Modified ALL-BFM 95 protocol
advertisement

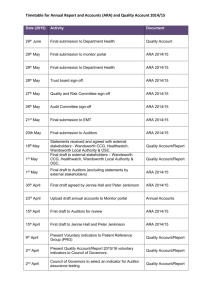
Contents The therapy protocols, details about PRBC transfusions, methods of echocardiography, electron microscopy, MRI, tests of porphyrin metabolism, genetic iron overload genes and statistics with the relevant references are presented. Drawing blood The blood samples were drawn after 8-12 hours’ of fasting. In patients who required packed red blood cell (PRBC) transfusion at admission, the pretreatment samples were drawn before PRBC transfusions were initiated. In patients whom we started iron chelation therapy, the iron parameters established only before chelation were taken into consideration, while evaluating the iron parameters during chemotherapy. Transfusions of PRBC PRBCs are prepared by automated exctractor (Bioelettronica Bagpress) and one unit of PRBC involves mean 240 cc erythrocyte suspension, each unit of PRBC involving 250 mg elementary iron (1). Patients with hemoglobin (Hb) level below or equal to 80 g/L were transfused with irradiated PRBCs with leukocyte filters, in 10 cc/kg dose, via drop counter equipment (Abbott, Lifecare Infusion System). Therefore the transfused blood was calculated as cc/kg, not Unit/kg. Therefore, for patients who gained weight within time, the values of transfused cumulative PRBC volume and iron per body weight might have been reduced. Modified ALL St Jude TXIII therapy protocol (ALL-1 Group) for high risk groups Induction: Methyl prednisolone 20 mg/kg (days 1 through 7), 10 mg/kg (days 8 through14), 2 mg/kg (days 15 through 29) (max 1 gr), vincristine 1.5 mg/kg (max 2 mg) (days 1, 8, 15, 22); daunorubicin 25 mg/m2 (max 40 mg) (days 1, 8), L-asparaginase 10 000 U/m2 (days 2,4,6, 8, 10, 12, 15, 17, 19); etoposide 300mg/m2 (days 22,25, 29), cytosine arabinoside (Ara C) 300mg/m2 (days 22,25, 29). Consolidation: Methotrexate 2 g/m2 (days 44, 51) and, at the weeks 6,14,22,30,38,46,54 Maintenance therapy: Weekly alternate therapies with the following pairs for 120 weeks: Etoposide + cyclophosphamide; 6-mercaptopurine+methotrexate; methotrexate + Ara C; prednisolone+vincristine+L-Asparaginase; etoposide + cyclophosphamide; 6-mercaptopurine+high dose methotrexate; etoposide+Ara C; prednisolone+vincristine+L-Asparaginase; etoposide + cyclophosphamide; 6-mercaptopurine+methotrexate; methotrexate+Ara C (The doses of the drugs: Vincristine:1.5 mg/m2; etoposide: 300 mg/m2; Ara C: 300 mg/m2; cyclophosphamide: 300 mg/m2; methotrexate: 40 mg/m2; 6-mercaptopurine: 75 mg/m2 for 7 days po; prednisolone: 40 mg/m2 for seven days po, L-Asparaginase: 10 000 U/m2 only for seven times) Reinduction: Same as initial induction is given from weeks 32 to 37. İntrathecal therapy: During induction on days 1, 22, 43; during maintenance at 1st, 2nd, 6th weeks, then monthly for high risk and bi-monthly for intermediate risk patients until the 54th week of maintenance Doses:<1 year of age (y): methotrexate: 6 mg, hydrocortisone: 12 mg, Ara C:18 mg; 12-23 months of age (mo): methotrexate: 8 mg, hydrocortisone: 16 mg, Ara C: 24 mg; 24-35 mo: methotrexate: 10 mg, hydrocortisone: 20 mg, Ara C: 30 mg; >36 mo: methotrexate:12 mg, hydrocortisone: 24 mg; Ara C:36 mg (Since hydrocortisone was not available, prednisolone was used instead). Central nervous system radiotherapy: Non-T, non-mature B ALL cases with WBC>100 x 109/L at admission, non-T ALL cases with WBC> 50 x 109/L at admission, Ph+ ALL and patients with initial CNS leukemia receive 1800 cGy cranial irradiation coupled with five triple intrathecal (it) treatments at week 56 of continuation (2). TR ALL-BFM Therapy Protocol (Modified ALL-BFM 95 protocol) Therapy of Medium Risk Group (MRG) Protocol I Phase 1 (P1P1): Prednisolone 60 mg/m2po (days 5 through 28. 