refer all those patients to DHQ or Tertiary Care Hospital that are beyond its capacity on prescribed “THQ Referral Form”. If that patient is already referred from BHU and/or RHC on Referral Form, that/those will be attached to THQ referral form; 3. The DHQ will refer all those patients to Tertiary Care Hospital that are beyond its capacity on prescribed “DHQ Referral Form”. If that patient is already referred from BHU, RHC and/or THQ on Referral Form, that/those will be attached to DHQ referral form; 4. On receiving a referral from THQ, the health care providers at referral facility i.e., DHQ and Tertiary Care Hospital will provide feedback to referring facility on the same referral form. 5. This communications between referring and referral facilities will be part of records at corresponding levels of the referral system. Performance Incentives Honorarium/bonus will be admissible to the Officers and support staff of the program on recommendations of the Steering Committee. This will create a sense of competition and aid in effective implementation of the program strategies. The PMU, through a consultancy, will define deliverables for facility based staff which will be measurable along with performance indicators. These will determine incentives for facility-staff. Quality of work will have important bearing on these bonuses. Based on the results performance incentives will be given to provincial and district program managers on achievement of performance targets. 54 2. MAINSTREAMING FAMILY PLANNING SERVICES AND INTERVENTIONS AS A STRATEGY TO IMPROVE MATERNAL HEALTH Birth Spacing or Family Planning is one of the most important and cost effective preventive health interventions for reducing maternal, child and neonatal mortality. Voluntary family planning is recognized as the only acceptable means of regaining proper balance between fertility and mortality. The imbalance between these two, i.e., high fertility and declining mortality leads to excessive population growth. Pakistan is facing the same situation which has become a barrier in economic growth of the country. Despite tremendous investments, the child spacing could not become part of our family life because of poor quality and inaccessibility of services, lack of effective communication policy and its patch implementation, fear of side effects, religious and cultural misperceptions. Moreover instead of understanding ‘child spacing’ the major focus has been given to making services available. Currently, there is almost 18% unmet need for FP services. The social marketing in urban and semi-urban areas and LHWs’ program in the rural areas are the major interventions for increasing contraceptive prevalence rate in the country. There are about 4,000 health facilities in the Punjab but their share in provision of family planning services is generally less than 1%. The current facilities offering family planning services are generally underutilized. For instance, one evaluation showed that, on an average, a family welfare center received only 2 clients per day13. One reason for this is the limited access of Pakistani women to health or family planning services. There are many ways to expand access beyond static clinics and, over the past 30 years, many of them have been tried in Pakistan. The training of traditional birth attendants, or dais, has been tried on many occasions in South Asia, but their low social status prevents them from being plausible agents of social change, and their impact on family planning has been negligible. All health facilities would be equipped to provide a full range of contraceptive and follow up services. Surgical contraception would be provided at the Comprehensive EmONC facilities. Capacity building of staff of all Comprehensive and Basic EmONC facilities would be done in FP, HTSP, Postpartum FP and Supply Chain management system. At grassroots level LHWs and CMWs have been providing FP services and data of the community based workers will be consolidated and integrated at the BHU level. These community based workers of health and PWD would refer the clients to the most appropriate health facilities if required. Unmet need can be decreased and CPR can be greatly enhanced if both health and PWD would work in close collaboration with one another at micro, meso and macro level. The following activities will be undertaken to address FP services as an integrated strategy to address maternal health 13 Cernada GP, Rob AKU, Ameen SI, Ahmad MS. A Situation Analysis of Family Welfare Centers in Pakistan.Islamabad, Pakistan: Population Council; 1993. 55 a) b) c) d) e) Linkages building with PWD at all levels including UC, district and provincial level Ensure un-interrupted provision of FP supplies to health facilities, CMWs and LHWs by putting in place an effective Supply Chain Management System Capacity building of LHWs, CMWs and health facility staff on HTSP, PPFP counseling and skills Integrated MIS regarding FP data at the community and facility level Regular District Technical Committee Meeting (DTC) on monthly basis Under the proposed program, efforts would be made to ensure that preferably all health facilities are providing maximum range of family planning services for HTSP. The program will meet all logistics and training needs. a. Strategy Healthy Timing and Spacing of Pregnancy (HTSP) strategy will be adopted at community and facility-based level. b. Interventions and Targets In order to achieve its objectives, the program will have the following interventions and targets: 1. Training of 4,000 health care providers in birth spacing counseling techniques; 2. Ensuring surgical contraception services at all RHCs, THQ and DHQ hospitals; 3. Ensuring availability of at least three month stock of contraceptives at minimally 80% of health facilities; 4. Ensuring reduction in stock outs of contraceptives at BHUs to less than 20%; 5. Ensuring availability of LHVs at all DHQ, THQ and RHC and at least 90% of BHUs; c. Essential Components of Birth Spacing Services In order to achieve its birth spacing objectives, the program will need to have the following essential components: 1. Ensuring Multi-sectoral Participation: The program will need to combine the efforts of Government, NGOs, social marketing, private sector and international partners; 2. Presentation as Health Intervention: In program’s communication strategy, the birth spacing will be presented as health intervention with carefully developed concept and wording; 3. Broad Range of Service Outlets: The birth spacing services will be made available at wide range of outlets including Government, NGOs, private clinics, pharmacies and community workers; 56 4. Inclusion in Postpartum Care: The postpartum period is the most appropriate timeframe during which birth spacing counseling and provision of supplies can achieve tremendous and efficient results. d. Trainings on Birth Spacing Counseling The program plans to train all the health facility staff on birth spacing counseling. A manual will be developed for this purpose. The trainings will be held in collaboration with Regional Training Institutes wherever possible. The training process will be of the cascade type: first a batch of provincial master trainers will be trained. These will train district master trainers, preferably from the DHQ hospitals, who will impart training to the staff of the health facilities i.e., DHQ, THQ, RHC and BHU. Before the commencement of the training cascade, a two day orientation and planning workshop at the provincial level will be conducted. The list of available facilitators from each district will be discussed and availability of training aids at different training sites will be reviewed. According to the training plan decided at the provincial level the training cascade will be initiated, and adhered to. The first workshop will be of 10 participants at the provincial level with facilitation from a team of experts. These trainers will then hold district training workshops for staff of DHQ hospital, from where district trainers will be identified to impart training to the rest of the health facilities in the district. The staff to be trained at the DHQ and THQ will include: WMO, MO, LHV, and other technical staff involved in provision of birth spacing services. At the RHC and BHU the WMO, MO, LHV, FMT, Dispenser, MT and other technical staff involved in provision of birth spacing services will be trained. The total number of facility staff to be trained is envisaged to be around 4,000, with each of the training proposed to be of 3 working days. e. Trainings on Surgical Contraceptive Techniques Three staff members from each health facility providing EmONC (comprehensive or basic) shall be trained in surgical contraceptive techniques. The trainings shall take place at regional training institutes (RTI centers). 57 3. PREVENTION AND MANAGEMENT OF MALNUTRITION BY IMPLEMENTING PAKISTAN INTEGRATED NUTRITION STRATEGY The findings of the 2011 National Nutrition Survey reveal a very grave picture of Punjab showing prevalence of chronic malnutrition among children under-5 years of age at 39.2 % and maternal anemia at 49.6%. Similarly the prevalence of acute malnutrition among children is 13.7% and child anemia in Punjab is 60.4%. (NNS 2011) The Punjab Policy guidance note on Nutrition shows that there is a strong association between factors such as poverty and women’s education and malnutrition. Special efforts will thus be made to reach the poorest households and the communication for behavior change will be designed in a way to effectively communicate with illiterate and less educated mothers. The NNS data reflect the abysmal condition of nutrition among the more vulnerable segments of the population, which include women and children of the province. Such indicators on the part of the provincial health department also warrant a comprehensive and effective plan of action on a war footing, to improve the existing deplorable health conditions and indictors for the women and children. The integrated nutrition strategy will be implemented in districts having poor indicators related to nutrition and health. A comprehensive nutrition strategy will be implemented to address malnutrition through preventive and curative services. The preventive nutrition interventions are being proposed for all 36 districts; additionally, curative component addressing severely acute malnutrition is proposed for 12 priority Districts and urban peripheries of 9 mega-Districts of Punjab in the first phase. Then phase wise extension is also proposed for Curative component to address severely acute Malnutrition throughout the province. It is proposed to implement Nutrition activities especially curative services in a phased manner. This will not only help in testing ease of implementation and identify bottlenecks but will also provide an opportunity for piloting some of the interventions before their scale up through subsequent PC-1s. Preventive services will be implemented in all 36 districts through advocacy and Communitybased Nutrition services. The Nutrition Initiative has been developed to provide benefit to the entire population of the province with the introduction of proven, cost-effective interventions. The undertaking within this program includes implementation of a province-wide Nutrition Education Package with an aim to enhance knowledge within the community about nutrition and alter behaviors and practices which hinder improved nutrition. This will help create linkages between health, hygiene and immunization and will serve to improve health systems’ efforts to address malnutrition. This component will focus on prevention of malnutrition among the general population, with particular focus on pregnant and lactating women and under 5 children and adolescent girls. 58 Capitalizing latest research findings on impact of maternal nutrition on child nutrition, the 1000+ days approach, with focus on the period of the life cycle from conception till the first 24 months of the child’s life (when irreversible damage from malnutrition is likely to occur), will be utilized. It is envisaged that by focusing on maternal health both before and during pregnancy through integrated nutrition and reproductive health interventions, improved maternal and neonatal nutritional and survival outcomes will be realized. The nutrition package will include nutrition education campaign, community based IYCF activities (counseling for breastfeeding and adequate complementary feeding). Provision of iron and folic acid tablets to adolescent girls, with particular focus on pregnant and lactating mothers, Biannual de-worming of children Vitamin A supplementation for children will be continued, with a focus on improving performance in lower performing areas. Zinc supplementation will also be provided and advocated with ORS as treatment of diarrhea. Provision of MMS to MAM children Advocacy with policy makers and legislating bodies for compulsory fortification of food will also be part of this component. Curative/Therapeutic Nutrition interventions This component will be implemented in a phased manner, addressing those most marginalized and poorest sections of society within rural and peri-urban areas. The first phase will include 12 districts having poor nutrition indicators and urban slums of 9 mega districts. In the 2nd and 3rdphases, therapeutic nutrition services will be extended to all 36 Districts. Proposed activities include: Treatment of Severely Acute Malnourished children (SAM) with Ready to Use Therapeutic Food (RUTF). Treatment of SAM with complications at Stabilization Centers (SC) in all 36 districts of Punjab Treatment of moderately acute malnourished pregnant and lactating women (MAM PLWS) and moderately acute malnourished (MAM) children through provision of supplementary food with the support of WFP and UNICEF will be part of program in District Rajan Pur and D.G. Khan only. 59 IMPLEMENTATION OF NUTRITION PROGRAM IN PHASING Sr.No 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 2013-14 Narowal Layyah Mianwali Multan Khushab Rahimyar Khan Pakpattan D. G. Khan Muzaffargarh Bhakkar Rajanpur Bhawal Nagar Gujranwala Sargodha Rawalpindi Faisalabad Bhawal Pur Sahiwal Khanewal Sialkot Lahore 2014-15 Narowal Layyah Mianwali Multan Khushab Rahimyar Khan Pakpattan D. G. Khan Muzaffargarh Bhakkar Rajanpur Bhawal Nagar Gujranwala Sargodha Rawalpindi Faisalabad Bhawal Pur Sahiwal Attock Chiniot Gujrat Hafizabad Jhang Jhelum Kasur Khanewal Lodhran Vehari Sialkot Lahore 2015-16 Narowal Layyah Mianwali Multan Khushab Rahimyar Khan Pakpattan D. G. Khan Muzaffargarh Bhakkar Rajanpur Bhawal Nagar Gujranwala Sargodha Rawalpindi Faisalabad Bhawal Pur Sahiwal Attock Chiniot Gujrat Hafizabad Jhang Jhelum Kasur Khanewal Lodhran M.B. Din Chakwal Nankana Sahib Okara Sheikhupura T.T. Singh Vehari Sialkot Lahore 60 Implementation Strategies The proposed program aims at reducing maternal and child malnutrition in line with Government’s commitment of achieving health related MDGs through: a) a) Strengthening of community outreach services focusing on Nutrition Education Package through training &improved performance of LHWs. b) Prevention and management of malnutrition by providing community outreach and facility based services c) Addressing Micronutrient Malnutrition Strengthening of community outreach services focusing on Nutrition including MNCH/RH and FP through improved capacity building and performance of LHWs LHWS will be fully trained on the Nutrition Education Package including IYCF, micronutrient deficiency and WASH messages. This preventive Nutrition Education Package will be used for awareness raising and promoting healthy behaviors among the population, especially, women, children and adolescent girls. Additionally, in areas where the Therapeutic component will be undertaken, LHWs will be strengthening the Nutrition program through effective screening, referral and followup. LHWs will screen, refer and follow up pregnant and lactating women and malnourished children to the health facility for nutrition services. Key Interventions Provision of Logistics and Equipment o Provision of iron and folic acid tablets, zinc syrup , ORS, RUTF and micronutrient sachet to LHWs o Weighing scale (Salter) o Provision of MUAC tapes, height & length board Strengthening of Monitoring and Supervision of CMWs and LHWs o Capacity building of LHSs on supervision of CMAM and IYCF activities of LHWs o Monthly reporting of screening, referrals and follow-ups. o Monitoring visits to all LHWs by LHS at least once a month o Off and on Monitoring visit to all LHWs by the District Nutrition focal person o Development of E-monitoring and reporting through SMS based system 61 Establishment of Multi sectoral Coordination Committees at provincial, district and union council levels Membership for the Provincial Malnutrition Eradication committee includes: i. Department of Health ii. Food Department iii. Agriculture Department iv. Livestock Department v. Education Department Membership for the District Malnutrition Eradication committee includes: i. Department of Health ii. Food Department iii. Agriculture Department iv. Livestock Department v. Education Department Membership for the Union Council Malnutrition Eradication committee includes: i. School health nutrition supervisor (convener ) ii. LHS iii. UC Secretary iv. Representatives of agriculture, livestock and education departments 62 b) Prevention and management of malnutrition by providing community outreach and facility based services Therapeutic/Curative Nutrition along with Preventive services will be provided in 12 districts and 9 peri-urban areas of mega-districts. Two intervention arms are being implemented in these districts; in Districts DG Khan and Rajanpur treatment of SAM and MAM children and MAM PLWs will be undertaken, in other districts, only treatment of SAM children with and without complications will be undertaken. Key Activities: 1. Facility based CMAM (Community based Management of Acute Malnutrition) in Districts DG Khan and Rajanpur Provision of supplementary foods for distribution among identified cases will be supported by WFP and UNICEF. The following commodities will be used for treatment of identified cases a. Supplementary Feeding Program i. Provision of Fortified Blended Food (FBF) to MAM PLWs ii. Provision of Micro nutrient tablets to MAM PLWs iii. Provision of RUSF (Ready to Use Supplementary Food) for MAM Children 6-59 months in two districts iv. Provision of High Energy Biscuits (HEB) to siblings of identified SAM & MAM children v. Provision of Micronutrient sachet to MAM children and vi. Provision of Nutrition advocacy package (IYCF, immunization Wash, Fortification) b. Outpatient Therapeutic Program (OTP) i. Provision of RUTF (Ready to Use Therapeutic Food) to SAM children without complication ii. Provision of Nutrition advocacy package (IYCF, immunization Wash, Fortification) c. Stabilization Centers at DHQHs and teaching hospitals. I. Provision of F75, F100 and advised medicines to SAM children with medical complication 63 Recruitment and training of human resource for implementation of the above activities includes: 1. 