ADHD Clinical Practice Guideline
advertisement

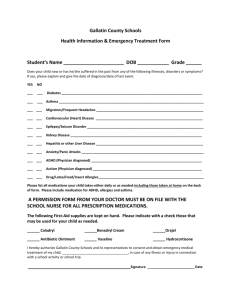
Clinical Practice Guideline for Attention-Deficit/Hyperactivity Disorder (ADHD) This guideline is intended for use primarily by practitioners working in primary care and other non-behavioral health settings. SUMMARY ADHD often goes undiagnosed; therefore, an evaluation for ADHD should be performed in patients 4 to 18 years of age who present in a health care setting with academic or behavior problems and who display inattention, hyperactivity, and/or impulsivity. In addition, there are many adults with symptoms of ADHD not diagnosed as children, prior to age 12, yet continue to struggle with inattention, hyperactivity, and/or impulsivity. These adults should also be evaluated for ADHD. When making an ADHD diagnosis, practitioners should ensure all criteria in the current Diagnostic and Statistical Manual of Mental Disorders (DSM) are met and all other causes are ruled out. Recommended Guidelines CHILDREN AND ADOLESCENTS Assessment and Diagnosis of Children and Adolescents The primary care physical health and/or behavioral health practitioner should initiate an evaluation for ADHD for any child four through 18 years of age who presents with academic or behavioral problems and symptoms of inattention, hyperactivity, or impulsivity. Information should be collected from the patient's parents/family, teachers, and other mental and physical health care professionals. 1. To make a diagnosis of ADHD, the primary care physical health and/or behavioral health clinician should determine diagnostic criteria have been met based on the current DSM: a. Making a diagnosis includes documenting that the child is impaired in more than one major setting (e.g., in school and at home). The primary care clinician should include reports from parents or guardians, teachers, and/or other school and mental health practitioners involved in the child’s care. b. The primary care clinician should also rule out any other possible causes of the noted symptoms. c. When evaluating a child for ADHD, the primary care clinician should assess whether other conditions are present coexisting with ADHD, including emotional or behavioral (e.g., anxiety, depressive, oppositional defiant, and conduct disorders), developmental (e.g., learning and language disorders or other neurodevelopmental disorders), and physical (e.g., tics, sleep apnea) conditions. 2. Socio-economic factors impacting the child and parents that may be contributing to and/or exacerbating symptoms for the child and should also be considered. If appropriate the child TCHP_ZZ80NR Effective 4/09/2015 Page 1 of 6 and/or parent may be screened with appropriate forms such as Adverse Childhood Experiences (ACES). 3. Prior to considering the use of psycho-stimulant medications all children and adolescents must be screened for cardiovascular risks1. 4. Adolescents with newly diagnosed ADHD should be assessed for substance abuse. When possible, substance abuse should be treated before initiating medication treatment for ADHD. 5. The primary care clinician should recognize ADHD as a chronic condition and, therefore, consider children and adolescents with ADHD as children and youth with special health care needs (CYSHN). Care for such children and youth should follow the principles of the chronic care model and the medical home. 6. If medications are utilized the primary care clinician should titrate doses of medication for ADHD to achieve maximum benefit with minimum adverse side effects. 7. It should be noted DSM criteria can be used in preschool-aged children (4-5 years of age), although the subtypes may not be valid. Treatment of Children and Adolescents Recommendations for treatment of children and youth with ADHD vary depending on the patient’s age. In demographic areas where evidence-based behavioral treatments are not available, the clinician needs to weigh the risks of starting medication at an early age against the harm of delaying diagnosis and treatment. The clinician should also consult additional resources about age appropriate evidence based treatment options including the education system and local behavioral health resources. 1. For preschool-aged children (4–5 years of age): a. The primary care clinician should prescribe evidence-based parent- and/or teacher-administered behavior therapy as the first line of treatment.2 b. Pharmacotherapy may be considered if the behavior interventions do not provide significant improvement and there is moderate-to-severe continuing disturbance in the child’s function. First choice to prescribe is methylphenidate. 