1st day %25 of the total, days 2 through 5, dose elevated by %25/g; dose is tapered down through days 29-37), vincristine 1.5 mg/m2 (days 8,15,22,29), daunorubicin 30 mg/m2 (days 8,15, 22, 29), L-asparaginase 5000 U/m2 (days 12,15,18,21,24,27,30,33), intrathecal methotrexate 12 mg (days 1,12,33). Protocol I Phase 2 (P1P2): Cyclophosphamide 1000 mg/m2 (days 36 and 64), mesna 400 mg/m2 /dose (at hours 0th, 4th, 8th hours of cyclophosphamide), furosemide 0.5 mg/kg (after 6 and 12 hours of cyclophosphamide), cytosine arabinoside (Ara-C) 75 mg/m2 (days 38 through 41, 45 through 48, 52 through 55, 59 through 62), 6-mercaptopurine 60 mg/m2 (days 36 through 63). Protokol M: 6mercaptopurine 25 mg/m2 /gün (through 8 weeks), methotrexate 5 g/m2 (days 8, 22, 36, 50), calcium folinate 15mg/m2 /dose (at 42th, 48th, 54th, 60th hours after methotrexate), intrathecal methotrexate 12 mg (days 8, 22, 36, 50). Protokol II Phase 1 (P2P1): Dexamethasone 10 mg/m2 (days 1 through 21; tapering the dose through days 22-31), vincristine 1.5 mg/m2, doxorubicin 30 mg/m2 (days 8,15,22,29), L-asparaginase 10000 U/m2 (days 8,11,15,18). Protocol II Phase 2 (P2P2): Cyclophosphamide 1000 mg/m2 infusion (day 36), mesna 400 mg/m2 (0th, 4th, 8th hours of cyclophosphamide), furosemide 0.5 mg/kg (6 and 12 hours after cyclophosphamide), 6thioguanine 60 mg/m2 (days 36 through 49), Ara C 75 mg/m2 (days 38 through 41 and 45 through 48), intratehecal methotrexate 12 mg (days 38 and 45) Prophylactic cranial radiotherapy:> 1 year of age: 12 Gy Maintenance: 6-mercaptopurine 50-75 mg/m2 /day po (until the whole therapy is completed to 24 months), methotrexate 20 -30mg/m2 /day po (until the whole therapy is completed to 24 months). Therapy of Standard Risk Group (SRG): The same with therapy for ALL-MRG group except that daunorubicine is administered 30 mg/m2 (on days 8 and 15). The maintenance is administered until the time elapsed between the beginning to the end of the therapy is 24 mo in girls and 36 mo in boys. No prophylactic cranial radiotherapy is administered. Therapy for High Risk Group (HRG): The order of therapy blocks: P1P1; blocks of HR1’, HR2, HR3, HR1, HR2, HR3; P2P1, P2P2, Prophylactic cranial radiotherapy; Maintenance. Protocol I Phase 1:Prednizolone 60 mg/m2 /d po (tapering the dose down starts on days 22 through 31), vincristine 1,5 mg/m2 (days 8,15 ,22, 29), daunorubicine 30 mg/m2 (days 8,15,22,29), L-asparaginase 5000 U/m2 (days 12,15,18,21,24,27), intratechal methotrexate 12 mg (days 1,12,27). HR1’(HR1’) block: Dexametazone 20mg/m2 /d po/iv (days 1 through 5); methotrexate 1g/m2 (day 1); cyclophosphamide 200mg/m2 2x1, days 2 through 4; 5 doses), mesna 70 mg/m2 (at 0th, 4th, 8th hours after cyclophosphamide); L-asparaginase 25000 U/m2 (day 6), Ara-C 2 g/m2 (day 5; 2x1). HR2 block: Dexametasone 20 mg/m2 /d po/iv (days 1 through 5); vindesin 3 mg/m2 (max 5 mg) (days 1, 6; if vindesin is not available vincristine 1,5 mg/m2 (max 2 mg),methotrexate 1 g/m2 (day 1; ifosfamide 800 mg/m2, 2x1, days 2 through 4; 5 