51 Nutrition Assistants in Districts DG Khan and Rajanpur for facility-based nutrition service provision. 2. 72 staff nurses at Stabilization Centers for inpatient Nutrition Care. Each SC will require a minimum of three member-staff for 24/7 operations: one existing staff will be utilized for this initiative, while other two members will be hired by the program. 2. In priority 12 Districts plus peri-urban areas of 9 mega districts (total of 21 districts), key interventions will be as following a. Supplementary Feeding Program i. Provision of Micro nutrient tablets to MAM PLWs ii. Provision of Micronutrient sachet to MAM children iii. Provision of Nutrition advocacy package (IYCF, immunization Wash, Fortification) b. Outpatient Therapeutic Program (OTP) iv. Provision of RUTF to SAM children without complication v. Provision of Nutrition advocacy package (IYCF, immunization Wash, Fortification) c. Stabilization Centers at DHQHs II. Provision of F75, F100 and advised medicines to SAM with medical complication 64 c) Addressing Micronutrient Malnutrition Micronutrient deficiencies are widespread in Punjab. Data for under-five years of age children reveals an alarming situation, with 40% children having iron deficiency anemia and 14% of preschool children having vitamin A deficiency. Micronutrient deficiency results from a complex interplay of factors, including poverty, limited access to a balanced diet, repeated infections and poor health and nutrition service delivery. Micronutrient (Iron, Folic Acid, Iodine, Zinc, Vitamin A and Vitamin D) deficiencies are multifaceted and are considered “silent hunger” which is hidden from everyone, from mothers’ to policy makers. Micronutrient deficiencies even at minor levels can leave an irreversible impact on growth and development of children. Hence in such context where the levels of acute and visible malnutrition are at critical levels of emergency, micronutrient deficiencies, specifically Iron deficiency Anemia and Iodine Deficiency Disorders are highly significant. Micronutrients are vital to healthy living, robust growth and intellect development. Fortifying flour and other staple food with folic acid and iron, can help in addressing micro nutrient deficiencies i-e reducing anaemia and birth defects; salt iodization reduces goiter and improves intellectual/ cognitive development; vitamin A supplementation plays an important role in reduction of child mortality and zinc supplementation reduces duration and severity of diarrhoea, one of the leading cause of deaths among children. The program seeks to address micro nutrition deficiencies, particularly among children of 6-59 months of age, PLW and adolescent girls, particularly from the lower income quintile and disadvantaged groups. Key activities Vitamin A supplementation campaigns Provision of iron folic supplements and counseling to pregnant and lactating women and adolescent girls Advocacy with policy makers and private industry for expansion of the wheat flour fortification program Advocacy with private salt processors for expansion of salt iodization program Creation of demand for iodized salt and wheat flour, through the BCC campaigns Setting up a system of sustainable supply of KIO3 (iodine fortificant) Treatment of diarrhea in children 6-24 months using zinc and ORS, ensuring continuous supply of Zinc and ORS and training of health workers Vitamin A supplementation Vitamin-A supplementation is being implemented with support from the Micronutrient Initiative (MI) and UNICEF administered through Polio NIDS for children 06 to 59 months. Currently Vitamin-A capsules are being administered through the Polio NIDs 65 Implementation status of provision of vitamin A through NIDs will be evaluated to assess coverage. The response would be designed accordingly. Expansion of Salt Iodization Program The province-wide expanded program will be made sustainable with effective behaviors. Legislation for compulsory salt iodization will be developed and promoted for ratification by provincial legislature with support of MI, WFP and UNICEF. It is anticipated that development partners will continue to support the production side with continuous monitoring of the salt processors and enabling regular access to potassium Iodate. Zinc Supplementation during Treatment of Diarrhea In many countries zinc supplementation during treatment of diarrhea has shown to have both curative (reduction in diarrhea) and preventive (fewer future episodes) effects. The commodity will be provided through HCP and LHWs for treatment of diarrhea. Behavior Change Behavior change is critical for practicing positive health related interventions. However, this requires assessments of behaviors and socio-cultural practices and translations of these into strategic health communications models. Along with communication efforts focused at ultimate beneficiaries, the project will entail advocacy interventions targeted at key stakeholders especially target population, policy makers and other players to garner relevant allocation of resources, oversight and support. Positive behaviors for adopting good health practices is a major resource for social, economic and personal development and an important dimension to quality of life. Political, economic, social, cultural, environmental, behavioral and biological factors can all favor health or be harmful to it. Health promotion action aims at making these conditions favorable through behavior change for health and nutrition. In our settings, income related poverty, illiteracy/ ignorance, socio-cultural practices, unemployment, dwelling style at rural, sub urban and urban slums contribute to household food insecurity/ inadequate food intake, inadequate care and unhealthy household environment. In this scenario, behavior change is significantly critical for practicing positive health and nutrition related interventions. However, this requires assessments of behaviors and translations of these into strategic health communications models. The objective of this component is: “To enhance levels of knowledge and increased awareness of nutrition intervention among men and women who have children less than 5 years of age and pregnant / lactating women” with special attention given to adolescent health The outcomes of the component are: Increased level of awareness among households about the nutrition interventions in the province with a focus on poor and disadvantaged. Increased knowledge about nutrition issues among households having children less than five years of age 66 Key activities Develop the tools and materials for communicating the key gender sensitive messages for behavior change and field test them before actual implementation The intervention will use multiplicity of channels, including face-to-face communication sessions, social mobilization and I.E.C. materials. The scope of communications component will focus on pregnant & lactating women and will address issues like breastfeeding, complementary feeding, use of multiple micronutrients, & use of iodized salt. In line with the use of latest technologies and methods for promoting healthy behaviors, the NPS will pilot the use of mobile phones for disseminating messages on nutrition promotion in one district, which should help in designing further strategies for promoting healthy nutrition behavior. 67 4. STRENGTHENING OF COMMUNITY-BASED OUTREACH SERVICES FOCUSING ON PHC, MNCH, RH/FP AND NUTRITION THROUGH IMPROVED PERFORMANCE OF LHWs AND CMWs Strengthening of PHC services including reproductive and family planning services is one of the most important components of the Program. Community based health workers already working at the community level for the above said purposes are LHWs and CMWs, that most of the deliveries in rural population (41% of the total) of Punjab takes place at homes through traditional birth attendants (TBAs) and unskilled birth attendants such as family members. Keeping in view illiteracy, poverty and access in terms of socio cultural and physical, it is necessary to provide skilled birth attendants at the doorstep of the community to conduct normal delivery with aseptic measures and at the same time identify and enhance uptake of facility-based deliveries through timely referral of cases to the most appropriate health facility. LHWs are working in catchment area population of 1200-1300 and providing PHC services. In Punjab almost 48,500 LHWs have been providing services regarding antenatal, postnatal and FP. They have also been providing service regarding IMNCI, immunization, control and prevention of malnutrition among women and children. CMWs are being trained and deployed to community-based need for SBA; they will work in close collaboration with LHWs of their area, providing trained prenatal and partum care at community level and refer high risk pregnancies and complicated cases to the most appropriate health facilities. Integration of service delivery at community-level will be developed by engendering linkages between CMWs and LHWs working within the communities. LHWs would refer pregnant mothers to SBAs for antenatal and normal delivery and both of them would work in a coordinated manner. However, strategies to improve coordination and service provision at community level, necessitates skills development, capacity building, effective monitoring and create strong referral linkages with health facilities. The following activities will be undertaken to integrate and improve community-based service provision. i. Capacity Building of community-based health workers a) b) c) ii. Capacity building of deployed CMWs on EMNC, CIMNCI, HTSP& PPFP counseling, IYCF and vaccination Capacity building of deployed LHWs on CIMNCI, IYCF, vaccination, HTSP and Postpartum Family Planning Counseling Refresher training of all CMWs and LHWs after periodic technical assessment Strengthening of Monitoring and Supervision of CMWs and LHWs d) e) f) Integration and consolidation of RH/MNCH data of CMWs and LHWs at the health facility level and dissemination to district DHIS and RH/MNCH office Monitoring visits to all LHWs and CMWs by LHS once a month Monitoring visit to all LHWs and CMWs by the District RH/MNCH focal person / district Monitoring officer at least twice biannually. 68 iii. Interventions for Hard to Reach Areas and urban slums g) h) Identification of hard to reach areas (in all districts) and urban slums (in bigger districts) in all districts after district mapping Review and revision of existing training manuals of CMW for LHW cum CMW training. 69 5. STRENGTHENING LINKAGES BETWEEN COMMUNITY OUTREACH HEALTH WORKERS WITH HEALTH FACILITIES Linkages of community based workers (LHWs& CMWs) with health facilities have not been established to the extent it was desired due to various reasons which may be poor quality of health services, limited scope, non availability of health care providers, poor physical access and improper provider’s behavior and direct and indirect cost associated with use of health care. At the same time socio cultural barriers are equally important in utilization of health care. One of the important reasons is the absence of well established referral protocols at the health facilities and referred patients/clients are not treated on priority basis. Therefore it is necessary to improve the access and availability of well trained and competent human resources at the health facilities. There is a dire need to develop referral protocols in terms of establishment of referral desk at THQ and DHQ level. There is also need to provide a gender friendly environment at the health facilities in terms of separate waiting area and wash room for the female patients. The following activities will be undertaken to improve linkages of community-based workers with health facilities. a) b) Development and implementation of referral protocols for referral of high risk cases to Basic and Comprehensive EMONC facilities Implementation of referral and follow up system for SAM Children with medical complication to established SC centers. 70 6. ESTABLISHING E-MONITORING AND E-REPORTING SYSTEM AND A WEB-BASED PROGRAM MIS WITH LINKAGES TO DHIS A strong monitoring and evaluation system is necessary to ensure proper functioning of the program in order to achieve the desired outputs and outcomes. M&E system of the program will be linked regular national Program monitoring system. Strong e-reporting and monitoring system will be prepared and launched at provincial level for example the monitoring reports submitted by all levels of supervisors and monitors (LHS, supervisors, district managers, provincial monitors, and provincial monitors) will be entered directly into the software through text messages and mobile phone based web applications. Soft ware engineer will be appointed on Provincial implementation unit level, s/he will be responsible for the up gradation of this reporting and monitoring software. The monitoring reports of these monitors will be submitted using web based mobile phone applications, and shall be immediately accessible to the managers. A robust program management information system is important to record the program implementation activities at ground level, preparation of program performance reports and planning of subsequent activities as well as policy designs. The program MIS will be web-based and deployed on a central server at the provincial office. District offices will be able to access and add information to the MIS by logging in at the program website. District monthly reports will be submitted online through web based data entry forms. A dashboard will be developed on the program website for provision of live streaming data based on the reports received. The software will generate analyzed reports for each level of management staff. These reports will be available to the managers on logging in to their personal accounts at the website. Key Activities 1. 2. 3. 4. 5. 