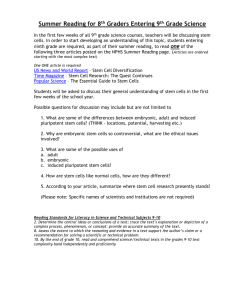
Embryonic Stem Cells - The DocMelillo Experience
advertisement

* CLONING FACT SHEET http://www.genome.gov/25020028 What is cloning? The term cloning describes a number of different processes that can be used to produce genetically identical copies of a biological entity. The copied material, which has the same genetic makeup as the original, is referred to as a clone. Researchers have cloned a wide range of biological materials, including genes, cells, tissues and even entire organisms, such as a sheep. Top of page Do clones ever occur naturally? Yes. In nature, some plants and single-celled organisms, such as bacteria, produce genetically identical offspring through a process called asexual reproduction. In asexual reproduction, a new individual is generated from a copy of a single cell from the parent organism. Natural clones, also known as identical twins, occur in humans and other mammals. These twins are produced when a fertilized egg splits, creating two or more embryos that carry almost identical DNA. Identical twins have nearly the same genetic makeup as each other, but they are genetically different from either parent. Top of page What are the types of artificial cloning? There are three different types of artificial cloning: gene cloning, reproductive cloning and therapeutic cloning. Gene cloning produces copies of genes or segments of DNA. Reproductive cloning produces copies of whole animals. Therapeutic cloning produces embryonic stem cells for experiments aimed at creating tissues to replace injured or diseased tissues. Gene cloning, also known as DNA cloning, is a very different process from reproductive and therapeutic cloning. Reproductive and therapeutic cloning share many of the same techniques, but are done for different purposes. Top of page What sort of cloning research is going on at NHGRI? Gene cloning is the most common type of cloning done by researchers at the National Human Genome Research Institute (NHGRI). NHGRI researchers have not cloned any mammals and NHGRI does not clone humans. Top of page How are genes cloned? Researchers routinely use cloning techniques to make copies of genes that they wish to study. The procedure consists of inserting a gene from one organism, often referred to as "foreign DNA," into the genetic material of a carrier called a vector. Examples of vectors include bacteria, yeast cells, viruses or plasmids, which are small DNA circles carried by bacteria. After the gene is inserted, the vector is placed in laboratory conditions that prompt it to multiply, resulting in the gene being copied many times over. Top of page How are animals cloned? The technique used to clone whole animals, such as sheep, is referred to as reproductive cloning. In reproductive cloning, researchers remove a mature somatic cell, such as a skin cell or an udder cell, from an animal that they wish to copy. They then transfer the DNA of the donor animal's somatic cell into an egg cell, or oocyte, that has had its own DNAcontaining nucleus removed. Researchers can add the DNA from the somatic cell to the empty egg in two different ways. In the first method, they remove the DNA-containing nucleus of the somatic cell and inject it into the empty egg. In the second approach, they use an electrical current to fuse the entire somatic cell with the empty egg. In both processes, the egg is allowed to develop into an early-stage embryo in the test-tube and then is implanted into the womb of an adult female animal. Ultimately, the adult female gives birth to an animal that has the same genetic make up as the animal that donated the somatic cell. This young animal is referred to as a clone. Reproductive cloning may require the use of a surrogate mother to allow development of the cloned embryo, as was the case for the most famous cloned organism, Dolly the sheep. Reproductive cloning may require the use of a surrogate mother to allow development of the cloned embryo, as was the case for the most famous cloned organism, Dolly the sheep. Top of page What animals have been cloned? Over the last 50 years, scientists have conducted cloning experiments in a wide range of animals using a variety of techniques. In 1979, researchers produced the first genetically identical mice by splitting mouse embryos in the test tube and then implanting the resulting embryos into the wombs of adult female mice. Shortly after that, researchers produced the first genetically identical cows, sheep and chickens by transferring the nucleus of a cell taken from an early embryo into an egg that had been emptied of its nucleus. It was not until 1996, however, that researchers succeeded in cloning the first mammal from a mature (somatic) cell taken from an adult animal. After 276 attempts, Scottish researchers finally produced Dolly, the lamb from the udder cell of a 6-year-old sheep. Two years later, researchers in Japan cloned eight calves from a single