times), mesna 300 mg/m2 at 0th, 4th, 8th hours of ifosfamide), daunorubicine 30 mg/m2 (day 5), L-asparaginase 25000 U/m2 (day 6). HR3 block: Dexamethasone 20 mg/m2 /d po/iv(days 1 through 5); L-asparaginase 25000 U/m2 (day 6), Ara-C 2 g/m2 (days 1,2; 2x1, 4 times), etoposide 100 mg/m2 (days 3 through 5; 2x1; 5 times); HR1 block: The same with HR’, except that it involves vincristine 1.5 mg/m2 (max 2 mg (days 1, 6). Intrathecal therapy: methotrexate 12 mg, Ara C 30 mg, prednisolone 10 mg on day 1 of all HR blocks. Protokol II, prophylactic radiotherapy and maintenance are the same with those of SRG and MRG groups. Maintenance is given until the time elapsed between the beginning and the end of the therapy s 24 mo. Cranial radiotherapy for children with CNS leukemia: 1-2 year of age: 12 Gy and >2 years of age: 18 Gy. Additional intrathecal therapy on days 18 and 27 of protocol I phase 1 for SRG and MRG patients, on day 18 for HRG patients; days 1 and 20 of P2P1 for all risk patients (3,4). COG 1962 Therapy Protocol Induction: Prednisone (60 mg/m2 /d po, days 0-27, tapering the dose on days 28 through 37), vincristine (1,5 mg/m2, days 0,7,14,21), daunomycine (25 mg/m2, days 0,7,14,21), L-Asparaginase 6 000 U/m2, days Monday,Wednesday,Friday, 9 times, days 3-21), Intrathecal therapy: Ara C (day 0) in doses: 1 y: 30 mg; 2y: 50 mg; >3y: 70 mg). Methotrexate (days 14, 28) in doses: 1y: 8 mg; 2y: 10 mg; >3y: 12 mg) (5). AML- BFM 2004 Protocol The order of therapy blocks For HRG patients: AIE (induction 1), HAM (induction 2), AI (consolidation), haM (intensification 1), HAE (intensification 2), prophylactic cranial radiotherapy and maintenance. For SRG patients: AIE (induction 1), AI (induction 2), haM (consolidation), HAE (intensification), prophylactic cranial radiotherapy, maintenance. Block AIE: Ara C 100 mg/m2 continued infusion (day 1 through 2), Ara C 100 mg/m2 2x1 (days 3 through 8), VP-16 150 mg/m2/d (days 6,7,8), idarubicine 12 mg/m2 (days 3,5,7), intrathecalAra C in age matched dose (day 1). Block HAM:Mitoxantrone 10 mg/m2 (days 3, 4), Ara C 3 g/m2, 2x1, 6 doses, days 1 through 3); intrathecalAra C in age matched dose (day 1). Block AI:Idarubicine 7 mg/m2 (days 3, 5), Ara C 500 mg/m2 (days 1 through 5), intrathecalAra C in age matched dose (day 1,6). Block haM: Ara C: 1 g/m2 2x1, 6 doses, days 1-3), mitoxantrone 10 mg/m2 (day 3, 4), intrathecalAra C in age matched dose (day 1, 6). Block HAE:Ara C 3 g/m2 2x1, 6 doses (days 1-3), etoposide 125 mg/m2 (days 2-5), intrathecalAra C in age matched dose (day 1). Maintenance: Cytarabine 40 mg/m2 consecutive 4 days every month, 6-Thioguanine 40 mg/m2 /d for 1 year po, intrathecalAra C in age matched dose (day 1,8,15,22 beginning concomitant with CNS irradiation). IntrathecalAra C: <1 y:20 mg; 1-<2 y: 26 mg, 2-<3 y: 34 mg, >3 y: 40 mg). Prophylactic cranial radiotherapy: >1 year of age: 12 Gy. (6). MRI Methods T2* method: The patients were evaluated for cardiac and hepatic iron status by using 1.5-T scanner (Siemens Symphony, Erlangen Germany) with multi-TE gradient Echo T2* magnetic resonance imaging (MRI). The parameters for cardiac T2* imaging were TR = 124, TE = 2.97– 22.6ms, FA = 20°, FOV = 400 mm, RFOV = 50–60%, and slice thickness = 10 mm. The parameters for liver T2* imaging were TR = 200, TE = 1.3–23 ms, FA = 20°, FOV = 400, RFOV = 50–75%, and slice thickness10 mm. The liver and cardiac