6. Development of key performance indicators will be for all program management and support staff at the PMU and DMU. These KPIs shall be used for annual performance evaluation reports and renewal of contractual staff. Recommendations for transfer of poor performing management staff working on deputation will be made to the competent authority based on the performance evaluation reports. Development of e-monitoring module and integration with the program MIS Provision of tracking SIMs to all community staff Provision of handsets having monitoring software and GPS technology to the district and provincial monitoring staff to ensure their presence in the field and timely submission of monitoring reports Purchase of required hardware and equipment for implementation of e-monitoring Hiring of relevant staff 71 Field Monitoring by Health Officer Under this program, as a leader of the health team, each health officer will conduct a monitoring and supervisory visit in the field every week to provide support to field staff. S/he will validate progress reports of LHWs, LHS, CMW, vaccinator, health and nutrition supervisor and male mobilizers and provide guidance and support to field staff in their activities. Monthly Meeting of BHU Health Team Each member of BHU health team will meet once every month at the BHU. The primary purpose is to prepare monthly progress reports, discuss progress made and issues faced during the last month and receive refresher training/Continuing Medical Education (as and when required), on the basis of findings of the field monitoring. 72 Conceptual Framework for E-Management 73 7. STRENGTHENING LINKAGES BETWEEN COMMUNITY AND THE HEALTH FACILITIES Linkages of community with the health facility would be created by constituting community support group at the health facility through Lady Health Worker and School Health and Nutrition Supervisors (SHNs). The objective is to ensure effective community participation and public accountability. This program views the communities not as merely the passive recipients of the benefits but as the key contributors in the overall process of health promotion and health improvements. Their participation initially will lead to communities’ capacity building through organizing and training them, and involving them in the implementation process. Thereafter, the communities start performing as active partners in planning, governing and owning of the health interventions alongside the professional and technical staff. This combination will certainly multiply the outcome of the interventions manifolds. The key to the success of this program is building communities’ trust on their health care delivery system. This can only be achieved through ensuring their active participation and providing space for them to play their supportive role in the process. There are two important explanations for seeking participation from the community: 1. The communities, which are otherwise alienated from the health service delivery system, develop ownership; and 2. Community members, being the sole benefactors of the health care delivery system, start contributing towards its further improvement. This process of community participation will lead to the establishment of “Community Governance Structure” starting with the formation of “Community Support Group (CSG)” within the catchment area of each of the program BHUs and leading to the district level. This is, in fact, an evolution of bringing the community members, who otherwise live and generally act in isolation, at a common platform for contributing and performing together in a cohesive manner. This cohesiveness strengthens the communities’ efforts leading to outcomes which are otherwise not possible through individual efforts. These CSGs will identify and discuss issues, find solutions and implement them in order to support the health interventions being carried out for their benefit. Moreover, they will provide support to field level health workers like LHWs, LHS, vaccinators and CDC supervisors. Formation of Community Support Group The process of organizing communities into CSG starts from the village level and involves all the population of the village. This essentially consists of the following steps: 1. Determining the number of communities (villages) in the catchment area of a BHU; 2. Establishing contact with each community through broad based community meeting; 3. Introduction of health program components to each community; 74 4. Facilitating each community to identify its 1-2 representatives 14 through a process that best suits them; 5. Bringing all these community representatives together at a platform to discuss and formalize this platform in the form of Community Support Group; 6. Strengthening these community platforms through regular technical training e.g., in general management, problem solving techniques, financial management, and small scale project planning, etc.; 7. Facilitating the members of “Community Support Group” to share the discussions and decisions of the forum with their fellow community members (whom they are representing) in order to continuously seek their inputs and advice; 8. Formalizing these community structures as “Community Support Group (CSG)” to take active part in the process along with the technical staff; 9. Holding regular meetings of the CSG at least once every month. Membership of CSG In addition to community representatives, health officer of the BHU and SHNS (as secretary of CSG) will be permanent members of the CSG. The CSG may include more members with the consent of its members. A community representative is the community member who is well trusted and respected by that community in all walks of life. 14 75 STRENGTHENING DISTRICT HEALTH SYSTEM This part of the program focuses at enhancing capacity of district health system to deliver essential package of healthcare (EPHC) at primary and secondary levels. The district health system undergoes process of strengthening which starts at the household level and reaches to the highest level of health care service delivery within the district. The following strategies are will be used to implement proposed interventions. Ensuring Essential Package of Health Services Ensuring EPNH (Essential newborn package) Services in the Field Under this program, the essential newborn package prepared by WHO and UNICEF and adopted by Ministry of Health, Government of Pakistan will be implemented at the community level through CMWs and LHWs. This program will develop training manual for community essential newborn package and will include it in LHWs and CMWs curriculum. Refresher training will be given and all the LHWs and CMWs will be trained in neonatal care which include immediate and critical life support to a new born by mouth-to-mouth resuscitation, prevention from hypothermia by keeping baby warm through Kangaroo mother care and delayed bathing, early initiation of breast feeding and ensuring cord care with Chlorhexidine. The LHWs and CMWs will educate pregnant women and their family on ENC package during antenatal care. The LHW will also assist the birth attendant in resuscitation of newborn at the time of delivery. She will conduct follow up visits for postnatal and neonatal care on day,1 3, 7, 14 and 28th days of birth. The LHWs and CMWs will be trained in identification of any sign of illness and to provide immediate pre-referral care to the newborn and refer to health facility. Ensuring Child Spacing Services Child spacing is an essential part of LHWs and CMWs training. The LHWs and CMWs will educate their respective communities on importance of Healthy Time Spacing (HTSP) . They will offer child spacing health education with information on their side effects, and help the willing women in selecting a method of their choice and provide them with that method or refer them to BHU to obtain that method. The LHWs and CMWs will counsel the women facing any side effects of child spacing methods and refer them to BHU, for appropriate treatment and guidance. Ensuring EMNC Services Care provision for common illnesses among neonates and infants especially infections, complications of preterm birth and of birth asphyxia, and prevention from hypothermia save significant number of lives. This program will ensure these services at all health facilities 76 through training of respective staff members as well as provision of specialized equipment at referral facilities. The components of ENC package include immediate life support for newborn by mouth to mouth breathing, prevention from hypothermia by keep warm through Kangaroo mother care and delayed bathing, early initiation of breast milk, and cord care with 4% chlorhexidine solution. BHUs & RHCs The health care provider at all the 2,456 basic health units and 289 rural health centers will be trained in ENC package during the currency of the program duration. The preference will be given to female health care providers who deal with the newborn in the labor room. The twenty districts where CHARM and CMAM interventions will be replicated shall be given priority The health care providers at BHUs and RHCs will identify the serious neonatal conditions and will provide pre-referral care including first dose of intravenous antibiotic where required. All the required items including Ambo bag, oxygen and antibiotics will be made available at all BHUs and RHCs. The neonatal cases referred from the field will be entertained at BHUs and RHCs for management and further referrals to THQ and DHQ hospitals where required. Newborn Care Protocols The protocols for newborn resuscitation and immediate care have already been developed in Pakistan by Women’s Health Project. These protocols will be provided to all the labor rooms at BHUs, RHCs, THQ and DHQ hospitals in public sector and in around 1,500 maternity homes in the private sector. THQ & DHQ Hospitals At all THQ and DHQ hospitals, newborn care units would be established to become part of the comprehensive and basic emergency obstetric care services. All the facility staff handling deliveries would be trained in essential newborn care. However, for emergency newborn care specialized units would be established with adequate staff and equipment. Staff would be given specialized training for the purpose and will be permanently deployed in the unit rather than on rotation basis (especially the nursing staff) .All health facilities providing comprehensive EmONC services will have functional newborn units. Each newborn unit will require minimally the presence of a pediatrician, one medical officer / woman medical officer specifically for the unit in addition to at least two staff nurses to run the unit. This staff strength is included in the minimum staff requirement for 24/7 EmONC services which is given in the EmONC section. 77 Strengthen Program Management In order to strengthen overall program management the program will: 1. Develop standard operational procedures (SOPs) for program operations, personnel management and logistics management; 2. Set minimum service delivery standards (MSDS) for each of the program interventions with specified levels and dimensions; 3. Develop modalities for pre-service and induction training for various staff categories working in the program; 4. Develop and implement monitoring and supportive supervision system consisting of monitoring checklists, schedules, data base and mechanism for feedback and follow up on suggested corrective actions. Field Monitoring Officers/M&E Officers The Provincial Office will conduct monitoring and supervision of program field-activities through a cadre of Field Monitoring Officers. This cadre will be developed by re-designating existing FPOs (of LHW Program) and social organizers (of MNCH Program) for supervision. The M& E Officer is a BPS 17 position. Provincial PMU officers will also conduct regular supervision activities in the districts and support the FPOs. 78 INNOVATIONS The aforementioned interventions will continue throughout the period of PC-1 from 2013-2016. The program will also begin testing new models and innovations. The Program aims to take advantage of important new evidence on the impact of certain maternal and child health interventions in order to fine-tune the package of services provided by the LHWs. Though the evidence on some of these interventions appears to be quite promising, some would need to be pilot-tested prior to their introduction in the program. Some programmatic interventions to be pilot-tested would be chosen following a screening process by the “Technical Committee on Interventions” with membership from within Program and technical experts on maternal health, child health and public health with experience of using scientific research methods and tools. Funding for the pilot of these innovations will be sought from donor organizations and partners like UNICEF, UNFPA, etc. Suggested avenues for exploration include 1. Health systems research, including 2. Pilot test impact of field monitoring through use of mobile phones Pay for performance initiatives for community-based and facility-based healthcare staff Pilot test establishment and assess impact of EPI Centers at LHW Health House Nutritional interventions research, including Evaluation of efficacy of Wheat-Soy Blend (WSB) in treatment of PLWs and impact of nutrition status of index case and birth weight of newborn in Districts DG Khan and Rajanpur Development and field-based evaluation of local low-cost nutritional alternatives to Ready to Use Therapeutic Food (RUTF) Feasibility of follow-up and treatment of SAM children by LHWs 79 MANAGEMENT STRUCTURE Administrative Arrangements The administrative arrangements for program implementation consist of establishment of: 1. 2. Provincial and district steering committees Provincial and district management units Provincial Steering Committee (PSC) Provincial steering committee shall comprise of: • • • • • • • Chairman Planning & Development Department /Member Social Sector Secretary Health Director General Health Program Director PHSRP Program Director DG Population Welfare Department Secretary Finance Department Chairman Member Member Member Secretary Member Member District Steering Committee (DSC) District steering committee shall comprise of: • • • • • District Coordination Officer Executive District Officer (Health) District Coordinator District Officer Health EDO F&P Chairman Member Secretary Member Member Provincial Level Management Committee A Provincial level Management Committee will be notified for the purpose of selection of Districts and health facilities for implementation of the proposed program activities. Headed by Secretary Health, the Committee will comprise of the memberships: Program Manager Representative from DGHS Office Representative from PHSRP/PSU Office This committee will be responsible for District-based mapping of health facilities and determining selection of sites for program implementation in a phased manner for Nutrition, Primary Health and Reproductive Health interventions. 80 Department of PHC, FP, RH & nutrition Policy for the program, Service specification, Funding, Health Program Monitoring and Evaluation PHC Policy Advice, National Reporting, Internal Supervision and Monitoring, Evaluation, Training, Program, Procurement/Distribution, Operational Planning and budgeting, Financial Accounting, LHW-MIS System PMU Internal Supervision and Monitoring, Program Reporting, District LHW Allocation, Operational Plan Implementation, Accounting and Budgeting, Organization of Training, Distribution, LHW-MIS Data Collation and analysis. LHW, CMW, LHS-District Supervision, LHW & LHS Hiring /Firing, Training, Operational DMU Plan Implementation, Distribution, Vehicle maintenance, Accounting, Program Reporting, MIS Data Collation, analysis and use of information in management Recommendation for hiring of LHWs & LHSs by the Medical Officer/Woman Medical Officer, Training of LHWs, Collation of MIS, Organizing Kit replenishment, FLCF (all) Providing meeting point for LHWs and LHS, and collaboration with CMWs and PWD staff. Selected RHCs for Provision of comprehensive EmONC services and serve as a referral facility for Comprehensive obstetric cases EmONC Services All RHCs and Provision of basic EmONC services round the clock, provision of outdoor obstetric Selected BHUs for care, routine EPI, family planning services and nutrition services (CMAM/OTP). 24/7 EmONC Basic Additional HR, equipment and supplies will be ensured to enhance the capacity & of these facilities for provision of services beyond the existing ToRs. Nutrition Services LHW PHC & FP service provision to community, community organization CMW MNCH & FP service provision to community 81 THE PMU Role The program management unit shall be based at the provincial head quarter and will be headed by the Program Director/ ADGHS. The PMU shall be responsible to provide leadership role in addition to this program to MNCH & LHWs Program; 1. 2. 3. 4. 5. 