cow, but only four survived. Besides cattle and sheep, other mammals that have been cloned from somatic cells include: cat, deer, dog, horse, mule, ox, rabbit and rat. In addition, a rhesus monkey has been cloned by embryo splitting. Top of page Have humans been cloned? Despite several highly publicized claims, human cloning still appears to be fiction. There currently is no solid scientific evidence that anyone has cloned human embryos. In 1998, scientists in South Korea claimed to have successfully cloned a human embryo, but said the experiment was interrupted very early when the clone was just a group of four cells. In 2002, Clonaid, part of a religious group that believes humans were created by extraterrestrials, held a news conference to announce the birth of what it claimed to be the first cloned human, a girl named Eve. However, despite repeated requests by the research community and the news media, Clonaid never provided any evidence to confirm the existence of this clone or the other 12 human clones it purportedly created. In 2004, a group led by Woo-Suk Hwang of Seoul National University in South Korea published a paper in the journal Science in which it claimed to have created a cloned human embryo in a test tube. However, an independent scientific committee later found no proof to support the claim and, in January 2006, Science announced that Hwang's paper had been retracted. From a technical perspective, cloning humans and other primates is more difficult than in other mammals. One reason is that two proteins essential to cell division, known as spindle proteins, are located very close to the chromosomes in primate eggs. Consequently, removal of the egg's nucleus to make room for the donor nucleus also removes the spindle proteins, interfering with cell division. In other mammals, such as cats, rabbits and mice, the two spindle proteins are spread throughout the egg. So, removal of the egg's nucleus does not result in loss of spindle proteins. In addition, some dyes and the ultraviolet light used to remove the egg's nucleus can damage the primate cell and prevent it from growing. Top of page Do cloned animals always look identical? No. Clones do not always look identical. Although clones share the same genetic material, the environment also plays a big role in how an organism turns out. For example, the first cat to be cloned, named Cc, is a female calico cat that looks very different from her mother. The explanation for the difference is that the color and pattern of the coats of cats cannot be attributed exclusively to genes. A biological phenomenon involving inactivation of the X chromosome (See sex chromosome) in every cell of the female cat (which has two X chromosomes) determines which coat color genes are switched off and which are switched on. The distribution of X inactivation, which seems to occur randomly, determines the appearance of the cat's coat. Top of page What are the potential applications of cloned animals? Reproductive cloning may enable researchers to make copies of animals with the potential benefits for the fields of medicine and agriculture. For instance, the same Scottish researchers who cloned Dolly have cloned other sheep that have been genetically modified to produce milk that contains a human protein essential for blood clotting. The hope is that someday this protein can be purified from the milk and given to humans whose blood does not clot properly. Another possible use of cloned animals is for testing new drugs and treatment strategies. The great advantage of using cloned animals for drug testing is that they are all genetically identical, which means their responses to the drugs should be uniform rather than variable as seen in animals with different genetic make-ups. After consulting with many independent scientists and experts in cloning, the U.S. Food and Drug Administration (FDA) decided in January 2008 that meat and milk from cloned animals, such as cattle, pigs and goats, are as safe as those from non-cloned animals. The FDA action means that researchers are now free to using cloning methods to make copies of animals with desirable agricultural traits, such as high milk production or lean meat. However, because cloning is still very expensive, it will likely take many years until food products from cloned animals actually appear in supermarkets. Another application is to create clones to build populations of endangered, or possibly even extinct, species of animals. In 2001, researchers produced the first clone of an endangered species: a type of Asian ox known as a guar. Sadly, the baby guar, which had developed inside a surrogate cow mother, died just a few days after its birth. In 2003, another endangered type of ox, called the Banteg, was successfully cloned. Soon after, three African wildcats were cloned using frozen embryos as a source of DNA. Although some experts think cloning can save many species that would otherwise