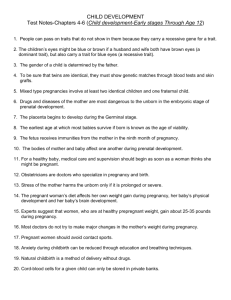
Charles and Baby Florence (last 2 action points)
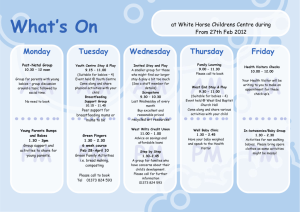
advertisement

Charles and Baby Florence Action Point Prepare a teaching plan for the coffee group that outlines The weeks during pregnancy when a first time mother will start to feel her baby move for the first time By the end of the fourth month and beginning of the fifth month the first time mother will start to feel her baby move. The difference in weeks when movements are felt for a mother in a second or subsequent pregnancy Some women who have had previous children may feel their baby’s movements during the fourth month The correct term for feeling a baby move, is it in fact lightening? These first fetal movements are called quickening and are often described as flutters. It may be difficult to determine whether this feeling is gas or your baby’s movements. Warning signs of pregnancy, what would cause a pregnant woman to seek help urgently from her LMC? Signs of pregnancy Pregnancy can be exciting or daunting, depending on the circumstances. Do you suspect you're pregnant? Below are some of the tell-tale first signs of pregnancy. Most women mark the first missed period as the first sign of pregnancy, but a missed period can be caused by a number of factors. A large change in diet, exercise or stress level can also contribute to a missed period. Some women experience spotting about two weeks after the first day of the previous period as the first sign of pregnancy. This spotting is caused when the fertilized egg implants in the uterus and is usually very light. Mood Swings caused by hormonal surges early in pregnancy can be more severe than those experienced during PMS. Often this is the first symptom of pregnancy noticed by family members! Breast tenderness and enlargement, caused by the breast preparing for breastfeeding is especially common during very early pregnancy, but often disappears after a few weeks. Darkening areolas, or the area around your nipples, occurs soon after conception and may persist throughout the pregnancy. Fatigue is an early sign of pregnancy, but also a sign of many other conditions. Nausea and vomiting, sometimes referred to as morning sickness, ranging from queasiness to severe vomiting that can manifest just in the morning (when hormone concentrations are highest) or all day. Changes in appetite and food cravings often plague the newly pregnant woman and can occur early in the pregnancy right through delivery. Pregnancy symptoms you should not ignore Note that some of these symptoms may be more or less urgent depending on how far along you are in your pregnancy and on your particular situation or health history. Ask your practitioner to review with you which signs warrant an urgent call or immediate emergency medical care as your pregnancy progresses. Your baby is moving or kicking less than usual (once he begins moving regularly). Ask your caregiver whether you should monitor your baby's activity by doing daily "kick counts." She can give you specific instructions on how to count and when to call. Severe or persistent abdominal pain or tenderness. Vaginal bleeding or spotting. An increase in vaginal discharge or a change in the type of discharge – that is, if it becomes watery, mucousy, or bloody (even if it's only pink or blood-tinged). Note: After 37 weeks, an increase in mucus discharge is normal and may indicate that you'll be going into labor soon. Pelvic pressure (a feeling that your baby is pushing down), lower back pain (especially if it's a new problem for you), menstrual-like cramping or abdominal pain, or more than four contractions in an hour (even if they don't hurt) before 37 weeks. Painful or burning urination, or little or no urination. Severe or persistent vomiting, or any vomiting accompanied by pain or fever. Chills or fever of 100 degrees Fahrenheit or higher. Visual disturbances such as double vision, blurring, dimming, flashing lights, or "floaters" (spots in your field of vision). Persistent or severe headache, or any headache accompanied by blurred vision, slurred speech, or numbness. Any swelling in your face or puffiness around your eyes, anything more than a little swelling in your hands, severe and sudden swelling of your feet or ankles, or a rapid weight gain (more than 4 pounds in a week). A persistent or severe leg cramp or calf pain that doesn't ease up when you flex your ankle and point your toes toward your nose or when you walk around, or one leg being significantly more swollen than the other. Trauma to the abdomen. Fainting, frequent dizziness, a rapid heartbeat, or heart palpitations. Difficulty breathing, coughing up blood, or chest pain. Severe constipation accompanied by abdominal pain or severe diarrhea that lasts more than 24 hours. Persistent intense itching of your torso, arms, legs, palms, or soles, or a feeling of itchiness all over your body. Flu exposure or symptoms. Both flu and H1N1 (swine) flu are very risky for pregnant women. So let your caregiver know right away if you've been in close contact with someone who has the flu or if you have any flu symptoms, which may include fever, sore throat, cough, runny or stuffy nose, fatigue, and body aches and chills. Symptoms may occasionally include vomiting or diarrhea. Seek immediate emergency medical care if you're experiencing shortness of breath or difficulty breathing, chest or abdominal pain, sudden dizziness or confusion, severe or persistent vomiting, decreased fetal movement, or if you have a high fever despite taking acetaminophen. Exposure