2. For elementary school–aged children (6–11 years of age): a. The primary care clinician should prescribe evidence-based parent- and/or teacher-administered behavior therapy as the first line of treatment. The school environment, program, or placement is a part of any treatment plan.2 b. Pharmacotherapy may be considered if the behavior interventions do not provide significant improvement and there is moderate-to-severe continuing disturbance in the child’s function. The primary care clinician should prescribe US Food and Drug Administration (FDA) – approved medications for ADHD. The evidence is particularly strong for stimulant medications and sufficient, but less strong, for atomoxetine, extended-release guanfacine, and extended-release clonidine (in that order). TCHP_ZZ80NR Effective 4/09/2015 Page 2 of 6 3. For adolescents (12–18 years of age): a. The primary care clinician should prescribe evidence-based parent- and/or teacher-administered behavior therapy as the first line of treatment.2 The school environment, program, and/or placement is part of any treatment plan. b. Information should be collected from the patient's parents, teachers, and other mental and physical health care professionals. Most adolescents (12 to 18 years of age) have more than one teacher; practitioners should, attempt to get information from at least two teachers, and from other persons who interact with the adolescent (e.g., coaches, counselors).c. To monitor for misuse or diversion of stimulants, primary care clinics should consider using a controlled substances agreement and random urine drug screening in addition to regular follow-up visits. d. Pharmacotherapy may be considered if the behavior interventions do not provide significant improvement and there is moderate-to severe continuing disturbance in the child’s function. The primary care clinician should prescribe FDA – approved medications for ADHD with the assent of the adolescent. The evidence is particularly strong for stimulant medications and sufficient, but less strong, for atomoxetine, extended-release guanfacine, and extended-release clonidine (in that order). Non-stimulant medications for the treatment of ADHD may also be considered for older adolescents. ADULTS Assessment and Diagnosis of Adults Attention-deficit/hyperactivity disorder in childhood can persist into adulthood in at least 30 percent of patients, with 3 to 4 percent of adults meeting the DSM diagnostic criteria. Of the adults meeting criteria, 40 percent will be in the severe category for ADHD. In addition, up to 16 percent of adults will exhibit symptoms of attention-deficit hyperactivity disorder, yet will not meet the full DSM diagnostic criteria. Many adults with ADHD were not identified as children, nor do they have the memory of being diagnosed or treated prior to the age of 12. It is important to consider the adult’s current symptoms, whether or not they were identified as having the disorder as a child. 1. The clinical diagnosis of ADHD in adults should take a stepwise approach, including: a. Evaluating current (in the past six months) ADHD symptoms using rating scales with adult norms. b. Establishing a childhood history (before 12 years of age) of ADHD. Obtaining a developmental history helps to establish symptoms which occurred in childhood. . It may be helpful to try to obtain school records or report cards, and to speak with the TCHP_ZZ80NR Effective 4/09/2015 Page 3 of 6 patient's parents or other family members who interacted with the patient when he or she was a child. c. Evaluating functional impairment at home, work, and school, and in relationships. d. Obtaining a psychiatric history to rule out other psychiatric disorders or to establish the presence of comorbid disorders, including anxiety, mood, obsessive-compulsive, substance use, antisocial personality, borderline personality, learning disorders, and intellectual disability. e. Obtaining a family history for ADHD, tics, drug use, and criminal behavior. f. Performing a physical examination to eliminate medical or other physical causes. The examination should focus on thyroid and neurologic examination to rule out thyroid abnormalities and neurologic disorders (e.g., head injury, seizure disorder), and on possible contraindications of stimulant therapy (e.g., hypertension). Baseline weight and blood pressure should be recorded for comparison in future monitoring. Medical conditions include hearing impairment, thyroid disease, lead toxicity, hepatic disease, sleep apnea, and drug interactions should be considered. Certain substances, such as steroids, antihistamines, anticonvulsants, caffeine, and nicotine may have adverse effects