disappear, others argue that cloning produces a population of genetically identical individuals that lack the genetic variability necessary for species survival. Some people also have expressed interest in having their deceased pets cloned in the hope of getting a similar animal to replace the dead one. But as shown by Cc the cloned cat, a clone may not turn out exactly like the original pet whose DNA was used to make the clone. Top of page What are the potential drawbacks of cloning animals? Reproductive cloning is a very inefficient technique and most cloned animal embryos cannot develop into healthy individuals. For instance, Dolly was the only clone to be born live out of a total of 277 cloned embryos. This very low efficiency, combined with safety concerns, presents a serious obstacle to the application of reproductive cloning. Researchers have observed some adverse health effects in sheep and other mammals that have been cloned. These include an increase in birth size and a variety of defects in vital organs, such as the liver, brain and heart. Other consequences include premature aging and problems with the immune system. Another potential problem centers on the relative age of the cloned cell?s chromosomes. As cells go through their normal rounds of division, the tips of the chromosomes, called telomeres, shrink. Over time, the telomeres become so short that the cell can no longer divide and, consequently, the cell dies. This is part of the natural aging process that seems to happen in all cell types. As a consequence, clones created from a cell taken from an adult might have chromosomes that are already shorter than normal, which may condemn the clones' cells to a shorter life span. Indeed, Dolly, who was cloned from the cell of a 6-year-old sheep, had chromosomes that were shorter than those of other sheep her age. Dolly died when she was six years old, about half the average sheep's 12-year lifespan. Top of page What is therapeutic cloning? Therapeutic cloning involves creating a cloned embryo for the sole purpose of producing embryonic stem cells with the same DNA as the donor cell. These stem cells can be used in experiments aimed at understanding disease and developing new treatments for disease. To date, there is no evidence that human embryos have been produced for therapeutic cloning. The richest source of embryonic stem cells is tissue formed during the first five days after the egg has started to divide. At this stage of development, called the blastocyst, the embryo consists of a cluster of about 100 cells that can become any cell type. Stem cells are harvested from cloned embryos at this stage of development, resulting in destruction of the embryo while it is still in the test tube. In November 2007, using a new cloning method that removes the egg's nucleus without dyes or ultraviolet light, researchers produced the first primate embryonic stem cells. The work involved transferring the nucleus of a skin cell from a male rhesus monkey into the nucleus-free egg of a female rhesus monkey. These embryonic stem cells did not develop into a whole monkey, and researchers said their work was aimed at therapeutic applications. However, the research shows that, with some adjustments, the techniques used to make whole copies of other animals may also work in primates. Top of page What are the potential applications of therapeutic cloning? Researchers hope to use embryonic stem cells, which have the unique ability to generate virtually all types of cells in an organism, to grow tissues in the laboratory that can be used to grow healthy tissue to replace injured or diseased tissues. In addition, it may be possible to learn more about the molecular causes of disease by studying embryonic stem cell lines from cloned embryos derived from the cells of animals or humans with different diseases. Top of page What are the potential drawbacks of therapeutic cloning? Many researchers think it is worthwhile to explore the use of embryonic stem cells as a path for treating human diseases. However, some experts are concerned about the striking similarities between stem cells and cancer cells. Both cell types have the ability to proliferate indefinitely and some studies show that after 60 cycles of cell division, stem cells can accumulate mutations that could lead to cancer. Therefore, the relationship between stem cells and cancer cells needs to be more clearly understood if stem cells are to be used to treat human disease. Top of page What are some of the ethical issues related to cloning? Gene cloning is a carefully regulated technique that is largely accepted today and used routinely in many labs worldwide. However, both reproductive and therapeutic cloning raise important ethical issues, especially as related to the potential use of these techniques in humans. Reproductive cloning would present the potential of creating a human that is genetically identical to another person who