to a communicable disease like chicken pox or rubella if you're not immune or are showing signs of infection. Call your caregiver – don't show up at the office without phoning first. Depression or severe anxiety. If you are feeling a profound sense of sadness or hopelessness, having panic attacks, are unable to handle your daily responsibilities, or are having thoughts of harming yourself, seek help immediately. Any other health problem that you'd ordinarily call your practitioner about, even if it's not related to your pregnancy (like worsening asthma or a cold that gets worse rather than better). Use this opportunity to educate the coffee group about contraception options for breast feeding women One participant says “I’m so pleased I don’t have to worry about contraception cause I can’t get pregnant while I’m breastfeeding”. Outline your response Breastfeeding and birth control For the nursing mother who wants to space her pregnancies, there are many birth control options to choose from. Each method offers advantages and disadvantages. As long as the nursing mother is exclusively breastfeeding, (nursing frequently day and night with no supplemental feedings), the baby is younger than 6 months of age, and the mother has not started having periods, she is more than 98% protected against pregnancy. This period of exclusive nursing means not only no supplemental feedings of water or formula, but also little or no pacifier use. All of the baby's sucking needs are met at the breast, which means demand feedings around the clock. As long as the mother has had no vaginal bleeding after 56 days postpartum, and the baby receives no supplemental feeds, she has only about a 2% chance of becoming pregnant (this compares to the combined birth control pill, which is about 98%-99% effective if taken every day without missing a dose). It is important to understand that as soon as there is a decline in breastfeeding, due to the baby eating supplemental feedings or nursing less often, the contraceptive protection decreases, and other methods should be considered. Fertility is most effectively suppressed when the baby goes no longer than four hours during the day and six hours at night between feedings. The pattern of breastfeeding is a key factor, but the mother's own body chemistry also has an influence. Some mothers nurse without supplements and still start having periods within the first few months of nursing. Others whose babies sleep through the night or have supplemental feedings will not have a period for twelve months or longer. Some women go as long as two years or more without menstruating. After the initial flow of lochia (the bleeding experienced for two to four weeks after birth) has stopped, nursing mothers will usually experience no vaginal bleeding for several months. Often, the first period occurs without ovulation. Many women refer to this as a "warning" period, and take it as a sign that they are fertile from that point on. Often light bleeding or spotting is the first indication of the return of fertility. Any bleeding or spotting that lasts more than a couple of days should be considered a sign that the mother is fertile again. It is not unusual for a mother to have irregular periods during the time she is nursing. Some (but not all) mothers notice a slight decrease in their milk supply during their periods, but after a few days the supply will increase. It is important to think about birth control options well before the time a mother becomes fertile again. What follows is a list of family planning options as they relate to breastfeeding women. It is important to emphasize that hormonal methods containing estrogen should be avoided whenever possible. Changes in the mother's body during lactation may include vaginal dryness due to low levels of estrogen. Intercourse may be more comfortable if a water-based lubricant such as K-Y jelly is used. The release of oxytocin during orgasm may cause the mother's milk to leak or spray and surprise both partners. Feeding the baby or expressing some milk before love-making, applying pressure as the milk lets down, and keeping a towel handy to catch the leaks may be helpful. The first choice of birth control for nursing mothers is non-hormonal methods. This includes condom use, which has the advantages of being readily available, and having no effect on breastfeeding. Condoms can be very effective if used correctly. Condoms offer some protection against STDS (sexually transmitted diseases) and have no risks to the mother or child, but can be irritating to vaginal tissue and may require additional lubrication. Diaphragms also have no effect on breastfeeding, and can be very effective if used correctly. Their effectiveness depends on use with a spermicide, and they must be re-fitted after the baby is born and the uterus has returned to its pre-pregnancy size. Spermicides have no effect on breastfeeding, and can be very effective if used according to instructions. They may be irritating to the vagina and to the male partner. Spermicides are not known to pass into the milk and affect the baby in any way. IUDs have no effect on breastfeeding, and are very effective. There is a possible risk of expulsion or uterine perforation if the device is not properly placed or is inserted before 6 weeks postpartum. Permanent methods such as vasectomy and tubal ligation have no effect on breastfeeding and are nearly 100% effective. These methods are considered irreversible, and should only be considered if no more children are desired. If these methods are considered, counseling