6. Play steward ship role in formulation of program policy guidelines in consultation with all stakeholders and dissemination of the same to all district managers. Constitute and notify the technical advisory groups ( TAG) on different themetic areas for formulation of technical guidlines Development of training and capacity building strategies, training modules, training of master trainers Monitoring and evaluation of program activities, internal evaluations, coordination for third party evaluations Conduct performance audit and internal financial audit of the districts Hearing of appeals against the district management unit 82 JOB Description Designation &Pay scale Eligibility Criteria ToRs / Responsibilities Deputy Program Manager A medical doctor with post graduate Deputy Program Manager Nutrition, reporting to the Provincial Coordinator, shall be responsible for affairs related to Project activities, finances, Nutrition qualification in public health procurement and logistics and assignments given by the Provincial Coordinator BPS 19/18 by transfer/ At least 15 years of experience at mid time to time. Deputation/open competition and senior level positions including 5 years of project management experience He will be employed through transfer/deputation from Health Department. In for implementation of field based case Health Department not depute any officer within six months after the projects requisition by this office and repeated requests the officer may be appointed on contract basis through open competition. Nutrition Officer BPS 17- S/he is having at least 1st Division Degree in MSC Nutrition alongwith 02 years experience in Public Health Sector or implementing nutrition based projects. Nutrition Officer will be reporting to the Deputy Program Director, is responsible for overall management, planning ,provision of technical support and successful nutrition trainings. Or assignments given by the Provincial Coordinator/Deputy Program manager nutrition time to time. The remuneration for this position will be equivalent to grade 17 officer as admissible under the Government rules in case of an existing Government employee or Rs. 100,000 per month in case of non- Government candidates. Research Officer BPS 17 Or i. market based @ Rs. 80,000/ii. 1st class Master’s Degree in Bio Research Officer will be reporting to the Deputy Program Director is responsible for overall management, planning,provision of technical support and successful Statistic. nutrition trainings. Or assignments given by the Provincial Coordinator/Deputy 02 years experience of Program manager nutrition time to time. monitoring demonstrated experience and competence in The remuneration for this position will be equivalent to grade 17 officer as monitoring and evaluation, admissible under the Government rules in case of an existing Government Nutrition project management employee or Rs. 100,000 per month in case of non- Government candidates. and training. 83 iii. Knowledge of computerized database & statistical analysis software. iv. Proven management experience for minimum of three years v. Master’s level university or vocational training in Social Sciences, Management or Public Health. Data Entry BPS-12 Or market S/he at least D.COM having 02 year Data Entry Operator, reporting to the research officer for reporting nutrition experience in Data Entry in Public Health project data or any assignment given to him / her by Nutrition / Research Officer based @ Rs. 35,000/Sector or Implementing field services projects. The remuneration for this position will be equivalent to grade 12 officer with a project allowance as admissible under the Government rules in case of an existing Government employee or Rs. 35,000/- per month in case of nonGovernment candidates. 84 Facility & Field Staff Designation & Pay scale WMO LHV 1.1 Eligibility Requirement Roles & Responsibilities MBBS Preference will be given to those with post graduate diploma/fellowships in obstetrics & gynecology or pediatrics LHV course At least six months of experience in public sector Budget: Budget of the Program will be prepared by PMU, in accordance with the provisions of the PC-1. Finance Officer of PMU will prepare NISs (New Items Statements) i.e. budget statements for coming financial year(s) (mentioned in Table-A below) according to accounting circle and he will submit the NISs to Department of Health for signature of Section Officer (Development) and endorsement of Deputy Financial Advisor (Health). Sr. No. 1 1.2 NISs of each office of the Program Accounting Circles PMU-Punjab, Lahore (includes budgets of DMUs). AG Punjab, Lahore & District Accounts Offices in all District of Punjab. Releases and Fund Flow Mechanism at PMU Punjab. The PMU will submit the budget demand as per approved cash plan or according to instructions of Ministry of Finance regarding release/ utilization of funds to Health Department Govt. of the Punjab for release of funds from Planning Division, Govt. of Pakistan under PSDP Sr. No. 31 as per CCI decision dated 28-04-2011. Planning Division Islamabad will release the budget on quarterly basis to Govt. of Punjab through Planning & Development Department Govt. of Punjab Lahore to Health Department Govt. of Punjab for further release into Assignment A/c maintained in NBP Main branch Lahore and in A/c-I to all districts in Punjab on the request of Provincial PIU to SDAs of development funds maintained by District Coordination Officers and Executive Districts Officers (F & P) through District Accounts Offices concerned. Health Department, Govt. of Punjab will forward the budget request of PMU to Finance Department, Govt. of Punjab for release of budget. 85 1.3 Releases and Fund Flow Mechanism at District Level. On request of PMU, the Finance Department, Govt. of Punjab through Health Department will release the budget in systems against the Cost Centers of development funds to all districts in Punjab and as well as ceiled copy to District Accounts Offices concerned and intimation copies to all relevant departments. The District Accounts Offices concerned on receipt of ceiled budget copy from Finance Department, Govt. of Punjab Lahore will release budget into SDA A/c maintained in the O/o EDO (F & P) with the signatures of DCO & EDO (F & P). The District Coordinator National Program of concerned district will sign the all object head claims and will forward to EDO (F & P) through EDO (Health) for payment. The EDO (F & P) will forward the claims to DAO concerned for pre-audit and after pre-audit, the EDO (F&P) office will issue the SDA cheque in the name of vendors after ensuring that all payments are being made through bank without any encashment of cheque. The SDAs of DMUs will contain funds on account of Telephone & Trunk Calls, Courier & Pilot Services, POL, Stationary, Others Miscellaneous & Repair of Vehicles. All payments from the SDAs will be made by PMU with the approval of competent authority. District Coordinator National Program and his staff will carry out reconciliation of the receipts and expenditure pertaining to the SDAs on monthly basis. It is responsibility of the District Coordinator/Account Supervisor that outstanding cheques are cleared for payments and no outstanding balance will remain in the SDAs. 1.4 Assignment Accounts of PMU PMU Assignment Account has the approval of Finance Department and Finance Department is placing funds in the PMUs Assignment A/cs through the funds ceiling sanction letter addressed to the AG Punjab. The AG Punjab then issue sealed authority letter to Treasury Officer Lahore for its crediting through challan form/receipt voucher into Assignment A/c No. 103 maintained at NBP Main branch, Lahore for admitting expenditure up to the amount mentioned in the sanction letters. The AAs of PMUs will contain funds on account of employee related expenses; purchase of assets and for all PMU operational costs/expenses. Payments of stipends of LHWs, LHSs, and all Programs employees including employees working at DMUs levels are made from Provincial AAs. Two authorized signatories will operate the AA. All payments from the AA will be made by PMU with the approval of competent authority. The AA cheques will be issued under the signature of two authorized signatories. The schedule of the cheques will be sent to the concerned NBPs. Finance and Accounts (F&A) Section of PMU will carry out reconciliation of the receipts and expenditure pertaining to the AA on monthly basis. It is responsibility of the F&A Section of PMUs that outstanding cheques are cleared for payments and no outstanding balance will remain in the AA. 86 1.5 Reconciliation with DAO/TO and Banks Reconciliation with AG Punjab/Treasury Office of Assignment Account and SDAs A/cs with District Accounts Offices will be made on monthly basis by the Finance Officer of PMU and the District Coordinators and Accounts Supervisors respectively. 1.6 Finance and Accounts Staff Finance Officer, Audit Officers, Cashiers will be hired on deputation basis from AGP/CGA however, existing working officers/staff will continue to work if they have been appointed on contract basis with the approval of competent authority. In case AGP/CGA offices do not fill in the position within four (4) months of the submission of requisitions and repeated requests, the position will be filled in on contract basis in consultation/approval of the Department of Health. Accountants and Senior Auditor posts will be filled on contract basis however during the recruitment on contract basis, PMU will give priority to existing staff. 1.7 Internal Audit: Internal audit of Program units i.e. PMUs and DMUs will be carried out by the DGHS on regular basis. Internal audit of PMU will be carried out annually whereas the PMU will also conduct audit of the districts in such a way that each district should be audited once in 02 years. However, PMU should also conduct internal audit of DMUs. 1.8 External Audit: Audit Team of the Auditor General of Pakistan will conduct audit of accounts of the Program at PMU and DMUs level. Audit Officer of PMU will coordinate external audit task. 87 Schedule of Activities for Nutrition Program Punjab Annexure Activity Year 1 1st 2nd 3rd Year 2 4th 1st 2nd 3rd Year 3 4th 1st 2nd 3rd 4th Selection of Centre for Nutrition Activities Component 1: Addressing General Malnutrition among Children, Pregnant and Lactating Women Sub Component 1.1 Infant and Young Child Feeding (IYCF) 1.1.1 Provincial level dissemination of IYCF Strategy 1.1.2 Training of district master trainers on IYCF) in 12 districts (02 Master trainers per districts) 1.1.3 Training of Health care facility staff on IYCF component at District level 1.1.4 Training of LHWs, CMWs on IYCF component at facility level 1.1.5 Training of LHS on IYCF and Nutrition supportive monitoring 1.1.5.1 Development of MIS monitoring and reporting tools 1.1.5.2 Preparation of Training manual for reporting and monitoring tools 1.1.5.3 Training of LHS on monitoring and reporting tools 1.1.6 Implementation of IYCF activities Sub Component 1.2 Community Management of Acute Malnutrition for children and pregnant and lactating women 1.2.1 Training of district master trainers 88 on Nutrition 1.2.2 Training of health care facility staff (BHU, RHC) on nutrition 1.2.3 Training of LHWs on Screening referral 1.2.4 Implementation of CMAM activities 1.2.11 Strengthening/operationalization of Health facilities as OTPs (BHUs and RHCs) 1.2.11.1 Provision of OTP supplies and equipment 1.2.11.2 Procurement and distribution of Ready to use therapeutic food (RUTF) 1.2.12 Strengthening/operationalization of stabilization centers at the DHQ level 1.2.12.1 Recruitment and training of SC staff 1.2.12.2 Provision of SC supplies and equipment 1.2.12.3 distribution of F100 and F75 1.2.12.4 distribution of Ready to use Therapeutic food Activity Year 1 1st 2nd 3rd Year 2 4th 1st 2nd 3rd Year 3 4th 1st 2nd 3rd 4th Sub-Component 1.3 Management of Maternal Malnutrition 1.3.1 Procurement and Distribution of Iron Folic Acid tablets 1.3.2 Provision of Iron Folic Acid tablets to Pregnant women and Adoscolent girls 89 Component 2: Addressing Micronutrient Malnutrition: Sub Component 2.2 Universal salt iodization program: 2.1.2 Developing and designing the legislative/Enforcement mechanisms for solt iodization fortification of all food items to be fortified Consultative Meetings with Private Sector for arrangements for procurement and distribution of KOI at commercial rates Refresher training of health managers and District Focal Persons on management, monitoring and quality control of iodized salt. Refresher training of salt processors on salt iodization techniques & internal quality control. Bi Annual meeting of provincial steering committee on IDD/USI and district IDD Control Committees Sub Component ___Vitamin A Supplementation Program 2.1.1 Provincial level seminars on VAS with the line departments and development partners for advocacy and sensitization on VAS Refresher training of health managers and district EPI focal persons on management of Vitamin A supplementation campaign and its monitoring. Awareness raising sessions of Medical Officers, School Health and nutrition supervisors, vaccinators and Lady health supervisors. 90 Activity Year 1 1st Q 2nd 3rd Year 2 4th 1st 2nd 3rd Year 3 4th 1st 2nd 3rd 4th Sub Component 2.4 Zinc supplementation treatment of diarrhea during 2.4.1 Procurement and distribution of Zinc sulphate 2.4.2 Training of Health Facility Staff 2.4.3 Training of LHWs/CMWs 2.4.4 Treatment of Diarrhea with Zinc Sulphate and ORS Subcomponent 2.5 Use of Multimicronutrient Powder through LHWs program 2.5.1 Procurement and distribution of Multi Micronutrient Powder Sachet 2.5.2 Training of Lady Health Workers, LHSand CMWs 2.5.3 Provision of Multimieronutrient Sachet to children 06-23 months of age Component 3 Communication For Development 3.1.1 IEC matrial for distribution to Health Facility and Community based staff 3.1.4 Material Field implemented tested and 3.1.2 Distribution of IEC matrial to Districts Component 4. Strengthening Arrangements Institutional 4.1.1 Placing of appropriate staff at 91 provincial and district level 4.1.3 Meeting of the provincial Integrated Nutrition committee 4.1.1 Meetings of Provincial coordination committee 4.1.2 Meetings of District Coordination Committee 4.1.3 Meetings of Thematic Working Group 4.1.4 Collaboration meeting with partners Strengthening Research, Monitoring and Evaluation Systems 5.1.1 Annual Assessments 5.1.2 Integration of different infromation systems 92 93 DGHS Program Director Additional PD I Finance Officers I and II Accountan ts Logistics Officer Procureme nt Officer Logistic Assistant/ Store Keeper Internal Auditor Deputy PD Human Resource Training Coordinator Deputy PD Training and Capacity Building Health Education Officer Additional PD II Deputy PD MIS/M&E R&D Officer Researcher Data Analysts Software Developer Computer Programmer Field Monitoring Officers Additional Deputy PDPD IIIDeputy PD Facility Community Based Based Interventio Interventio ns ns Nutrition MIS Coordinator Officer Data Analysts Data Entry Operators 94 EDO (H) DDOH (PHC & RH) M&E (Adm) M&E (Tech) Accounts Assistant Logistics Assistant Data Entry Operator 95 Annex: Organogram 96 Annex: Facility Based Services 97 98 ANNEXURES 99 STAFF STRENGTH No of FLCF S.No Cadre BPS/Fixed Salary Strength No of FLCF FINANCIAL YEAR 2013-14 BPS/Fixed Salary Strength No of FLCF FINANCIAL YEAR 2014-15 BPS/Fixed Salary Strength FINANCIAL YEAR 2015-16 Field Staff 1 Nursing Staff (for DHQ Nutrition) 34 DHQ +2 Teaching hospital 2 WMO 292 RHCs 3 Computer Operator PMU 4 LHVs (CHARM) 300 BHUs 5 Aya (CHARM) 300 BHUs 6 Ambulance drivers (CHARM) 7 Gaurds (CHARM) Fixed Salary 72 34 DHQ +2 Teaching hospital 72 34 DHQ +2 Teaching hospital 72 292 292 RHCs 292 292 RHCs 292 2 PMU Fixed Salary 2 PMU Fixed Salary 2 600 500 BHUs 1000 700 BHUs 1400 600 500 BHUs 1000 700 BHUs 1400 200 300 BHUs 300 Total Field Staff (2013-14) 2066 333 500 BHUS 500 Total Field Staff (2014-15) 3199 466 700 BHUs 1400 Total Field Staff (2015-16) 5032 PMU STAFF 1 Program Manager Nutrition 18/19 1 2 Nutrition Officer 17 1 3 Software Engineer 17 1 4 Statestical Officer 17 1 Total PMU Staff (2013-14) 4 Total PMU + Field Staff (2013-14) 2070 Program Manager Nutrition Nutrition Officer Software Engineer Statestical Officer 18/19 1 Program Manager Nutrition 17 1 17 17 Total PMU Staff (2014-15) Total PMU + Field Staff (201415) 18/19 1 Nutrition Officer 17 1 1 Software Engineer 17 1 1 Statestical Officer 17 1 4 Total PMU Staff (2015-16) 4 3203 Total PMU + Field Staff (2015-16) 5036 100 Targeted Married Women & Children Per Beneficiary Cost Total Population 16 % Married Women of Total Population 14 % Children of Total Population Total Population of Married Women & Children Average Cost 2013-16 Average Annual Cost of Married Women & Children 94,000,000 15,040,000 13,160,000 28,200,000 3,271,390,359 116 Total Population Targeted Population of Married Women & Children Average Annual Cost of Married Women & Children 