has previously existed or who still exists. This may conflict with long-standing religious and societal values about human dignity, possibly infringing upon principles of individual freedom, identity and autonomy. However, some argue that reproductive cloning could help sterile couples fulfill their dream of parenthood. Others see human cloning as a way to avoid passing on a deleterious gene that runs in the family without having to undergo embryo screening or embryo selection. Therapeutic cloning, while offering the potential for treating humans suffering from disease or injury, would require the destruction of human embryos in the test tube. Consequently, opponents argue that using this technique to collect embryonic stem cells is wrong, regardless of whether such cells are used to benefit sick or injured people. * Stem Cell Debate: Is it Over? http://learn.genetics.utah.edu/content/tech/stemcells/scissues/ Both human embryonic stem (hES) cells and induced pluripotent stem (iPS) cells are pluripotent: they can become any type of cell in the body. While hES cells are isolated from an embryo, iPS cells can be made from adult cells. Stem cell therapies are not new. Doctors have been performing bone marrow stem cell transplants for decades. But when scientists learned how to remove stem cells from human embryos in 1998, both excitement and controversy ensued. The excitement was due to the huge potential these cells have in curing human disease. The controversy centered on the moral implications of destroying human embryos. Political leaders began to debate over how to regulate and fund research involving human embryonic stem (hES) cells. New breakthroughs may soon bring this debate to an end. Scientists have learned how to stimulate a patient's own cells to behave like embryonic stem cells. These so-called induced pluripotent stem (iPS) cells are reducing the need for human embryos in research and opening up exciting new possibilities for stem cell therapies. The Ethical Questions Until recently, the only way to get pluripotent stem cells for research was to remove the inner cell mass of an embryo and put it in a dish. The thought of destroying a human embryo can be unsettling, even if it is only five days old. Stem cell research thus raised difficult questions: Does life begin at fertilization, in the womb, or at birth? Is a human embryo equivalent to a human child? Does a human embryo have any rights? Might the destruction of a single embryo be justified if it provides a cure for a countless number of patients? Since ES cells can grow indefinitely in a dish and can, in theory, still grow into a human being, is the embryo really destroyed? IPS Cells: Problem Solved? With iPS cells now available as an alternative to hES cells, the debate over stem cell research is becoming increasingly irrelevant. But ethical questions regarding hES cells may not entirely go away. Inevitably, some human embryos will still be needed for research. iPS cells are not exactly the same as hES cells, and hES cells still provide important controls: they are a gold standard against which the "stemness" of iPS cells is measured. Some experts believe it's wise to continue the study of all stem cell types, since we're not sure yet which one will be the most useful for cell replacement therapies. An additional ethical consideration is that iPS cells have the potential to develop into a human embryo, in effect producing a clone of the donor. Many nations are already prepared for this, having legislation in place that bans human cloning. Stem Cell Research Legislation Governments around the globe have passed legislation to regulate stem cell research. In the United States, laws prohibit the creation of embryos for research purposes. Scientists instead receive "leftover" embryos from fertility clinics with consent from donors. Most people agree that these guidelines are appropriate. Disagreements surface, however, when political parties debate about how to fund stem cell research. The federal government allocates billions of dollars each year to biomedical research. But should taxpayer dollars be used to fund embryo and stem cell research when some believe it to be unethical? Legislators have had the unique challenge of encouraging advances in science and medicine while preserving a respect for life. U.S. President Bush, for example, limited federal funding to a study of 70 or so hES cell lines back in 2001. While this did slow the destruction of human embryos, many believe the restrictions set back the progress of stem cell research. President Obama overturned Bush's stem cell policy in 2009 to expand the number of stem cell lines available to researchers. Policy- makers are now grappling with a new question: Should the laws that govern iPS cells differ from those for hES cells? If so, what new legislation is needed? Regulations and policies change frequently to keep up with the pace of research, as well as to