is recommended for couples. Vasectomy is considered minor surgery with minimal side effects. Tubal ligation may involve short-term mother-infant separation, and has risks, as all surgery does. Anesthesia may pass into breastmilk and sedate the baby. As a general rule, tubal ligation has more risks for the mother and is considered more complicated surgery than vasectomy is for the father. The other non-hormonal method of birth control is natural family planning. This method involves learning the signs and symptoms of infertility, and may require extended periods of abstinence. It has no effect on breastfeeding, and can be very effective if used correctly. Because it may be difficult to interpret signs of fertility during breastfeeding, this method may require additional training in order to interpret the symptoms of fertility during lactation. If the nursing mother chooses to use a hormonal method of birth control, the second choice is progestin only methods, such as Norplant (implants), mini-pills, or injectables (Depo-Provera). All of these methods can be very effective, and may even increase milk volume. Although some of the progestin hormone may enter the breastmilk, there is no evidence of adverse effects from the small amount of hormone that passes into the milk. It is recommended that the use of progestin-only hormones be delayed for at least six weeks post-partum due to the possibility of the hormones interfering with the early establishment of lactation. The third and last choice of birth control for nursing mothers is methods which contain estrogen, such as the standard combined oral contraceptives. These methods are very effective, but often decrease milk supply, and some of the hormone may pass into the mother's milk. Although there is no evidence of a direct negative effect on the babies of mothers taking the combined pill, there is strong evidence that in many women, estrogen can lead to a decrease in milk supply and early weaning. If the other methods of birth control can't be avoided, and the combined pill is the only option, then breastfeeding can and should be continued, since it offers many health and nutritional benefits which are important for the nursing infant or toddler. If the mother chooses to use this method, the baby's weight should be monitored carefully so that adequate intake is ensured. For many mothers, a slight decrease in milk output is insignificant, and in any case, the benefits of breastfeeding far outweigh the disadvantages. You can tell that one or more of the participants of the coffee groups are smokers and you become concerned when you hear a discussion that implies smoking is a good way to ensure you have a small baby that will be easier to deliver. Action Point Prepare a teaching plan for the coffee group that covers the development of a foetus in utero and the effect smoking will have on the developing foetus. You decide it is relevant to include all lifestyle changes required pre-pregnancy to ensure women give themselves and their unborn babies the best development possible by caring about their health. Smoking during pregnancy Smoking during pregnancy reduces the growth and health of babies and increases the risks of a number of complications and illnesses for both the mother and baby. In New Zealand in 2006, around 22 percent of pregnant women reported they smoked while pregnant. Quitting smoking before or during pregnancy, and avoiding exposure to second-hand smoke, will have a positive impact on the health of both the mother and the unborn baby. It will also reduce the likelihood of related health problems for the child after birth. Babies born to women who smoke during pregnancy have a greater chance of premature birth, low birth weight, stillbirth, and infant mortality. Smoking during pregnancy can also affect the development of babies' lungs, which increases the risk for many health problems. Nicotine and other chemicals in tobacco smoke are passed onto the baby through the placenta. Nicotine causes the blood vessels to constrict which decreases the amount of oxygen going to the unborn baby and is an important contributor to low birth weight. Mothers who smoke also pass nicotine onto their babies through their breast milk. Smoking during any stage of pregnancy increases the risk of premature birth. Australian research shows that in 2003, for babies of mothers who smoked, the likelihood of pre-term birth was 60 percent higher than in babies of mothers who did not smoke. Low birth weight is a leading cause of infant death and an important risk factor for a number of health problems and complications in infancy and childhood. The Australian research also showed that babies of mothers who smoked were twice as likely to be of low birth weight than babies of mothers who did not smoke. On average, babies born to smoking mothers weigh about 200 grams less than those born to non-smoking mothers. Mothers who smoke are 50 percent more likely to have a stillborn baby than mothers who do not smoke. This risk is believed to be influenced by smoking-induced placental complications combined with smoking-induced abnormal foetal growth. In addition, babies born to mothers who smoke before and after birth are three times more likely to die from Sudden Infant Death Syndrome (SIDS). It has been estimated that around 50 New Zealand babies die every year from SIDS as a result of exposure to second-hand smoke, and emerging evidence suggests that smoking during pregnancy is an even stronger risk factor for SIDS than exposure to second-hand smoke. Some of the long-term