94,000,000 28,200,000 116 100,000,000 90,000,000 80,000,000 70,000,000 60,000,000 50,000,000 40,000,000 30,000,000 20,000,000 10,000,000 0 Series1 101 Total Required Cost for Procurement of Contraceptives Total Population Urban Population (30% of Total Population) Rural Population (70% of Total Population) Eligible Couples in Urban Area (16% of Urban Population) 94,157,907 28,247,372 65,910,535 4,519,580 Budget Demand for Procurement of Contraceptives in PC-I by the Vertical Program S.No 1 2 3 Name of Program Lady Health Worker Program National MNCH Program Nutrition + CHARM Total FY Budget Demanded Eligible Couples in Rural Area (16% of Rural Population) Targeted Eligible Couples in Urban/Users of Contraceptives (25% of Eligible Couples in Urban Area) Targeted Eligible Couples in Rural/Users of Contraceptives (50% of Eligible Couples in Rural Area) Contraceptive Cost per Couple per month in Urban (Targeted Eligible Couple s in Urban x 30x 12) Contraceptive Cost per Couple per month in Rural (Targeted Eligible Couple s in Rural x 30x 12) Total Cost of Contraceptives for per couple per month 10,545,686 1,129,895 5,272,843 406,762,158 1,898,223,405 2,304,985,563 2.5E+09 2E+09 1.5E+09 2011-17 575364924 2012-16 800,000,000 2013-16 850000000 Name of Program FY 1E+09 Budget Demanded 500000000 0 1 2 3 Total 2225364924 102 Year wise Cost Sheets for UNICEF & WFP Shares S.No FY UNICEF Share (Cost of Mobendazoal+Cost per SAM Child in 07 Districts) 1 2013-14 260,155,109 43,336,800 303,491,909 2 3 2014-15 2015-16 - 43,336,800 43,336,800 43,336,800 43,336,800 260,155,109 130,010,400 390,165,509 Total WFP Share (Cost Per PLW for Rajanpur & D.G.Khan) Total UNICEF & WFP Share 400,000,000 200,000,000 - 1 2 3 Total 103 District wise phasing of Implementation of MCH and Nutrition Interventions 2013-14 Sr. No Name Of District 1 Narowal 2 Layyah 3 Mianwali 4 Multan 5 Hafizabad 6 Rahimyar Khan 7 Pakpattan 8 D. G. Khan 9 Muzaffargarh 10 Bhakkar 11 Rajanpur 12 Bhawal Nagar 13 Jhang 14 Sargodha 15 Bahwalpur 16 Khanewal 17 Rawalpindi 18 Sahiwal 19 Faisalabad 20 Sialkot 21 Lahore 22 Attock 23 Chiniot 24 Gujrat 25 Khushab 26 Jhang 27 Jhelum 28 Kasur 29 Lodhran 30 Vehari 31 M.B. Din 32 Chakwal 33 Nankana Sahib 34 Okara 35 Sheikhupura 36 T.T. Singh Nutrition Interventions 2014-15 24/7 Nutrition Interventions 2015-16 24/7 Nutrition Interventions 24/7 104 PAY OF OFFICERS Basic Pay Pay of Contract Staff ALLOWANCES REGULAR ALLOWANCES House Rent Allowance Conveyance Allowance Medical Allowance Deputation Allowance Special Travelling Allowance (FTA) Non Practicing Allowance Special Additional Allowance (50% 2010) 105 Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program Yearwise Phasing for the Financial Year 2013-16 A01 A01106 A012 Object Heads Financial Year 2013-14 Financial Year 2014-15 Financial Year 2015-16 Total 2013-16 Average 2013-16 EMPLOYEE RELATED EXPENSES 588,210,384 789,970,384 1,090,684,384 2,468,865,152 822,955,051 PAY 1,719,600 1,719,600 1,719,600 5,158,800 1,719,600 PAY OF OFFICERS 1,719,600 1,719,600 1,719,600 5,158,800 1,719,600 Pay of Contract Staff 1,119,600 1,119,600 1,119,600 3,358,800 1,119,600 ALLOWANCES 586,490,784 788,250,784 1,088,964,784 2,463,706,352 821,235,451 REGULAR ALLOWANCES 53,930,784 53,930,784 71,450,784 179,312,352 59,770,784 A01202 House Rent Allowance 229,296 229,296 229,296 687,888 229,296 A01203 Conveyance Allowance 240,000 240,000 240,000 720,000 240,000 A01217 Medical Allowance 146,544 146,544 146,544 439,632 146,544 A01236 Deputation Allowance 72,000 72,000 72,000 216,000 72,000 A01243 Special Travelling Allowance (FTA) 52,560,000 52,560,000 70,080,000 175,200,000 58,400,000 A01252 Non Practicing Allowance 48,000 48,000 48,000 144,000 48,000 A01964 Special Additional Allowance (50% 2010) 488,400 488,400 488,400 1,465,200 488,400 Adhoc Relief Allowance (15% 2011) 146,544 146,544 146,544 439,632 146,544 532,560,000 734,320,000 1,017,514,000 2,284,394,000 761,464,667 A0 1970 OTHER ALLOWANCES A01271 Over Time Allownace A01273 Honorarium/Incentive for performance/ 10,000 10,000 10,000 30,000 10,000 44,160,000 44,160,000 44,160,000 132,480,000 44,160,000 A01274 Medical Charges 50,000 6,804,000 6,804,000 13,658,000 4,552,667 A01277 Contingent Paid staff 25,500,000 25,500,000 18,300,000 69,300,000 23,100,000 A01299 Other (Stipend of LHVs, Ayas, Ambulance Drivers & Guards) 462,840,000 657,846,000 948,240,000 2,068,926,000 689,642,000 A03 OPERATING EXPENSES 553,534,213 602,678,846 696,046,618 1,852,259,677 617,419,892 A032 COMMUNICATION 1,160,000 1,160,000 1,160,000 3,480,000 1,160,000 A03201 Postage and Telegraph 20,000 20,000 20,000 60,000 20,000 A03202 Telephone and Trunk Calls Charges 100,000 100,000 100,000 300,000 100,000 A03203 Telex. Teleprinter and Fax 40,000 40,000 40,000 120,000 40,000 A03204 Electronic communication ( E - Governance + Internet Charges) 800,000 800,000 800,000 2,400,000 800,000 A03205 Courior and Pilot Services 200,000 200,000 200,000 600,000 200,000 UTILITIES 600,000 600,000 600,000 1,800,000 600,000 Electricity Charges 600,000 600,000 600,000 1,800,000 600,000 OCCUPANCY COSTS 500,000 500,000 500,000 1,500,000 500,000 Rates & Taxes( Vehicles Tax & Toll Tax) 500,000 500,000 500,000 1,500,000 500,000 TRAVEL & TRANSPORTATION 131,860,000 57,874,000 75,996,000 265,730,000 88,576,667 GOVT. SERVANTS 131,860,000 57,874,000 75,996,000 265,730,000 88,576,667 A03801 Training -Domestic (all training s &TOT) for 03 trainings 82,350,000 22,300,000 27,750,000 132,400,000 44,133,333 A03805 T.A (Govt. Servants) 500,000 500,000 500,000 1,500,000 500,000 A033 A03303 A034 A03407 A038 106 A03806 Transportation of Goods 25,000,000 3,000,000 3,000,000 31,000,000 10,333,333 A03807 POL Charges 24,000,000 32,064,000 44,736,000 100,800,000 33,600,000 A03808 Local Conveyance Charges 10,000 10,000 10,000 30,000 10,000 A039 GENERAL 419,414,213 542,544,846 617,790,618 1,579,749,677 526,583,226 A03901 Stationary 100,000 100,000 100,000 300,000 100,000 4,000,000 4,000,000 2,000,000 10,000,000 3,333,333 600,000 600,000 600,000 1,800,000 600,000 10,000 10,000 10,000 30,000 10,000 2,000,000 2,000,000 2,000,000 6,000,000 2,000,000 5,000 5,000 5,000 15,000 5,000 A03902 A03903 Printing and Publication ( MIS Tools, Training manuals , BCC Material etc Conference /Siminars/Workshops/Symposium/ Review Meetings A03905 News Papers, Periodicals & Books A03907 Advertising & Publicity A03917 Law Charges A03927 Purchase of Drug and Medicines & Tab Iron Folic Acid for Nutrition 410,299,213 533,429,846 612,115,618 1,555,844,677 518,614,892 A03970 Others ( Supplies for nutrition components & consumables) 2,400,000 2,400,000 960,000 5,760,000 1,920,000 A04 EMPLOYEES RETIREMENT BENEFITS 312,804 312,804 312,804 938,412 312,804 A041 PENSION 312,804 312,804 312,804 938,412 312,804 A04101 Pension Contribution 140,004 140,004 140,004 420,012 140,004 A04115 Social Security Benefits to Contract Employees (30%) 172,800 172,800 172,800 518,400 172,800 Entertainment & Gift 10,000 10,000 10,000 30,000 10,000 A06301 Entertainment & Gift 10,000 10,000 10,000 30,000 10,000 A09 PHYSICAL ASSETS 1,302,996,603 2,108,327,890 2,077,909,344 5,489,233,837 1,829,744,612 A092 COMPUTER EQUIPMENT 5,200,000 2,600,000 2,400,000 10,200,000 3,400,000 A09202 Software ( Call Response center+ Web based MIS etc) 2,000,000 1,000,000 800,000 3,800,000 1,266,667 A09203 IT Equipment 3,200,000 1,600,000 1,600,000 6,400,000 2,133,333 1,117,946,603 1,975,427,890 1,926,534,344 5,019,908,837 1,673,302,946 550,000,000 300,000,000 850,000,000 283,333,333 A06 A094 OTHER STORE AND STOCK A09401 Medical Stores (Contraceptives) A09470 OTHER STORE AND STOCK A096 A09601 A097 A09701 1,117,946,603 1,425,427,890 1,626,534,344 4,169,908,837 1,389,969,612 PLANT AND MACHINERY 177,000,000 128,400,000 147,150,000 452,550,000 150,850,000 MACHINERY AND EQUIPMENT 177,000,000 128,400,000 147,150,000 452,550,000 150,850,000 FURNITURE AND FIXTURE 2,850,000 1,900,000 1,825,000 6,575,000 2,191,667 Furniture and Fixture 2,850,000 1,900,000 1,825,000 6,575,000 2,191,667 A13 REPAIRS AND MAINTENANCE 948,000 948,000 948,000 2,844,000 948,000 A130 TRANSPORT 848,000 848,000 848,000 2,544,000 848,000 Transport 848,000 848,000 848,000 2,544,000 848,000 COMPUTER EQUIPMENT 100,000 100,000 100,000 300,000 100,000 Software 100,000 100,000 100,000 300,000 100,000 2,446,012,005 3,502,247,924 3,865,911,150 9,814,171,078 3,271,390,359 A13001 A137 A13702 TOTAL 107 Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program Budget Requirement for Financial Year 2013-14 Object Heads A01 EMPLOYEE RELATED EXPENSES 588,210,384 PAY 1,719,600 PAY OF OFFICERS 1,719,600 A01101 Basic Pay A01106 Pay of Contract Staff A012 Budget Demand 600,000 1,119,600 ALLOWANCES 586,490,784 REGULAR ALLOWANCES 53,930,784 A01202 House Rent Allowance 229,296 A01203 Conveyance Allowance 240,000 A01217 Medical Allowance 146,544 A01236 Deputation Allowance 72,000 A01243 Special Travelling Allowance (FTA) A01252 Non Practicing Allowance 48,000 A01964 Special Additional Allowance (50% 2010) 488,400 Adhoc Relief Allowance (15% 2011) 146,544 A0 1970 OTHER ALLOWANCES 52,560,000 532,560,000 A01271 Over Time Allownace 10,000 A01273 Honorarium/Incentive for performance/ A01274 Medical Charges A01277 Contingent Paid staff 25,500,000 A01299 Other (Stipend of LHVs, Ayas, Ambulance Drivers & Guards) 462,840,000 A03 OPERATING EXPENSES 553,534,213 A032 COMMUNICATION 44,160,000 50,000 1,160,000 A03201 Postage and Telegraph 20,000 A03202 Telephone and Trunk Calls Charges 100,000 A03203 Telex. Teleprinter and Fax 40,000 A03204 Electronic communication ( E - Governance + Internet Charges) 800,000 A03205 Courior and Pilot Services 200,000 UTILITIES 600,000 Electricity Charges 600,000 OCCUPANCY COSTS 500,000 Rates & Taxes( Vehicles Tax & Toll Tax) 500,000 A033 A03303 A034 A03407 A038 TRAVEL & TRANSPORTATION 131,860,000 GOVT. SERVANTS 131,860,000 A03801 Training -Domestic (all training s &TOT) for 03 trainings 82,350,000 A03805 T.A (Govt. Servants) A03806 Transportation of Goods 500,000 25,000,000 108 A03807 POL Charges A03808 Local Conveyance Charges 24,000,000 10,000 A039 GENERAL 419,414,213 A03901 Stationary 100,000 A03902 Printing and Publication ( MIS Tools, Training manuals , BCC Material etc A03903 Conference /Siminars/Workshops/Symposium/ Review Meetings 600,000 A03905 News Papers, Periodicals & Books 10,000 A03907 Advertising & Publicity A03917 Law Charges A03927 Purchase of Drug and Medicines & Tab Iron Folic Acid for Nutrition A03970 Others ( Supplies for nutrition components & consumables) 4,000,000 2,000,000 5,000 410,299,213 2,400,000 A04 EMPLOYEES RETIREMENT BENEFITS 312,804 A041 PENSION 312,804 A04101 Pension Contribution 140,004 A04115 Social Security Benefits to Contract Employees (30%) 172,800 Entertainment & Gift 10,000 A06301 Entertainment & Gift 10,000 A09 PHYSICAL ASSETS 1,302,996,603 A092 COMPUTER EQUIPMENT A06 5,200,000 A09201 Hardware A09202 Software ( Call Response center+ Web based MIS etc) 2,000,000 A09203 IT Equipment 3,200,000 A094 OTHER STORE AND STOCK A09401 Medical Stores (Contracepitves) A09470 OTHER STORE AND STOCK A096 A09601 A097 A09701 1,117,946,603 1,117,946,603 PLANT AND MACHINERY 177,000,000 MACHINERY AND EQUIPMENT 177,000,000 FURNITURE AND FIXTURE 2,850,000 Furniture and Fixture 2,850,000 A13 REPAIRS AND MAINTENANCE 948,000 A130 TRANSPORT 848,000 Transport 848,000 COMPUTER EQUIPMENT 100,000 A13001 A137 A13702 Software 100,000 TOTAL 2,446,012,005 109 Budget Requirement for transport ( Ambulances ) For the Financial Year 2013-14 Sr. No. 1 Name of District Ambulances Total Budget Required No. of Vehicles 100 A-03807 POL A-13001 ROT Total Budget Required 24,000,000 4,200,000 28,200,000 41,472,000 848,000 49,952,000 110 Budget Requirement of POL (A-03807) For the Financial Year 2013-14 Sr. No. 1 Name of District Ambulances No. of Vehicles Rate Per Month No. of Months Total POL Budget Required 100 20,000 12 24,000,000 Total Budget Required 24,000,000 111 Budget Requirement of A-13001 Repair (Vehicle/Transport) For the Financial Year 2013-14 Sr. No. 1 Name of District Ambulances No. of Vehicles Repair of Vehicle @ Rs. 2500/- P.m. Total Budget for Repair of Vehicle Required 100 4,200,000 4,200,000 Total Budget Required 4,200,000 112 Budget Demand under the Head A-03801 Training Domestic for the Financial Year 2013-14 Unit Cost Training No. of Days Total Amount 300 2000 5 3,000,000.00 Training on IMNCI 300 3000 11 9,900,000.00 3 Training of LHWs & CMWs on Nutrition & IYCF 8000 900 4 28,800,000.00 4 Training of Medical officer on PHC & Nutrition 300 2500 3 2,250,000.00 5 Training of HCPs on EmONC & FP 600 2000 7 8,400,000.00 6 Training of LHWs LHSs on HTSP & FP 15000 500 4 30,000,000.00 Sr. No. Cadre No. of Posts 1 Training of HCPs on Nutrition and IYCF 2 Total 82,350,000.00 Grand Total 82,350,000.00 113 COST OF MEDICINES CHARAM (24/7) Category # of Units Unit Cost per month # of Months Total RHCs 162 3000 12 5832000 Basic Health Units 300 2500 12 9000000 Total 14,832,000 114 Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program Recurring Costs Category PMU Managerial Staff Number Unit Cost/ Monthly Monthly Total Annual Total (Rs) Annual Total $ - 52,560,000 192,720,000 108,000,000 50,400,000 27,000,000 24,000,000 9,000,000 24,000,000 - FTA for WMO 292 15000 WMO 292 55000 LHVs 600 15000 Ayas 600 7000 Security Guards 300 7500 Drivers 200 10000 Medicines 300 2500 FP Material 0 0 Pay for performance 40 50000 4,380,000 16,060,000 9,000,000 4,200,000 2,250,000 2,000,000 750,000 2,000,000 Consumables (Lab Kits and gloves) 300 2000 600,000 7,200,000 83,720.93 Petty Cash 300 2000 100 16500 7,200,000 19,800,000 83,720.93 POL for ambulances 600,000 1,650,000 230,232.56 Operational Cost ( POL & Office suplies) 1 0 - - - TA/DA 1 0 0 0 - - Miscellaneous - Operational Cost ( POL, Repair of transport & Office suplies) 20 0 - - - Miscellaneous 20 10000 20 50000 Medicines 162 3500 Additional HR 45 25000 PGRs 40 0 Advertisements 1 MRM @ District 20 10000 2,400,000 12,000,000 6,804,000 13,500,000 2,000,000 2,400,000 27,906.98 Additional HR 200,000 1,000,000 567,000 1,125,000 200,000 Quarterly Review Meeting & Dissemination 4 150000 600,000 600,000 Chairperson 1 Program Director 1 Deputy PD 1 Human Resource Manger 1 Finance Manager 1 MIS Manager 1 Office Assistant 1 - District Manager M & E Officer DSU Data Entry Program Assistant Accounts Officer BHU PMU DSU RHCs THQ Overall Operational Costt 611,162.79 2,240,930.23 1,255,813.95 586,046.51 313,953.49 279,069.77 104,651.16 279,069.77 - 139,534.88 79,116.28 156,976.74 23,255.81 27,906.98 6,976.74 115 Call Response Center 20 100000 Printing 4 150000 2,000,000 600,000 Total 2,000,000 600,000 561,584,000 23,255.81 6,976.74 6,530,046.51 One Time Cost BHU 0 35000 Ambulances Furniture & Fixture for DSU IT Equipment (Laptop, PC, desktop, Printer, Fax) 100 0 45,000,000 10,500,000 2,850,000 - 16 0 - - - 16 200000 3,200,000 3,200,000 37,209.30 USG Portable 150 500000 15 0 Equipment for RHCs Equipment for THQs/DHQs 20 800000 75,000,000 16,000,000 872,093.02 Repair & Renovation 75,000,000 16,000,000 50 400,000 20,000,000 20,000,000 232,558.14 - - - 172,550,000 2,006,395.35 Basic Equipment for BHUs 300 150000 UPS with Battries 300 35000 F&F for BHUs 300 9500 Computers & Printer DSU/RSU RHCs THQ& DHQ 0 Total 45,000,000 10,500,000 2,850,000 - 523,255.81 122,093.02 33,139.53 - 186,046.51 - Annual Cost 561,584,000 Two Years Cost 1,123,168,000 One Time Cost 172,550,000 Total (Rs) 1,295,718,000 Total $ 14,724,068 116 Budget Requirement under Head A-01299 Others (Stipend of LHVs/Ayas/Ambulance Drivers & Guards for the Financial Year 2013-14 Sr. No. Cadre # of Health Facilities 1 Nursing Staff (for DHQ Nutrition) 2 3 Budget Requirement in Rs. Strength Net Pay Period 34 DHQ +2 Teaching hospital 72 30000 12 25920000 WMO 292 RHCs 292 55000 12 192720000 Computer Operator PMU 2 25000 12 600000 600 17000 12 122,400,000 600 9000 12 64,800,000 200 10000 12 24,000,000 300 9000 12 32,400,000 4 LHVs (CHARM) 300 BHUs 5 Aya (CHARM) 300 BHUs 6 Ambulance drivers (CHARM) 7 Gaurds (CHARM) Total 300 BHUs BPS Fixed Salary 2066 462,840,000.00 117 Summary for Budget Requirement of Salary of Nutrition Program Staff working in Scales for the period July-2013 to June 2014 during the financial year 2013-14 Sr. No. Particulars A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA A01224 Entertainment Allow. A01217 Medical Allow A01964 SAA (2010) SPHA Comp Allow A04115 Social Security 30% A-01970 Adhoc Relief Allow. 