reflect the views of different political parties. Here President Obama signs an executive order on stem cells, reversing some limits on federal research funding. (White House photo by Chuck Kennedy) *How Stem Cells Work http://science.howstuffworks.com/life/cellular-microscopic/stem-cell6.htm How Stem Cells Work by Stephanie Watson and Craig Freudenrich, Ph.D. Stem Cell Research Advocates Since 1991, when he was diagnosed with Parkinson's disease (a degenerative brain disorder that affects movement), actor Michael J. Fox has been a vocal proponent for stem cell research. His foundation has donated more than $205 million to help fund Parkinson's research [source: Michael J. Fox Foundation]. Fox and his foundation are hoping that scientists will one day be able to coax stem cells into producing dopamine, a chemical in the body that is deficient in patients with Parkinson's disease. Former first lady Nancy Reagan also became an advocate for stem cell research when her husband, former President Ronald Reagan, was stricken with Alzheimer's, another degenerative brain disease. He died of Alzheimer's in the summer of 2004. Stem Cell Research Controversy Stem cell research has become one of the biggest issues dividing the scientific and religious communities around the world. At the core of the issue is one central question: When does life begin? At this time, to get stem cells that are reliable, scientists either have to use an embryo that has already been conceived or else clone an embryo using a cell from a patient's body and a donated egg. Either way, to harvest an embryo's stem cells, scientists must destroy it. Although that embryo may only contain four or five cells, some religious leaders say that destroying it is the equivalent of taking a human life. Inevitably, this issue entered the political arena. In 1996, Congress passed a rider to the federal appropriations bill called the Dickey-Wicker amendment. Representatives Jay Dickey and Roger Wicker proposed banning the use of federal monies for any research in which a human embryo is created or destroyed. Federal monies are a primary source of funding for stem cell research. The amendment has been renewed every year since that time. In 2001, President George W. Bush further restricted federal stem cell research. In an executive order, Bush stated that federal funds could only be used for research on human embryonic stem cell lines that had already been established (only 22 cell lines). This prevented researchers from creating more embryonic stem cell lines for research. In 2009, President Barack Obama issued an executive order to expand embryonic stem cell research. Obama's administration allowed federal funding of embryonic stem cell research if the following conditions applied: The cell line was one of the 22 in existence during the Bush administration or was created from embryos that had been discarded after in vitro fertilization procedures. The donors of the embryos were not paid in any way. The donors clearly knew that the embryos would be used for research purposes prior to giving consent. According to the administration, the new policy did not violate the Dickey-Wicker amendment because the money did not finance the creation of new embryos (they had already been created by private means) and did not finance the destruction of them. In 2009, two researchers from Boston, Dr. James Sherley of the Boston Biomedical Research Institute and Dr. Theresa Deisher of the Ava Maria Biotechnology Company, and other agencies filed a lawsuit against the government. Initially, the lawsuit was dismissed because the judge ruled that the plaintiffs had no legal standing (i.e. they were not affected materially by the new rules). However, a court of appeals overturned the initial ruling. The two scientists remained plaintiffs. The scientists claimed that, because they used adult stem cells exclusively in their research, the new rules would increase competition for federal research dollars, thereby affecting their ability to obtain funding. Federal Judge Royce Lamberth upheld the appeals court ruling. He placed an injunction preventing the new rules from going into place. He claimed that the rules violated the Dickey-Wicker amendment because embryos must be destroyed in the process of creating embryonic stem cell lines. In September 2010, The New York Times reported that the U.S. Court of Appeals ruled that federal funding of embryonic stem cell research could continue under the new rules while the court considers Judge Lamberth's ruling [source: New York Times]. This ruling allows researchers to continue feeding embryonic stem cell cultures, experimenting with mice, and other research activities until this court rules, the U.S. Supreme Court weighs in, or Congress passes legislation that clarifies the issues. In the meantime, stem cell research and the careers of stem cell researchers hang on a legal roller coaster. Although stem cells have