T2* images were obtained from the level of the portal hilus and midventricular line respectively. Measurements were made by using CMR tools (7). R2 method: The patients were evaluated for hepatic iron status by using 1.5-T scanner (GE HDx 1.5 Tesla MR, USA), using different gradient sequences, in the axial plan. The sequences which we used were GRE 120/14 (Flipangle 20), GRE 120/4G(Flipangle 20), GRE 120/4G(Flipangle 90), GRE 120/9G(Flipangle 20), GRE 120/21G(Flipangle 20). The signal intensity in the liver and paravertebral muscles was measured with ROI. The values were determined using the gradient recalled echo sequences established at the University of Rennes (8). Procedure of evaluation of iron overload genes The genomic DNA wasextractedfromfreshbloodwith EDTA usingNucleoSpin Blood DNA Extraction kit (Macherey-Nagel, Duren, Germany). The mutations were analyzed by reverse hybridization using Haemochromatosis Strip Assay A kit (Vienna Lab Labordiagnostika GmbH, Vienna, Austria) according to the manufacturer’s instructions. Briefly, thisassay has twostepsafterthe DNA isolation. First, a multiplexpolymerasechainreaction (PCR) amplification is performed using biotinylated primers, and later amplification products are hybridized to a test strip containing allele-specific oligonucleotide probes. Bound biotinylated amplification products are detected using streptavidin-alkaline phosphatase and color substrates. Interpretation of the results was performed according to the manufacturer’s instructions (9). Echocardiographic evaluation Echocardiographic evaluations were made before initiation of therapy, in all groups and every six months in ALL-1 on days 8,22 of P2P1 and before every HR block in ALL-2 and before every block in AML. All patients were shown to have normal cardiac functions. Light and transmission electron microscopic (TEM) evaluation Bone marrow smears were stained with Giemza and Prussian blue for light microscopic evaluation. Bone marrow of four ALL-2 and one AML patient which were obtained during chemotherapy when indicated in the protocols were evaluated with TEM. Procedure of electron microscopic evaluation: Bone marrow samples were fixed in 3% gluteraldehyde in 0,2 M phosphate buffer and were washed with 0,1 M phosphate buffer. Postfixation with 1% osmium tetroxide was performed and the specimens were dehydrated in a graded series of ethanol and embedded in Araldite CY- 212. Ultrathin serial sections were cut on a Leica Ultracut R ultramicrotome (Leica, Vienna, Austria) and stained with lead citrate anduranyl acetate examined by Leo 906 E TEM (80 KV) (Oberkohen –Germany) (10). Procedure of evaluation of porphyria metabolism Aminolevulinic acid (ALA) and porphobilinogen (PBG) in urine were evaluated, the day after the end of their last chemotherapy block (after HR1,HR2, HR3 blocks in one ALL, after protocol M in another, and after HAE block, in one AML patient). One of the ALL patients was additionally evaluated for protoporphyrin and coproporphyrins in blood . Procedure: A sample of urine from 24 hours specimen collected in dark colored bottles, was passed consecutively through two chromatographic columns that contain ionic exchance resins; the first one retains PBG, while the second retains ALA. Once the interfering substances are removed by washing, ALA and PBG are eluted and quantified by the absorbance 555 nm of the