15% 20% Adhoc Relief Allowance (2012) Total 1 Staff Salary July to Nov-13 250,000 0 0 456,000 0 95,540 100,000 30,000 20,000 0 61,060 203,500 56,000 0 72,000 61,060 91,200 1,496,360 2 Staff Salary Dec to June-14 350,000 0 0 663,600 0 133,756 140,000 42,000 28,000 0 85,484 284,900 78,400 0 100,800 85,484 132,720 2,125,144 600,000 0 0 1,119,600 0 229,296 240,000 72,000 48,000 0 146,544 488,400 134,400 0 172,800 146,544 223,920 3,621,504 Total Budget Requirement for 2013-14 118 Budget Requirement of Salary for the staff of Nutrition Program Punjab for the period Dec-13 to June-2014 Sr. No. Particulars BPS A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA Entertainment Allow A01217 Medical Allow SAA (2010) SPHA 4448 14825 11200 4448 14825 11200 Comp Allow Adhoc Relief Allow. 15% Adhoc Relief Allow. 20% Total 4448 0 105730 0 4448 0 105730 Social Security 30% 01 Posts of BPS-18 1 Program Manager Nutrition 19 Total 50000 50000 0 0 0 0 5809 5000 6000 4000 5809 5000 6000 4000 0 0 03 Posts of BPS-17 1 Nutrition Officer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 2 Software Engineer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 3 Statestical Officer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 Total Total PMU Salary for one Month Budget for Dec-13 to June-14 0 0 0 94800 0 13299 15000 0 0 0 7764 25875 0 0 14400 7764 18960 197862 50,000 0 0 94,800 0 19,108 20,000 6,000 4,000 0 12,212 40,700 11,200 0 14,400 12,212 18,960 303,592 350,000 0 0 663,600 0 133,756 140,000 42,000 28,000 0 85,484 284,900 78,400 0 100,800 85,484 132,720 2,125,144 119 Budget Requirement of Salary for the staff of Nutrition Program Punjab for the period July-13 to Nov-13 Sr. No. Particulars BPS A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA Entertainment Allow A01217 Medical Allow SAA (2010) SPHA 4448 14825 11200 4448 14825 11200 Comp Allow Adhoc Relief Allow. 15% Adhoc Relief Allow. 20% Total 4448 0 105730 0 4448 0 105730 Social Security 30% 01 Posts of BPS-18 1 Program Manager Nutrition 18 Total 50000 50000 0 0 0 0 5809 5000 6000 4000 5809 5000 6000 4000 0 0 03 Posts of BPS-17 1 Nutrition Officer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 2 Software Engineer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 3 Statestical Officer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 15000 25875 0 0 14400 7764 18240 193542 0 0 0 Total PMU Salary for one Month Total 91200 0 13299 50,000 0 Budget for July 13 to Nov-13 250,000 0 0 91,200 0 19,108 20,000 0 456,000 0 95,540 100,000 0 0 0 7764 6,000 4,000 0 12,212 40,700 11,200 0 14,400 12,212 18,240 299,272 30,000 20,000 0 61,060 203,500 56,000 0 72,000 61,060 91,200 1,496,360 120 Cost Sheet of Nutrition Budget for the Financial Year 2013-14 S.No Districts Total population of districts 50%Target Population For 12 District & for 09 Urban slam Districts is 25% Total children age 6 to 59 month 14 % Narowal 1516173 758086.5 1486000 743000 1 MICs 2010-11 # of target Children SAM 30 % + 2% relapse & incidence rate ( 4% of Total target population) Cost per SAM Child # children age 6 month to 2 years Cost per Multinutrient supplementation for 6 month to 2 years # children age 2 to 5 years Cost for tab. Mebandazole Total PLW7.5 % 13 % MAM PLW + 1.5 % Relapse & Incidence rate Cost per PLW Cost for Tab.Iron Folic Acid SC Cost (F 75 & F 100) Cost for Anthropometry Equipment Total Cost for Supplies 16 106132 16981 5298 21192460 30323 6822779 56856 341139 56856 7650 12240065 7107061 100000 500000 48303503 104020 14 14563 4544 18174374 29720 6687000 55725 334350 55725 7498 11996478 6965625 100000 500000 44757827 91630 21 19242 6004 24014390 26180 5890500 49088 294525 49088 6573 10516506 6135938 100000 500000 47451859 279580 20 55916 17446 69783168 79880 17973000 149775 898650 149775 20055 32087796 18721875 100000 500000 140064489 19.7 15607 4869 19477947 22636 5093037 42442 254652 42442 5683 9092769 5305247 100000 500000 39823651 293860 19 55833 17420 69680083 83960 18891000 157425 944550 157425 30698 49116600 19678125 100000 500000 158910358 113190 19 21506 6710 26839613 32340 7276500 60638 363825 60638 11824 18918900 7579688 100000 500000 61578525 155330 19 29513 9208 36831850 44380 9985500 83213 499275 83213 16226 25962300 10401563 100000 500000 84280487 250530 17 42590 13288 53152445 71580 16105500 134213 805275 134213 26171 41874300 16776563 100000 500000 129314082 95771 26 24900 7769 31075612 27363 6156675 51306 307834 51306 10005 16007355 6413203 100000 500000 60560679 103950 13.7 14241 4443 17772955 29700 6682500 55688 334125 55688 10859 17374500 6960938 100000 500000 49725018 179620 17 30535 9527 38108179 51320 11547000 96225 577350 96225 18764 30022200 12028125 100000 500000 92882854 123312 13 16031 5002 20006139 35232 7927200 66060 396360 66060 12882 20610720 8257500 500000 57697919 89292 12 10715 3343 13372370 25512 5740200 47835 287010 47835 9328 14924520 5979375 500000 40803475 120988 13 15728 4907 19629093 34568 7777800 64815 388890 64815 12639 20222280 8101875 500000 56619938 191016 14 26742 8344 33374316 54576 12279600 102330 613980 102330 19954 31926960 12791250 500000 91486106 90076 14 12611 3935 15738079 25736 5790600 48255 289530 48255 9410 15055560 6031875 500000 43405644 62776 16 10044 3134 12535112 17936 4035600 33630 201780 33630 6558 10492560 4203750 500000 31968802 72380 21 15200 4742 18969350 20680 4653000 38775 232650 38775 7561 12097800 4846875 500000 41299675 96180 12 11542 3601 14403917 27480 6183000 51525 309150 51525 10047 16075800 6440625 500000 43912492 242200 14 33908 10579 42317184 69200 15570000 129750 778500 129750 25301 40482000 16218750 500000 115866434 493949 154112 ###### 9453400 1575567 Layyah 2 Mianwali 1309000 654500 3994000 1997000 3 Multan 4 Khushab 1131786 565893 4198000 2099000 1617000 808500 5 79225 Rahimyar Khan 6 Pakpattan 7 D. G. Khan 2219000 1109500 8 Muzaffargarh 3579000 1789500 1368150 684075 9 Bhakkar 10 Rajanpur 1485000 742500 11 Bhawal Nagar 2566000 1283000 4404000 880800 12 Gujranwala 13 Sargodha 3189000 637800 14 Rawalpindi 4321000 864200 6822000 1364400 15 Faisalabad 16 Bhawal Pur 3217000 643400 17 Sahiwal 2242000 448400 18 Khanewal 2585000 517000 3435000 687000 19 Sialkot 20 Lahore 8650000 1730000 21 ####### ####### ###### ########## 840302 ######## 285,686 ######## ########## ######## 10,500,000 1,480,713,817 121 Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program Budget Requirement for Financial Year 2014-15 Object Heads A01 EMPLOYEE RELATED EXPENSES 789,970,384 PAY 1,719,600 PAY OF OFFICERS 1,719,600 A01101 Basic Pay A01106 Pay of Contract Staff A012 Budget Demand 600,000 1,119,600 ALLOWANCES 788,250,784 REGULAR ALLOWANCES 53,930,784 A01202 House Rent Allowance 229,296 A01203 Conveyance Allowance 240,000 A01217 Medical Allowance 146,544 A01236 Deputation Allowance 72,000 A01243 Special Travelling Allowance (FTA) A01252 Non Practicing Allowance 48,000 A01964 Special Additional Allowance (50% 2010) 488,400 Adhoc Relief Allowance (15% 2011) 146,544 A0 1970 OTHER ALLOWANCES 52,560,000 734,320,000 A01271 Over Time Allownace 10,000 A01273 Honorarium/Incentive for performance/ 44,160,000 A01274 Medical Charges 6,804,000 A01277 Contingent Paid staff 25,500,000 A01299 Other (Stipend of LHVs, Ayas, Ambulance Drivers & Guards) 657,846,000 A03 OPERATING EXPENSES 602,678,846 A032 COMMUNICATION 1,160,000 A03201 Postage and Telegraph 20,000 A03202 Telephone and Trunk Calls Charges 100,000 A03203 Telex. Teleprinter and Fax 40,000 A03204 Electronic communication ( E - Governance + Internet Charges) 800,000 A03205 Courior and Pilot Services 200,000 UTILITIES 600,000 Electricity Charges 600,000 OCCUPANCY COSTS 500,000 Rates & Taxes( Vehicles Tax & Toll Tax) 500,000 A033 A03303 A034 A03407 A038 TRAVEL & TRANSPORTATION 57,874,000 GOVT. SERVANTS 57,874,000 A03801 Training -Domestic (all training s &TOT) for 03 trainings 22,300,000 A03805 T.A (Govt. Servants) A03806 Transportation of Goods 500,000 3,000,000 122 A03807 POL Charges A03808 Local Conveyance Charges 32,064,000 10,000 A039 GENERAL 542,544,846 A03901 Stationary 100,000 A03902 Printing and Publication ( MIS Tools, Training manuals , BCC Material etc A03903 Conference /Siminars/Workshops/Symposium/ Review Meetings 600,000 A03905 News Papers, Periodicals & Books 10,000 A03907 Advertising & Publicity A03917 Law Charges A03927 Purchase of Drug and Medicines & Tab Iron Folic Acid for Nutrition A03970 Others ( Supplies for nutrition components & consumables) 4,000,000 2,000,000 5,000 533,429,846 2,400,000 A04 EMPLOYEES RETIREMENT BENEFITS 312,804 A041 PENSION 312,804 A04101 Pension Contribution 140,004 A04115 Social Security Benefits to Contract Employees (30%) 172,800 Entertainment & Gift 10,000 A06301 Entertainment & Gift 10,000 A09 PHYSICAL ASSETS 2,108,327,890 A092 COMPUTER EQUIPMENT 2,600,000 A09202 Software ( Call Response center+ Web based MIS etc) 1,000,000 A09203 IT Equipment 1,600,000 A06 A094 OTHER STORE AND STOCK A09401 Medical Stores (Contraceptives) A09470 OTHER STORE AND STOCK A096 A09601 A097 A09701 1,975,427,890 550,000,000 1,425,427,890 PLANT AND MACHINERY 128,400,000 MACHINERY AND EQUIPMENT 128,400,000 FURNITURE AND FIXTURE 1,900,000 Furniture and Fixture 1,900,000 A13 REPAIRS AND MAINTENANCE 948,000 A130 TRANSPORT 848,000 Transport 848,000 COMPUTER EQUIPMENT 100,000 Software 100,000 A13001 A137 A13702 TOTAL 3,502,247,924 123 Budget Requirement for DPIU's/PPIUs in Punjab For the Financial Year 2014-15 Sr. No. 1 Name of District Ambulances Total Budget Required No. of Vehicles A-03807 POL A-13001 ROT Total Budget Required 167 32,064,000 6,509,000 38,573,000 41,472,000 848,000 49,952,000 124 Budget Requirement of POL (A-03807) For the Financial Year 2014-15 Sr. No. 1 Name of District Ambulances No. of Vehicles Rate Per Month No. of Months Total POL Budget Required 167 17,000 12 32,064,000 Total Budget Required 32,064,000 125 Budget Requirement of A-13001 Repair (Vehicle/Transport) For the Financial Year 2014-15 Sr. No. 1 Name of District Ambulances No. of Vehicles Repair of Vehicle @ Rs. 22500/- P.m. Budget required for major repair and change of tyres Total Budget for Repair of Vehicle Required 167 4,509,000 2,000,000 6,509,000 Total Budget Required 6,509,000 126 Budget Demand under the Head A-03801 Training Domestic For the Financial Year 2014-15 Sr. No. Cadre No. of Posts Unit Cost Training No. of Days Total Amount 200 2000 5 2,000,000.00 0 3000 11 - 1 Training of HCPs on Nutrition and IYCF 2 Training on IMNCI 3 Training of LHWs & CMWs on Nutrition & IYCF 10000 400 4 16,000,000.00 4 Training of Medical officer on PHC & Nutrition 200 2500 3 1,500,000.00 5 Training of HCPs on EmONC & FP 200 2000 7 2,800,000.00 Total 22,300,000.00 127 COST OF MEDICINES (Charam 24/7) # of Units Unit Cost per month # of Months Total RHCs 162 3000 12 5832000 Basic Health Units 500 3000 12 18000000 Category Total 23,832,000 128 Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program Recurring Costs FTA for WMO 292 15000 WMO 292 55000 LHVs 1000 15000 Ayas 1000 7000 Security Guards 500 7500 Drivers 333 9000 Medicines 500 2500 FP Material 0 0 Pay for performance 40 50000 Monthly Total 4,380,000 16,060,000 15,000,000 7,000,000 3,750,000 2,997,000 1,250,000 2,000,000 Consumables (Lab Kits and gloves) 500 2000 1,000,000 12,000,000 139,534.88 Petty Cash 200 2000 167 16000 4,800,000 32,064,000 55,813.95 POL for ambulances 400,000 2,672,000 372,837.21 Operational Cost ( POL & Office suplies) 1 0 - - - TA/DA 1 0 0 0 - - Miscellaneous - Operational Cost ( POL, Repair of transport & Office suplies) 20 0 - - - Miscellaneous 20 10000 20 50000 Medicines 162 3500 Additional HR 45 25000 PGRs 40 0 Advertisements 1 MRM @ District 10 10000 2,400,000 12,000,000 6,804,000 13,500,000 2,000,000 1,200,000 27,906.98 Additional HR 200,000 1,000,000 567,000 1,125,000 100,000 Quarterly Review Meeting & Dissemination 4 150000 600,000 600,000 Category PMU Managerial Staff Number Chairperson 1 Program Director 1 Deputy PD 1 Human Resource Manger 1 Finance Manager 1 MIS Manager 1 Office Assistant 1 Unit Cost/ Monthly - District Manager M & E Officer DSU Data Entry Program Assistant Accounts Officer BHU PMU DSU RHCs THQ Overall Operational Costt Annual Total (Rs) 52,560,000 192,720,000 180,000,000 84,000,000 45,000,000 35,964,000 15,000,000 24,000,000 Annual Total $ 611,162.79 2,240,930.23 2,093,023.26 976,744.19 523,255.81 418,186.05 174,418.60 279,069.77 - 139,534.88 79,116.28 156,976.74 23,255.81 13,953.49 6,976.74 129 Call Response Center 10 100000 Printing 4 150000 1,000,000 600,000 Total 1,000,000 600,000 716,612,000 11,627.91 6,976.74 8,332,697.67 One Time Cost BHU 0 35000 Ambulances Furniture & Fixture for DSU IT Equipment (Laptop, PC, desktop, Printer, Fax) 167 0 30,000,000 7,000,000 1,900,000 - 0 50000 - - - 8 200000 1,600,000 1,600,000 18,604.65 USG Portable 100 500000 20 0 Equipment for RHCs Equipment for THQs/DHQs 8 800000 50,000,000 6,400,000 581,395.35 Repair & Renovation 50,000,000 6,400,000 40 500000 20,000,000 20,000,000 232,558.14 - - - 116,900,000 1,359,302.33 Basic Equipment for BHUs 200 150000 UPS with Battries 200 35000 F&F for BHUs 200 9500 Computers & Printer DSU/RSU RHCs THQ& DHQ 0 Total 30,000,000 7,000,000 1,900,000 - 348,837.21 81,395.35 22,093.02 - 74,418.60 - Annual Cost 716,612,000 Two Years Cost 1,433,224,000 One Time Cost 116,900,000 Total (Rs) Total $ 1,550,124,000 17,615,045 130 Budget Requirement under Head A-01299 Others (Stipend of LHVs/Ayas/Ambulance Drivers & Guards for the Financial Year 2014-15 Strength Net Pay Period Budget Requirement in Rs. 34 DHQ +2 Teaching hospital 72 31000 12 26784000 292 RHCs 292 57500 12 201480000 2 26000 12 624000 1000 18000 12 216,000,000 1000 9500 12 114,000,000 333 10500 12 41,958,000 500 9500 12 57,000,000 Sr. No. Cadre # of Health Facilities 1 Nursing Staff (for DHQ Nutrition) 2 WMO 3 Computer Operator PMU 4 LHVs (CHARM) 500 BHUs 5 Aya (CHARM) 500 BHUs 6 Ambulance drivers (CHARM) 7 Gaurds (CHARM) Total BPS 500 BHUS Fixed Salary 3199 657,846,000.00 131 Summary for Budget Requirement of Salary of Nutrition Program Staff working in Scales for the period July-2014 to June 2015 during the financial year 2014-15 Sr. No. Particulars A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA A01224 Entertainment Allow. A01217 Medical Allow A01964 SAA (2010) SPHA Comp Allow A04115 Social Security 30% A-01970 Adhoc Relief Allow. 15% 20% Adhoc Relief Allowance (2012) Total 1 Staff Salary July to Nov-14 250,000 0 0 456,000 0 95,540 100,000 30,000 20,000 0 61,060 203,500 56,000 0 72,000 61,060 91,200 1,496,360 2 Staff Salary Dec to June-15 350,000 0 0 663,600 0 133,756 140,000 42,000 28,000 0 85,484 284,900 78,400 0 100,800 85,484 132,720 2,125,144 600,000 0 0 1,119,600 0 229,296 240,000 72,000 48,000 0 146,544 488,400 ##### 0 172,800 146,544 223,920 3,621,504 Total Budget Requirement for 2014-15 132 Budget Requirement of Salary for the staff of Nutrition Program Punjab for the period Dec-14 to June-2015 Sr. No. Particulars BPS A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA Entertainment Allow A01217 Medical Allow SAA (2010) SPHA 4448 14825 11200 4448 14825 11200 Comp Allow Adhoc Relief Allow. 15% Adhoc Relief Allow. 20% Total 4448 0 105730 0 4448 0 105730 Social Security 30% 01 Posts of BPS-18 1 Program Manager Nutrition 19 Total 50000 50000 0 0 0 0 5809 5000 6000 4000 5809 5000 6000 4000 0 0 03 Posts of BPS-17 1 Nutrition Officer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 2 Software Engineer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 3 Statestical Officer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 Total Total PMU Salary for one Month Budget for Dec-14 to June-15 0 0 0 94800 0 13299 15000 0 0 0 7764 25875 0 0 14400 7764 18960 197862 50,000 0 0 94,800 0 19,108 #### 6,000 4,000 0 12,212 40,700 11,200 0 14,400 12,212 18,960 303,592 350,000 0 0 663,600 0 133,756 #### 42,000 28,000 0 85,484 #### #### 0 #### 85,484 132,720 ##### 133 Budget Requirement of Salary for the staff of Nutrition Program Punjab for the period July-14 to Nov-14 Sr. No. Particulars BPS A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA Entertainment Allow A01217 Medical Allow SAA (2010) SPHA 4448 14825 11200 4448 14825 11200 Comp Allow Adhoc Relief Allow. 15% Adhoc Relief Allow. 