impacting attentiveness and should be reviewed. g. Contraindications for stimulant use include hypertension, tachycardia, arrhythmia, psychosis, bipolar disorder, severe anorexia, Tourette’s disorder and other tic disorders. h. No specific laboratory or ancillary tests exist for confirmation of diagnosis, but some tests, such as thyroid studies, liver function tests, and lead levels may be helpful for ruling out comorbid or mimicking conditions. Treatment of Adults 1. Clinical guidelines recommend Cognitive Behavior Therapy (CBT) as an evidenced based treatment for adult ADHD. Treatment may be initiated by a behavioral health practitioner within the clinic or a referral should be made to an appropriately trained behavioral health specialist outside of the clinic. 2. Pharmacotherapy may be considered if the behavior interventions do not provide significant improvement and there is moderate-to-severe continuing disturbance in the person’s function. Adjunctive treatment with medication includes psycho-stimulants and the non-stimulant atomoxetine as first-line treatments, followed by antidepressants. For adults with coexisting depression, the combination of an antidepressant and stimulants has been shown to be safe and effective. 3. To monitor for misuse or diversion of stimulants, primary care clinics should consider using a controlled substances agreement and random urine drug screening in addition to regular followup visits. 4. Other medications used in children with ADHD, such as modafinil (Provigil) and the alpha agonists clonidine (Catapres) and guanfacine (Tenex), do not have enough evidence in adults TCHP_ZZ80NR Effective 4/09/2015 Page 4 of 6 to be recommended at this time and should only be considered if psychotherapy and other medications have not significantly reduced the symptoms of ADHD interfering with the adult’s daily function. Data Sources: 1. DSM-5® Diagnostic and Statistical Manual of Mental Disorders Fifth Edition, American Psychiatric Association 2. “Implementing the Key Action Statements: An Algorithm and Explanation for Process of Care for the Evaluation, Diagnosis, Treatment, and Monitoring of ADHD in Children and Adolescents” http://pediatrics.aappublications.org/content/suppl/2011/10/11/peds.20112654.DC1/zpe611117822p.pdf 3. “Practice Parameter for the Assessment and Treatment of Children and Adolescents With Attention-Deficit/Hyperactivity Disorder“ http://www.aacap.org/App_Themes/AACAP/docs/practice_parameters/jaacap_adhd_20 07.pdf 4. “Young Children With ADHD: Early Identification and Intervention” by George J. DuPaul, PhD and Lee Kern, PhD, (APA, 2011). 5. "Nonmedication Treatments for Adult ADHD: Evaluating Impact on Daily Functioning and Well-Being" (J. Russell Ramsay, 2010). 6. "Succeeding With Adult ADHD: Daily Strategies to Help You Achieve Your Goals and Manage Your Life" by Abigail Levrini, PhD, and Frances Prevatt, PhD, APA LifeTools book for the general public (APA, 2012). 7. "Attention Deficit Hyperactivity Disorder: Effectiveness of Treatment in At-Risk Preschoolers; Long-Term Effectiveness in All Ages; and Variability in Prevalence, Diagnosis, and Treatment." Comparative Effectiveness Review. 44. Rockville, MD: Agency for Healthcare Research and Quality, 2011. Web. 10 Dec. 2014. http://www.effectivehealthcare.ahrq.gov/ehc/products/191/818/CER44ADHD_20111021.pdf 8. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents U.S. Department of Health & Human Services National Institutes of Health NIH Publication No. 12-7486A October 2012 http://www.nhlbi.nih.gov/files/docs/peds_guidelines_sum.pdf 9. A PubMed search, including meta-analyses, randomized controlled trials, clinical trials, and reviews. An additional search included the Agency for Healthcare Research and Quality evidence-based practice database, the Cochrane Database of Systematic Reviews, the National Guideline Clearinghouse database, and Essential Evidence Plus TCHP_ZZ80NR Effective 4/09/2015 Page 5 of 6 Noted Resources: 1 The above listed Expert Panel (Data Source #8) has an excellent grid for cardiovascular assessment guidelines on Page 8 2 There are primarily four standardized programs of behavior training interventions for parents of preschoolers, the Triple P (Positive Parenting of Preschoolers program), Incredible Years Parenting Program, Parent-Child Interaction Therapy, and New Forest Parenting Program. Reviewed by Lynnea E. Lindsey-Pengelly, PhD, MSCP Coleen Connolly, MD Title Trillium Behavioral Health – Medical Services Director Trillium Community Health Plan, Inc. - Medical Director Date 11/01/2014 11/17/2014 Date of Creation: 11/01/2014 TCHP_ZZ80NR Effective 4/09/2015 Page 6 of 6