Ehrlich's reaction product by spectrophotometer (LABOSPEC –England) (11). Statistics The data was statistically evaluated through SPSS 15 package program. For comparison of two groups, Mann-Whitney U test; for three-four group comparisons Krukall-Wallis H test; for comparison of dependent groups, Wilcoxon test were used. For the evaluation of relationship between the variables, correlation analysis was made. Significance level was accepted as 0.05. REFERENCES 1) Knovich MA, Storey JA, Coffman LG, et al. Ferritin for the clinician. Blood Rev 2009; 23: 95-104. 2) Gürgey A, Yetgin S, Çetin M, et al. Acute lymphoblastic leukemia in infants. Turk J Pediatr 2004;46: 115-9. 3) Yüksel-Soycan L, Aydogan G, Tanyeli A, et al. BFM-TR ALL 2000: First Turkish multicentric study in the treatment of pediatric acute lymphoblastic leukemia. Ped Blood Cancer 2006;47:426-7. 4) Möricke A, Reiter A, Zimmermann M, et al. Risk-adjusted therapy of acute lymphoblastic leukemia can decrease treatment burden and improve survival: treatment results of 2169 unselected pediatric and adolescent patients enrolled in the trial ALL-BFM 95. Blood 2008; 111: 4477-89. 5) Avramis VI, Sencer S, Periciou AP, et al. A randomized comparison of native Escherichia coli asparaginase and polyethylene glycol conjugated asparaginase for treatment of children with newly diagnosed standard-risk acute lymphoblastic leukemia: a Children’s Cancer Group study. Blood 2002; 99: 1986-94. 6) Creutzig U, Zimmermann M, Bourquin J-P, et al. CNS irradiation in pediatric acute myeloid leukemia: Equal results by 12 or 18 Gy in studies AML-BFM98 and 2004. Pediatr Blood Cancer 2011; 57: 986-92. 1 7) Fernandes JL, Sampaio EF, Verissimo M, et al. Heart and liver T2* assessment for iron overload using different software programs. EurRadiol DOI 10.1007/s00330-011-2208-1. 8) Gandon Y. Iron and liver. Available at: http://www.radio.univ- rennes1.fr/Sources/EN/Hemo.html. 9) Oberkanins C, Moritz A, de Villiers JN, et al. A reverse-hybridization assay for the rapid and simultaneous detection of nine HFE gene mutations. Genet Test 2000;4:121-4. 10) Dykstra MJ. A manual applied techniques for biological electron microscopy. New York: Plenum Press; 1993: 1-65. 11) Mauzerall D, Granick S. The occurence and determination of Delta-Aminolevulinic acid and porphobilinogen in urine. J. Biol Chem 1956, 219:435-46. Legends to figures Figure 1S. Changes in the iron parameters and transfused cumulative PRBC volume and iron per body weight, in ALL-1 group who received modified St Jude TXIII protocol Figure 2S. Changes in the iron parameters and transfused cumulative PRBC volume and iron per body weight, in ALL-2 group who received TRALL-BFM protocol Figure 3S. Changes in the iron parameters and transfused cumulative PRBC volume and iron per body weight, in ALL-3 group who received COG 1962 ALL protocol, only during remission induction Figure 4S. Light microscopic appearences of bone marrow cells stained with giemza and Prussian Blue (x100) A,B, F: Free iron within the bone marrow matrix in an ALL patient in remission (A) and an AML patient at admission (B,F); C,E,F,H: Siderocytes; G,H: Iron within platelets; I: An iron laden macrophage; J,K: Dyserythropoiesis (orthochromic erythrocytes with laced cytoplasm); L,M,N: Dyserythropoiesis (long chromatin bridges); N,O: Dysmyelopoiesis (agranular stab and metamyelocytes); P: Apoptosis