20% Total 4448 0 105730 0 4448 0 105730 Social Security 30% 01 Posts of BPS-18 1 Program Manager Nutrition 18 Total 50000 50000 0 0 0 0 5809 5000 6000 4000 5809 5000 6000 4000 0 0 03 Posts of BPS-17 1 Nutrition Officer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 2 Software Engineer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 3 Statestical Officer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 Total Total PMU Salary for one Month Budget for July 14 to Nov14 0 0 0 91200 0 13299 15000 0 0 0 7764 25875 0 0 14400 7764 18240 193542 50,000 0 0 91,200 0 19,108 20,000 6,000 4,000 0 12,212 40,700 11,200 0 14,400 12,212 18,240 299,272 250,000 0 0 456,000 0 95,540 100,000 30,000 20,000 0 61,060 203,500 56,000 0 72,000 61,060 91,200 1,496,360 134 Cost Sheet of Nutrition Budget for the Financial Year 2014-15 S.No Districts Total population of districts 50%Target Population For 21 District & for 09 Urban slam Districts is 25% SAM 30 % + 2% relapse & incidence rate ( 4% of Total target population) Cost per SAM Child 1 Narowal 1516173 758086.5 106132 2 Layyah 1486000 743000 104020 16 16981 5298 21192460 30323 6822779 56856 341139 56856 7650 12240065 7107061 100000 500000 48303503 14 14563 4544 18174374 29720 6687000 55725 334350 55725 7498 11996478 6965625 100000 500000 3 Mianwali 1309000 654500 44757827 91630 21 19242 6004 24014390 26180 5890500 49088 294525 49088 6573 10516506 6135938 100000 500000 4 Multan 3994000 1997000 47451859 279580 20 55916 17446 69783168 79880 17973000 149775 898650 149775 20055 32087796 18721875 100000 500000 140064489 5 Khushab 1131786 565893 79225 6 Rahimyar Khan 4198000 2099000 293860 19.7 15607 4869 19477947 22636 5093037 42442 254652 42442 5683 9092769 5305247 100000 500000 39823651 19 55833 17420 69680083 83960 18891000 157425 944550 157425 30698 49116600 19678125 100000 500000 158910358 7 Pakpattan 1617000 808500 8 D. G. Khan 2219000 1109500 113190 19 21506 6710 26839613 32340 7276500 60638 363825 60638 11824 18918900 7579688 100000 500000 61578525 155330 19 29513 9208 36831850 44380 9985500 83213 499275 83213 16226 25962300 10401563 100000 500000 9 Muzaffargarh 3579000 1789500 84280487 250530 17 42590 13288 53152445 71580 16105500 134213 805275 134213 26171 41874300 16776563 100000 500000 129314082 10 Bhakkar 1368150 11 Rajanpur 1485000 684075 95771 26 24900 7769 31075612 27363 6156675 51306 307834 51306 10005 16007355 6413203 100000 500000 60560679 742500 103950 13.7 14241 4443 17772955 29700 6682500 55688 334125 55688 10859 17374500 6960938 100000 500000 12 Bhawal Nagar 49725018 2566000 1283000 179620 17 30535 9527 38108179 51320 11547000 96225 577350 96225 18764 30022200 12028125 100000 500000 13 92882854 Gujranwala 4404000 1321200 184968 14 25896 8079 32317609 52848 11890800 99090 594540 99090 19323 30916080 12386250 500000 88605279 14 Sargodha 3189000 956700 133938 15 20091 6268 25073194 38268 8610300 71753 430515 71753 13992 22386780 8969063 500000 65969851 15 Rawalpindi 4321000 1296300 181482 13 23593 7361 29443640 51852 11666700 97223 583335 97223 18958 30333420 12152813 500000 84679907 16 Faisalabad 6822000 2046600 286524 14 40113 12515 50061473 81864 18419400 153495 920970 153495 29932 47890440 19186875 500000 136979158 17 Bhawal Pur 3217000 965100 135114 14 18916 5902 23607118 38604 8685900 72383 434295 72383 14115 22583340 9047813 500000 64858466 18 Sahiwal 2242000 672600 94164 16 15066 4701 18802668 26904 6053400 50445 302670 50445 9837 15738840 6305625 500000 47703203 19 Attock 1562000 390500 54670 13 7107 2217 8869661 15620 3514500 29288 175725 29288 5711 9137700 3660938 500000 25858523 20 Chiniot 1156000 289000 40460 14 5664 1767 7069171 11560 2601000 21675 130050 21675 4227 6762600 2709375 500000 19772196 21 Gujrat 2509000 627250 87815 9 7903 2466 9863381 25090 5645250 47044 282263 47044 9174 14677650 5880469 500000 36849012 22 Hafizabad 1024000 204800 28672 14 4014 1252 5009572 8192 1843200 15360 92160 15360 2995 4792320 1920000 500000 14157252 23 Jhang 2333331 466666.2 65333 14 9147 2854 11415029 18667 4199996 35000 210000 35000 6825 10919989 4374996 500000 31620009 24 Jhelum 1134000 226800 31752 13 4128 1288 5151444 9072 2041200 17010 102060 17010 3317 5307120 2126250 500000 15228074 25 Kasur 3016000 603200 84448 21 17734 5533 22132132 24128 5428800 45240 271440 45240 8822 14114880 5655000 500000 48102252 26 Khanewal 2585000 517000 72380 21 15200 4742 18969350 20680 4653000 38775 232650 38775 7561 12097800 4846875 500000 41299675 27 Lodhran 1504000 300800 42112 19 8001 2496 9985597 12032 2707200 22560 135360 22560 4399 7038720 2820000 500000 23186877 28 Vehari 2671000 534200 74788 23 17201 5367 21467148 21368 4807800 40065 240390 40065 7813 12500280 5008125 500000 44523743 29 Sialkot 3435000 687000 96180 12 11542 3601 14403917 27480 6183000 51525 309150 51525 10047 16075800 6440625 500000 43912492 30 Lahore 8650000 1730000 242200 14 33908 10579 42317184 69200 15570000 129750 778500 129750 25301 40482000 16218750 500000 115866434 ####### ####### 626653 195516 2030270 12181622 2030270 ###### MICs 2010-11 ######### # children age 6 month to 2 years Cost per Multinutrient supplementation for 6 month to 2 years # of target Children Total children age 6 to 59 month 14 % 1082811 243,632,436 # children age 2 to 5 years Cost for tab. Mebandazole Total PLW7.5 % 13 % MAM PLW + 1.5 % Relapse & Incidence rate 374,353 Cost per PLW ######## Cost for Tab.Iron Folic Acid ########## SC Cost (F 75 & F 100) ######## Cost for Anthropometry Equipment ######### Total Cost for Supplies 1,906,825,736 Potassium Iodate for Salt Iodization 1,906,825,736 135 Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program Budget Requirement for Financial Year 2015-16 Object Heads A01 EMPLOYEE RELATED EXPENSES 1,090,684,384 PAY 1,719,600 PAY OF OFFICERS 1,719,600 A01101 Basic Pay A01106 Pay of Contract Staff A012 Budget Demand ALLOWANCES REGULAR ALLOWANCES 600,000 1,119,600 1,088,964,784 71,450,784 A01202 House Rent Allowance 229,296 A01203 Conveyance Allowance 240,000 A01217 Medical Allowance 146,544 A01236 Deputation Allowance 72,000 A01243 Special Travelling Allowance (FTA) A01252 Non Practicing Allowance 48,000 A01964 Special Additional Allowance (50% 2010) 488,400 Adhoc Relief Allowance (15% 2011) 146,544 A0 1970 OTHER ALLOWANCES 70,080,000 1,017,514,000 A01271 Over Time Allownace 10,000 A01273 Honorarium/Incentive for performance/ 44,160,000 A01274 Medical Charges 6,804,000 A01277 Contingent Paid staff 18,300,000 A01299 Other (Stipend of LHVs, Ayas, Ambulance Drivers & Guards) 948,240,000 A03 OPERATING EXPENSES 696,046,618 A032 COMMUNICATION 1,160,000 A03201 Postage and Telegraph 20,000 A03202 Telephone and Trunk Calls Charges 100,000 A03203 Telex. Teleprinter and Fax 40,000 A03204 Electronic communication ( E - Governance + Internet Charges) 800,000 A03205 Courior and Pilot Services 200,000 UTILITIES 600,000 Electricity Charges 600,000 OCCUPANCY COSTS 500,000 A033 A03303 A034 A03403 Rent of Residential Bilding A03407 Rates & Taxes( Vehicles Tax & Toll Tax) A038 500,000 TRAVEL & TRANSPORTATION 75,996,000 GOVT. SERVANTS 75,996,000 A03801 Training -Domestic (all training s &TOT) for 03 trainings 27,750,000 A03805 T.A (Govt. Servants) 500,000 136 A03806 Transportation of Goods 3,000,000 A03807 POL Charges 44,736,000 A03808 Local Conveyance Charges 10,000 A039 GENERAL A03901 Stationary A03902 Printing and Publication ( MIS Tools, Training manuals , BCC Material etc A03903 Conference /Siminars/Workshops/Symposium/ Review Meetings 600,000 A03905 News Papers, Periodicals & Books 10,000 A03907 Advertising & Publicity A03917 Law Charges A03927 Purchase of Drug and Medicines & Tab Iron Folic Acid for Nutrition A03970 Others ( Supplies for nutrition components & consumables) 960,000 A04 EMPLOYEES RETIREMENT BENEFITS 312,804 A041 PENSION 312,804 A04101 Pension Contribution 140,004 A04115 Social Security Benefits to Contract Employees (30%) 172,800 Entertainment & Gift 10,000 A06301 Entertainment & Gift 10,000 A09 PHYSICAL ASSETS 2,077,909,344 A092 COMPUTER EQUIPMENT A06 617,790,618 100,000 2,000,000 5,000 Software ( Call Response center+ Web based MIS etc) A09203 IT Equipment Medical Stores (Contraceptives) A09470 OTHER STORE AND STOCK A096 A09601 A097 A09701 800,000 1,600,000 OTHER STORE AND STOCK A09401 612,115,618 2,400,000 A09202 A094 2,000,000 1,926,534,344 300,000,000 1,626,534,344 PLANT AND MACHINERY 147,150,000 MACHINERY AND EQUIPMENT 147,150,000 FURNITURE AND FIXTURE 1,825,000 Furniture and Fixture 1,825,000 A13 REPAIRS AND MAINTENANCE 948,000 A130 TRANSPORT 848,000 Transport 848,000 COMPUTER EQUIPMENT 100,000 A13001 A137 A13702 Software 100,000 TOTAL 3,865,911,150 137 Budget Requirement for DPIU's/PPIUs in Punjab For the Financial Year 2015-16 Sr. No. 1 Name of District Ambulances Total Budget Required No. of Vehicles A-03807 POL A-13001 ROT Total Budget Required 233 44,736,000 11,184,000 55,920,000 41,472,000 848,000 49,952,000 138 Budget Requirement of POL (A-03807) For the Financial Year 2015-16 Sr. No. 1 Name of District Ambulances No. of Vehicles Rate Per Month No. of Months Total POL Budget Required 233 20,000 12 44,736,000 Total Budget Required 44,736,000 139 Budget Requirement of A-13001 Repair (Vehicle/Transport) For the Financial Year 2015-16 Sr. No. 1 Name of District Ambulances No. of Vehicles Repair of Vehicle @ Rs. 2500/P.m. ( Major& Minor repair) Total Budget for Repair of Vehicle Required 233 11,184,000 11,184,000 Total Budget Required 11,184,000 140 Budget Demand under the Head A-03801 Training Domestic For the Financial Year 2015-16 Sr. No. Cadre 1 Training of HCPs on Nutrition and IYCF 2 Training on IMNCI 3 4 5 Training of LHWs & CMWs on Nutrition & IYCF Training of Medical officer on PHC & Nutrition Training of HCPs on EmONC & FP Total No. of Posts Unit Cost Training No. of Days Total Amount 200 1800 5 1,800,000.00 0 3000 11 - 8000 700 4 22,400,000.00 100 2500 3 750,000.00 200 2000 7 2,800,000.00 27,750,000.00 141 COST OF MEDICINES(Charam 24/7) Category # of Units Unit Cost per month # of Months Total RHCs 162 2500 12 4860000 Basic Health Units 700 2500 12 21000000 Total 25,860,000 142 Integrated Reproductive Maternal Newborn & Child Health &Nutrition Program Recurring Costs Category PMU Managerial Staff Number Unit Cost/ Monthly Monthly Total Annual Total (Rs) Annual Total $ - 70,080,000 210,240,000 252,000,000 117,600,000 126,000,000 50,328,000 21,000,000 24,000,000 - FTA for WMO 292 20000 WMO 292 60000 LHVs 1400 15000 Ayas 1400 7000 Security Guards 1400 7500 Drivers 466 9000 Medicines 700 2500 FP Material 0 0 Pay for performance 40 50000 5,840,000 17,520,000 21,000,000 9,800,000 10,500,000 4,194,000 1,750,000 2,000,000 Consumables (Lab Kits and gloves) 700 2000 1,400,000 16,800,000 195,348.84 Petty Cash 700 2000 233 16000 16,800,000 44,736,000 195,348.84 POL for ambulances 1,400,000 3,728,000 Operational Cost ( POL & Office suplies) 1 0 - - - TA/DA 1 0 0 0 - - Miscellaneous - Operational Cost ( POL, Repair of transport & Office suplies) 20 0 - - - Miscellaneous 8 10000 8 50000 Medicines 162 3500 Additional HR 45 25000 156,976.74 PGRs 40 0 Advertisements 1 MRM @ District 20 10000 960,000 4,800,000 6,804,000 13,500,000 2,000,000 2,400,000 11,162.79 Additional HR 80,000 400,000 567,000 1,125,000 200,000 Quarterly Review Meeting & Dissemination 4 150000 600,000 600,000 6,976.74 Chairperson 1 Program Director 1 Deputy PD 1 Human Resource Manger 1 Finance Manager 1 MIS Manager 1 Office Assistant 1 - District Manager M & E Officer DSU Data Entry Program Assistant Accounts Officer BHU PMU DSU RHCs THQ Overall Operational Costt 814,883.72 2,444,651.16 2,930,232.56 1,367,441.86 1,465,116.28 585,209.30 244,186.05 279,069.77 520,186.05 - 55,813.95 79,116.28 23,255.81 27,906.98 143 Call Response Center 8 100000 Printing 4 150000 800,000 600,000 Total 800,000 600,000 980,648,000 9,302.33 6,976.74 11,402,883.72 One Time Cost BHU 0 35000 Ambulances Furniture & Fixture for DSU IT Equipment (Laptop, PC, desktop, Printer, Fax) 250 0 22,500,000 5,250,000 1,425,000 - 8 50000 400,000 400,000 4,651.16 8 200000 1,600,000 1,600,000 18,604.65 USG Portable 150 500000 20 0 Equipment for RHCs Equipment for THQs/DHQs 8 800000 75,000,000 6,400,000 872,093.02 Repair & Renovation 75,000,000 6,400,000 40 500000 20,000,000 20,000,000 232,558.14 - - - 132,575,000 1,541,569.77 Basic Equipment for BHUs 150 150000 UPS with Battries 150 35000 F&F for BHUs 150 9500 Computers & Printer DSU/RSU RHCs THQ& DHQ 0 Total 22,500,000 5,250,000 1,425,000 - 261,627.91 61,046.51 16,569.77 - 74,418.60 - Annual Cost 980,648,000 Two Years Cost 1,961,296,000 One Time Cost 132,575,000 Total (Rs) Total $ 2,093,871,000 23,793,989 144 Budget Requirement under Head A-01299 Others (Stipend of LHVs/Ayas/Ambulance Drivers & Guards for the Financial Year 2015-16 Sr. No. Cadre # of Health Facilities 1 Nursing Staff (for DHQ Nutrition) 2 Budget Requirement in Rs. Strength Net Pay Period 34 DHQ +2 Teaching hospital 72 32000 12 27648000 WMO 292 RHCs 292 58000 12 203232000 3 Computer Operator PMU 2 27000 12 648000 4 LHVs (CHARM) 700 BHUs 1400 19000 12 319,200,000 5 Aya (CHARM) 700 BHUs 1400 10000 12 168,000,000 6 Ambulance drivers (CHARM) 466 11000 12 61,512,000 7 Gaurds (CHARM) 1400 10000 12 168,000,000 Total Fixed Salary 600,000 700 BHUs BPS 5032 948,240,000.00 145 Summary for Budget Requirement of Salary of Nutrition Program Staff working in Scales for the period July-2015 to June 2016 during the financial year 2015-16 SPHA Comp Allow A04115 Social Securit y 30% A-01970 Adhoc Relief Allow. 15% 20% Adhoc Relief Allowanc e (2012) Total 203,500 56,000 0 72,000 61,060 91,200 1,496,36 0 85,484 284,900 78,400 0 100,800 85,484 132,720 2,125,14 4 146,544 488,400 134,400 0 172,800 146,544 223,920 ###### Sr. No . Particular s A01101 Basic Pay A0110 5 Qualif. Pay Persona l Pay A01106 Pay of Contract Staff A01156 Pay of Contrac t Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA A01224 Entertainmen t Allow. A01217 Medical Allow A01964 SAA (2010) 1 Staff Salary July to Nov-15 250,000 0 0 456,000 0 95,540 100,000 30,000 20,000 0 61,060 2 Staff Salary Dec to June-16 350,000 0 0 663,600 0 133,756 140,000 42,000 28,000 0 Total Budget Requirement for 2015-16 600,000 0 0 1,119,600 0 229,296 240,000 72,000 48,000 0 146 Budget Requirement of Salary for the staff of Nutrition Program Punjab for the period Dec-15 to June-2016 Sr. No. Particulars BPS A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA Entertainment Allow A01217 Medical Allow SAA (2010) SPHA 4448 14825 11200 4448 14825 11200 Comp Allow Adhoc Relief Allow. 15% Adhoc Relief Allow. 20% Total 4448 0 105730 0 4448 0 105730 Social Security 30% 01 Posts of BPS-18 1 Program Manager Nutrition 19 Total 50000 50000 0 0 0 0 5809 5000 6000 4000 5809 5000 6000 4000 0 0 03 Posts of BPS-17 1 Nutrition Officer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 2 Software Engineer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 3 Statestical Officer 17 31600 4433 5000 2588 8625 4800 2588 6320 65954 Total Total PMU Salary for one Month Budget for Dec-15 to June-16 0 0 0 94800 0 13299 15000 0 0 0 7764 25875 0 0 14400 7764 18960 197862 50,000 0 0 94,800 0 19,108 20,000 6,000 4,000 0 12,212 40,700 11,200 0 14,400 12,212 18,960 303,592 350,000 0 0 663,600 0 133,756 140,000 42,000 28,000 0 85,484 284,900 78,400 0 100,800 85,484 132,720 2,125,144 147 Budget Requirement of Salary for the staff of Nutrition Program Punjab for the period July-15 to Nov-15 Sr. No. Particulars BPS A01101 Basic Pay A01105 Qualif. Pay Personal Pay A01106 Pay of Contract Staff A01156 Pay of Contract Staff A01202 House Rent Allow. A01203 Conv Allow. A01236 Deput. Allow. A01252 NPA Entertainment Allow A01217 Medical Allow SAA (2010) SPHA 4448 14825 11200 4448 14825 11200 Comp Allow Adhoc Relief Allow. 15% Adhoc Relief Allow. 