health effects on the development of children born to smoking mothers include: Allergies – fourfold increased risk of having allergic skin diseases by 18 months of age. Higher blood pressure in childhood. A much greater risk of childhood respiratory disorders such as asthma and wheezing. Increased risk of obesity in childhood and into adolescence. According to a recent study, Australian children of mothers who smoked while pregnant are approximately 42 percent more likely to be obese by their early teens than children of mothers who did not smoke while pregnant. In addition to avoiding smoking while pregnant it is also important for pregnant women to avoid exposure to second-hand smoke as this can harm unborn babies. Maternal exposure to second-hand smoke may result in premature birth and lower birth weight for their babies. There is emerging evidence that the risk of some childhood cancers increases as a result of the mother's exposure to second-hand smoke during pregnancy. Other studies suggest that children of fathers who smoke have an increased risk of developing childhood cancers, possibly as a result of damage to the father's sperm. Alcohol Use When you drink alcohol your baby is drinking it too. Therefore, you should avoid all forms of alcohol when you are pregnant. This includes beer, wine and hard liquor. When a pregnant woman drinks alcohol, it quickly reaches the baby through the blood stream. Drinking alcohol during pregnancy may result in Fetal Alcohol Syndrome, lower birth weight, physical deformities, mental retardation, and motor development complications. There is no data to support a safe level of alcohol consumption during pregnancy. Therefore, medical experts recommend avoiding alcohol completely during your pregnancy. Exercise during pregnancy If you have been following a regular exercise program prior to your pregnancy, you should be able to maintain that program to some degree throughout your pregnancy. Exercise does not increase the risk for miscarriage in a normal low risk pregnancy. If you are just starting an exercise program as a way of improving your health during your pregnancy, you should start very slowly and be careful not to over exert yourself. Consider a prenatal yoga class that is specifically designed for pregnant women. Shop Yoga for home Listen to your body. Your body will naturally give you signals that it is time to reduce the level of exercise you are performing. Never exercise to the point of exhaustion or breathlessness. This is a sign that your baby and your body cannot get the oxygen supply they need. Wear comfortable exercise footwear that gives strong ankle and arch support. Take frequent breaks, and drink plenty of fluids during exercise. Avoid exercise in extremely hot weather. Avoid rocky terrain or unstable ground when running or cycling. Your joints are more lax in pregnancy, and ankle sprains and other injuries may occur. Contact sports should be avoided during pregnancy. Weight training should emphasize improving tone, especially in the upper body and abdominal area. Avoid lifting weights above your head and using weights that strain the lower back muscles. During the second and third trimesters, avoid exercise that involves lying flat on your back as this decreases blood flow to the uterus. Include relaxation and stretching before and after your exercise program. Eat a healthy diet that includes plenty of fruits, vegetables and complex carbohydrates. Eating Choose a variety of foods from each of the different food groups to make sure you're getting a good balance for your baby. Have a look at the table below Ask your health care professional about supplements if you are worried you are not getting what your baby needs from a particular food group Your health care professional will also recommend to take folic acid, if you are not already, for at least the first 12 weeks after conception Have three regular meals and two to three light snacks a day Include generous helpings of fruits and vegetables, wholegrain cereals and legumes to increase your dietary fibre intake. About 30 grams of dietary fibre a day is best Drink lots of water - at least six to eight glasses a day Include other drinks / liquids in your diet such as low-fat milk, fresh fruit juices and healthy soups Use healthier vegetable oils such as canola, olive and sunflower oil in your cooking Limit your intake of processed and preserved foods as they usually contain high levels of salt Reduce your caffeine intake – this means no more than three cups of coffee or tea a day Limit your intake of sweets, chips, cakes and biscuits as they contain lots of fats, oils, and sugar. These all provide extra calories but not much of the nutritional value that your baby needs. Also, over-indulging now means it will be harder to regain your pre-pregnancy figure afterwards, so try to resist dipping into the biscuit tin too often! Avoid alcohol totally. Your baby's growth certainly will not be helped by alcohol, so don't even go there! References http://www.americanpregnancy.org/duringpregnancy/firstfetalmovement.htm http://ezinearticles.com/?The-First-Warning-Signs-of-Pregnancy&id=33924 http://www.babycenter.com/signs-of-a-pregnancy-problem http://www.breastfeedingbasics.com/html/breastfeeding_and_birth_control.shtml http://www.moh.govt.nz/moh.nsf/indexmh/tobacco-warnings-factsheets-notonlyone http://www.americanpregnancy.org/pregnancyhealth/exerciseguidelines.html http://www.kariclub.co.nz/feeding_and_nutrition/pregnancy_nutrition/article/eating_well_in_preg nancy?gclid=CN-7xoH1lqsCFYEmpAodaQMJTA