20% Total 4448 0 105730 0 4448 0 105730 Social Security 30% 01 Posts of BPS-18 1 Program Manager Nutrition 18 Total 50000 50000 0 0 0 0 5809 5000 6000 4000 5809 5000 6000 4000 0 0 03 Posts of BPS-17 1 Nutrition Officer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 2 Software Engineer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 3 Statestical Officer 17 30400 4433 5000 2588 8625 4800 2588 6080 64514 Total 0 0 0 91200 0 13299 15000 0 0 0 7764 25875 0 0 14400 7764 18240 193542 Total PMU Salary for one Month 50,000 0 0 91,200 0 19,108 20,000 6,000 4,000 0 12,212 40,700 11,200 0 14,400 12,212 18,240 299,272 Budget for July 15 to Nov15 250,000 0 0 456,000 0 95,540 100,000 30,000 20,000 0 61,060 203,500 56,000 0 72,000 61,060 91,200 1,496,360 148 Cost Sheet of Nutrition Budget for the Financial Year 2015-16 Total children age 6 to 59 month 14 % MICs 2010-11 # of target Children SAM 30 % + 2% relapse & incidence rate ( 4% of Total target population) 16 16981 5298 21192460 30323 6822779 56856 341139 56856 7650 14 14563 4544 18174374 29720 6687000 55725 334350 55725 7498 91630 21 19242 6004 24014390 26180 5890500 49088 294525 49088 279580 20 55916 17446 69783168 79880 17973000 149775 898650 149775 19.7 15607 4869 19477947 22636 5093037 42442 254652 42442 5683 19 55833 17420 69680083 83960 18891000 157425 944550 157425 30698 113190 19 21506 6710 26839613 32340 7276500 60638 363825 60638 11824 155330 19 29513 9208 36831850 44380 9985500 83213 499275 83213 16226 250530 17 42590 13288 53152445 71580 16105500 134213 805275 134213 684075 95771 26 24900 7769 31075612 27363 6156675 51306 307834 742500 103950 13.7 14241 4443 17772955 29700 6682500 55688 334125 2566000 1283000 179620 17 30535 9527 38108179 51320 11547000 96225 Gujranwala 4404000 1321200 184968 13 24046 7502 30009208 52848 11890800 14 Sargodha 3189000 956700 133938 12 16073 5015 20058555 38268 15 Rawalpindi 4321000 1296300 181482 15 27222 8493 33973430 16 Faisalabad 6822000 2046600 286524 14 40113 12515 17 Bhawal Pur 3217000 965100 135114 14 18916 18 Sahiwal 2242000 672600 94164 16 15066 19 Attock 1562000 468600 65604 13 20 Chiniot 1156000 346800 48552 21 Gujrat 2509000 752700 22 Hafizabad 1024000 23 Jhang 24 S.No Districts Total population of districts 50%Target Population 1 Narowal 1516173 758086.5 106132 2 Layyah 1486000 743000 104020 3 Mianwali 1309000 654500 4 Multan 3994000 1997000 5 Khushab 1131786 565893 79225 6 Rahimyar Khan 4198000 2099000 293860 7 Pakpattan 1617000 808500 8 D. G. Khan 2219000 1109500 9 Muzaffargarh 3579000 1789500 10 Bhakkar 1368150 11 Rajanpur 1485000 12 Bhawal Nagar 13 # children age 6 month to 2 years Cost per Multinutrient supplementation for 6 month to 2 years # children age 2 to 5 years Cost for tab. Mebandazole SC Cost (F 75 & F 100) Cost for Anthropometry Equipment Total Cost for Supplies 12240065 7107061 100000 500000 48303503 11996478 6965625 100000 500000 44757827 6573 10516506 6135938 100000 500000 47451859 20055 32087796 18721875 100000 500000 140064489 9092769 5305247 100000 500000 39823651 49116600 19678125 100000 500000 158910358 18918900 7579688 100000 500000 61578525 25962300 10401563 100000 500000 84280487 26171 41874300 16776563 100000 500000 129314082 51306 10005 16007355 6413203 100000 500000 60560679 55688 10859 17374500 6960938 100000 500000 49725018 577350 96225 18764 30022200 12028125 100000 500000 92882854 99090 594540 99090 19323 30916080 12386250 500000 86296878 8610300 71753 430515 71753 13992 22386780 8969063 500000 60955212 51852 11666700 97223 583335 97223 18958 30333420 12152813 500000 89209698 50061473 81864 18419400 153495 920970 153495 29932 47890440 19186875 500000 136979158 5902 23607118 38604 8685900 72383 434295 72383 14115 22583340 9047813 500000 64858466 4701 18802668 26904 6053400 50445 302670 50445 9837 15738840 6305625 500000 47703203 8529 2661 10643593 18744 4217400 35145 210870 35145 6853 10965240 4393125 500000 30930228 14 6797 2121 8483005 13872 3121200 26010 156060 26010 5072 8115120 3251250 500000 23626635 105378 9 9484 2959 11836057 30108 6774300 56453 338715 56453 11008 17613180 7056563 500000 44118814 307200 43008 14 6021 1879 7514358 12288 2764800 23040 138240 23040 4493 7188480 2880000 500000 20985878 2333331 699999.3 98000 14 13720 4281 17122543 28000 6299994 52500 315000 52500 10237 16379984 6562493 500000 47180013 Jhelum 1134000 340200 47628 13 6192 1932 7727167 13608 3061800 25515 153090 25515 4975 7960680 3189375 500000 22592112 25 Kasur 3016000 904800 126672 21 26601 8300 33198198 36192 8143200 67860 407160 67860 13233 21172320 8482500 500000 71903378 26 Khanewal 2585000 775500 108570 21 22800 7114 28454026 31020 6979500 58163 348975 58163 11342 18146700 7270313 500000 61699513 27 Lodhran 1504000 451200 63168 19 12002 3745 14978396 18048 4060800 33840 203040 33840 6599 10558080 4230000 500000 34530316 28 M.B. Din 1523583 457074.9 63990 9 5759 1797 7187411 18283 4113674 34281 205684 34281 6685 10695553 4285077 500000 26987399 29 Chakwal 1435872 358968 50256 11 5528 1725 6899078 14359 3230712 26923 161536 26923 5250 8399851 3365325 500000 22556502 30 Nankana Sahib 1230000 307500 43050 14 6027 1880 7521696 12300 2767500 23063 138375 23063 4497 7195500 2882813 500000 21005884 31 Okara 2783000 556600 77924 22 17143 5349 21394813 22264 5009400 41745 250470 41745 8140 13024440 5218125 500000 45397248 32 Sheikhupura 2888000 577600 80864 13 10512 3280 13119375 23104 5198400 43320 259920 43320 8447 13515840 5415000 500000 38008535 33 T.T. Singh 1967000 393400 55076 16 8812 2749 10997576 15736 3540600 29505 177030 29505 5753 9205560 3688125 500000 28108891 34 Vehari 2671000 534200 74788 23 17201 5367 21467148 21368 4807800 40065 240390 40065 7813 12500280 5008125 500000 44523743 35 Sialkot 3435000 687000 96180 12 11542 3601 14403917 27480 6183000 51525 309150 51525 10047 16075800 6440625 500000 43912492 36 Lahore 8650000 1730000 242200 14 33908 10579 42317184 69200 15570000 129750 778500 129750 25301 40482000 16218750 500000 115866434 ####### ####### ###### 711443 221970 2335680 14014079 2335680 887,881,068 1245696 280,281,570 Total PLW7.5 % 13 % MAM PLW + 1.5 % Relapse & Incidence rate Cost for Tab.Iron Folic Acid Cost per SAM Child 433,908 Cost per PLW 694253276 291,959,969 ######## 18,000,000 2,187,589,962 Potassium Iodate for Salt Iodization 2,187,589,962 149 Program Reform Milestones including Disbursement Linked Indicators (DLIs) developed by WB/DFID Reform Area Component 1: Improving health service delivery i) Integrated management of MNCH and LHW Programs 2013-14 Essential Health Service Package at primary level defined, and approved 2014-15 EPHS for secondary care finalized and approved 2015-16 Plan developed for strengthening secondary care hospital developed Minimum Services Delivery Standards (MSDS) revised considering primary level EHSP and implementation started in all districts Assessment of MSDS in all districts of Punjab completed and more than 70% of the RMNCH and nutrition related quality standards met Punjab has operationalized the integrated management of three community based programs (Lady Health Workers, Maternal, Neonatal, and Child Health, and Nutrition programs), and approved the PC-1s for: (a) the integrated management for reproductive health, primary health care, and nutrition; (b) Lady Health Workers Program; and (c) Maternal, Neonatal, and Child Health. Punjab has attained: (i) at least 35% in the use of modern contraceptive methods; and (ii) at least 70% skilled birth attendance. MNCH Implementation of 24/7 comprehensive RMNCH program rolled out in 20 focus districts 17 of DHQ and 30 THQ hospitals providing full package of 24/7 comprehensive EmONC services 34 DHQ and >55 THQ hospitals providing complete package of 24/7 comprehensive EmONC services and >15 RHCs meeting 24/7 C-section signal function >200 RHCs providing complete package of basic EmONC services and >150 BHUs meeting 24/7 Assisted delivery signal function LHWP At least 15,000 LHWs in the priority districts trained on a) family planning and b) nutrition. 2016-17 EPHS for tertiary care finalized and approved Training of LHWs in delivering routine immunization started in 4 districts completed 36 DHQ and >65 THQ hospitals providing complete package of 24/7 comprehensive EmONC services along with >30 RHCs meeting C-section signal function >250 RHCs providing complete package of basic EmONC services and >300 BHUs meeting 24/7 Assisted delivery signal function Evaluation of “LHWs involved in routine immunization” initiated 150 ii) Introduction of Nutrition Services Comprehensive Nutrition interventions implementation initiated in 12 priority districts with materials and funding available and training completed IYCF training module for community workers developed and rolled out in 36 districts In the 12 priority districts, at least 20% of children with SAM registered for treatment In the 12 priority districts, at least 40% of children with SAM registered for treatment 15 Stabilization centers and 200 Outpatient Therapeutic Program centers made functional 35 Stabilization centers and >600 Outpatient Therapeutic Program centers made functional At least 20% of households receive a core package of nutrition services in 12 districts Review of regulatory monitoring system for food fortification carried out and new system agreed At least 80% of community-based workers in the 12 high-priority districts trained on nutrition At least 60% of children identified with severe acute malnutrition in all 12 high priority districts have been registered for treatment. At least 75% of households receive a core package of nutrition services in 12 districts More than 80% of LHWs have knowledge and skills scores (using case studies scenario) of above 80% 151 DFID’s Disbursement Linked Indicators for Punjab (Aligned with HSS, Operational Plan and PC-1s) The disbursement linked indicators for Provincial Health and Nutrition Programme – Punjab, for the period 2013-17 . 2013-14 AREA Service Delivery Weightage 45% 2014-15** 20015-16** 2016-17** Punjab: £14 million Punjab: £25 million Punjab: £27 million Punjab: £24 million - Approval of 3 year provincial PC-1 of Integrated RMNCH and nutrition programme with commitment of the provincial government to invest development funds in this programme; - Results based contracts defined (considering EHSP/ MHSP and including RMNCH and nutrition interventions at primary health facilities and community level) and signed for 14 districts in Punjab; - Assessment of MSDS in all districts of Punjab completed and more than 80% of the RMNCH and nutrition related quality standards met; - Third Party evaluation of the management models for service delivery and implementation of EPHS completed and following results achieved in Punjab. - Essential/ Minimum Health Service Package (E/MHSP) at primary level defined, costed and approved in Punjab; - Piloting of implementation of Infection Control Management Protocols started in at least one district in the province. Disbursement linked to the DLI for FY 2013/14: £6.3 million - Minimum Services Delivery Standards (MSDS) revised considering primary level EHSP/MHSP and implementation started in all districts Punjab; - 15 Stabilisation centres (with availability of RUTF - Readyto-use therapeutic food) and 200 Outpatient Therapeutic Programme (OTP) centres made functional with government financing in Punjab; - 35 Stabilisation centres (with availability of RUTF) and >600 Outpatient Therapeutic Programme (OTP) centres made functional with government financing in Punjab; - 60% of DHQ and THQ hospitals providing COMPLETE PACKAGE of 24/7 comprehensive EmONC services in Punjab; - Successful implementation of Infection Control Protocols in >20 districts of the Punjab. o o o o o o Modern methods CPR increased to 33% Exclusive breast feeding rate increased to >40% Immunisation coverage (fully) in the province increased to >75% >60% of identified children treated for Severe Acute Malnutrition (SAM) in last month/quarter >80% of DHQ and THQ hospitals providing COMPLETE PACKAGE of 24/7 comprehensive EmONC services Skilled Birth Attendance (SBA) increased to >70% Disbursement 152 linked to the DLI for FY 2015/16:£12.15 million Disbursement linked to the DLI for FY 2016/17:£10.8 million - Minimum two meetings of the steering committee/ task force of HSS implementation held during 2013-14 in Punjab - Minimum two meetings of the steering committee/ task force of HSS implementation held during 2014-15 in Punjab; - Minimum two meetings of the steering committee/ task force of HSS implementation held during 201516 in Punjab; - Review of restructuring of DGHS office completed in Punjab; - Restructuring of DGHS office completed in Punjab; - 40% of DHQ and THQ hospitals providing COMPLETE PACKAGE of 24/7 comprehensive EmONC services in Punjab. Disbursement linked to the DLI for FY 2014/15: £11.25 million Stewardship/ Governance Weightage 15% - Approval of HSS, Operational plan and notification of governance mechanism for its implementation oversight in the province; - Approval of PC-1 for continuation of Policy and Strategic Planning Unit (PSPU) in Punjab; - Business plan for Punjab Health Care Commission (PHCC) approved by the board in Punjab. Disbursement linked to the DLI for FY 2013/14: £2.1 million Human Resource Weightage 5% - In case of successful results, emanagement interventions scaled up in all districts of Punjab. Disbursement linked to the DLI for FY 2014/15:£3.75 million - Training of another batch of >1000 Community Midwives (CMWs) started in 2012 in Punjab. - Training of another batch of >1000 and 200 Community Midwives (CMWs) started in 2013 in Punjab; Disbursement linked to the DLI - Human Resource Strategy and Inservice training strategy - Implementation of plan to strengthen consumer complaints system started by PHCC in Punjab. Disbursement linked to the DLI for FY 2015/16:£4.05 million - Training of another batch of >1000 and 200 Community Midwives (CMWs) started in 2014 in Punjab respectively; - All LHWs trained on family planning - >90% of the management positions at provincial level and that of EDO(H) filled with qualified/ competent personals in Punjab. Disbursement linked to the DLI for FY 2016/17: £3.6 million - Training of another batch of >1000 and 200 Community Midwives (CMWs) started in 2015 in Punjab; - More than 80% of LHWs have knowledge and skills scores (using case 153 for FY 2013/14: £0.7 million developed and Human Resource Cell established in DoH Punjab; - All LHWs trained on IYCF in both provinces and training of LHWs in delivering routine immunisation started in 4 districts of Punjab. and trained LHWs immunising children and women in their catchment areas. Disbursement linked to the DLI for FY 2015/16:£1.35 million studies scenario) of above 80%; - Results of evaluation of “LHWs involved in routine immunisation” available. Disbursement linked to the DLI for FY 2016/17:£1.2 million Disbursement linked to the DLI for FY 2014/15:£1.25 million Information Weightage 10% - Development of health sector M&E plan of action started in Punjab. Disbursement linked to the DLI for FY 2013/14: £1.4 million - Health sector M&E plan of action including disease surveillance available and accordingly PC1 approved in Punjab; - Second round of Annual Health Facility Assessment completed. Disbursement linked to the DLI for FY 2014/15:£2.5 million Financing Weightage 15% - Development of fiduciary risks mitigation plan in Punjab; - Written commitment for inclusion of HSS’s policy objectives in the next year MTBF cycle in Punjab. Disbursement linked - Minimum 70% increase in development health expenditure (mainly for RMNCH interventions and excluding federal grants) at provincial level and 15% increase in Districts nonsalary - M&E unit in DGHS office fully functional and Disease surveillance system operationalized in selected districts in Punjab; - Third round of Annual Health Facility Assessment completed. - Fourth round of Annual Health Facility Assessment completed. Disbursement linked to the DLI for FY 2016/17:£2.4 million Disbursement linked to the DLI for FY 2015/16:£2.7million - Further 20% increase in development health expenditure (mainly for RMNCH interventions and excluding federal grants) at provincial level and 20% additional increase in non- - tbd - considering expected shift of provincial RMNCH and nutrition expenditures from provincial budgets to district current budgets; - Reassessment of fiduciary risk showing improvement Punjab; 154 to the DLI for FY 2013/14: £2.1 million expenditure in Punjab; - Successful implementation of Fiduciary risk mitigation plan in Punjab; - Options for health financing including testing of Vouchers Scheme explored. Medical Products Weightage 10% - Procurement cell in DoH -Approval of PC-1 and progress towards strengthening of the cell; and standard operating procedures (SOPs) for procurement developed in Punjab. Disbursement linked to the DLI for FY 2013/14: £1.4 million salary district expenditure in Punjab; - Successful implementation of Fiduciary risk mitigation plan in Punjab; Disbursement linked to the DLI for FY 2015/16:£4.05 million - Procurement cell ensuring implementation of PPRA rules and regulations in Punjab; - Procurement of contraceptive commodities for health facilities and community workers completed using provincial government resources initiated in Punjab; - More than 70% of LHWs having no stock out of Zinc, ORS, Iron/ folic acid tablets and deworming tab/syp and contraceptives over last one month in Punjab. Disbursement linked to the DLI for FY 2014/15: £2.5 million Disbursement linked to the DLI for FY 2016/17:£3.6 million - Implementation of Voucher Scheme started. Disbursement linked to the DLI for FY 2014/15:£3.75 million - More than 60% of health facilities having no stock out of 3 contraceptive methods in Punjab; - Intervention of Voucher Scheme evaluated. - More than 80% of LHWs having no stock out of Zinc, ORS, Iron/ folic acid tablets and deworming tab/syp and contraceptives over last one month in Punjab; - Government procured contraceptive commodities available in all districts of Punjab; - More than 85% of LHWs having no stock out of Zinc, ORS, Iron/ folic acid tablets and deworming tab/syp and contraceptives over last one month in Punjab. Disbursement linked to the DLI for FY 2016/17:£2.4 million - Misoprostol available in all RHCs in Punjab. Disbursement linked to the DLI for FY 2015/16:£2.7million *DLIs in bold are pre requisite for the disbursement ** DLIs to be reassessed and updated following reviews. *** Reviews to be held bi-annually or annually and will be agreed after discussion **** Funds disbursed on the achievement of DLIs will only be used for delivery of EHSP/ RMNCH (including nutrition) interventions through the development budget at provincial level or districts grants for the implementation of EHSP. 155