great potential for treating diseases, much work on the science, ethical and legal fronts remains. Stem Cell Basics A stem cell is essentially the building block of the human body. Stem cells are capable of dividing for long periods of time, are unspecialized, but can develop into specialized cells. The earliest stem cells in the human body are those found in the human embryo. The stem cells inside an embryo will eventually give rise to every cell, tissue and organ in the fetus's body. Unlike a regular cell, which can only replicate to create more of its own kind of cell, a stem cell is pluripotent. When it divides, it can make any one of the 220 different cells in the human body. Stem cells also have the capability to self-renew -- they can reproduce themselves many times over. There are several types of stem cells, including: Embryonic stem cells - Embryonic stem cells include those found within the embryo, the fetus or the umbilical cord blood. Depending upon when they are harvested, embryonic stem cells can give rise to just about any cell in the human body. Adult stem cells - Adult stem cells can be found in infants, children and adults. They reside in already developed tissues such as those of the heart, brain and kidney. They usually give rise to cells within their resident organs. Induced pluripotent stem cells (IPSC)- These stem cells are adult, differentiated cells that have been experimentally "reprogrammed" into a stem cell-like state. Embryonic Stem Cells Once an egg cell is fertilized by a sperm, it will divide and become an embryo. In the embryo, there are stem cells that are capable of becoming all of the various cell types of the human body. For research, scientists get embryos in two ways. Many couples conceive by the process of in vitro fertilization. In this process, a couple's sperm and eggs are fertilized in a culture dish. The eggs develop into embryos, which are then implanted in the female. However, more embryos are made than can be implanted. So, these embryos are usually frozen. Many couples donate their unused embryos for stem cell research. The second way in which scientists get embryos is therapeutic cloning. This technique merges a cell (from the patient who needs the stem cell therapy) with a donor egg. The nucleus is removed from the egg and replaced with the nucleus of the patient's cell. (For a detailed look at the process, see How Cloning Works) This egg is stimulated to divide either chemically or with electricity, and the resulting embryo carries the patient's genetic material, which significantly reduces the risk that his or her body will reject the stem cells once they are implanted. Both methods -- using existing fertilized embryos and creating new embryos specifically for research purposes -- are controversial. But before we get into the controversy, let's find out how scientists get stem cells to replicate in a laboratory setting in order to study them. When an embryo contains about eight cells, the stem cells are totipotent - they can develop into all cell types. At three to five days, the embryo develops into a ball of cells called a blastocyst. A blastocyst contains about 100 cells total and the stem cells are inside. At this stage, the stem cells are pluripotent - they can develop into almost any cell type. HowStuffWorks / Lee Dempsey To grow the stem cells, scientists remove them from the blastocyst and culture them (grow them in a nutrient-rich solution) in a Petri dish in the laboratory. The stem cells divide several times and scientists divide the population into other dishes. After several months, there are millions of stem cells. If the cells continue to grow without differentiating, then the scientists have a stem cell line. Cell lines can be frozen and shared between laboratories. As we will see later, stem cell lines are necessary for developing therapies. Today, many expectant mothers are asked about umbilical cord banking -- the process of storing umbilical cord blood after giving birth. Why would someone want to do that? Once a mother gives birth, the umbilical cord and remaining blood are often discarded. However, this blood also contains stem cells from the fetus. Umbilical cord blood can be harvested and the embryonic stem cells grown in culture. Unlike embryonic stem cells from earlier in development, fetal stem cells from umbilical cord blood are multipotent - they can develop into a limited number of cell types. Adult Stem Cells You can think of adult stem cells as our built-in repair kits, regenerating cells damaged by disease, injury and everyday wear and tear. These undifferentiated cells reside among other differentiated cells in a tissue or organ; they divide and become specialized to repair or replace the surrounding differentiated cells. A common example of adult stem cells is hemopoietic stem cells, which are found in red bone marrow. These stem cells differentiate into various blood cells (red blood cells, lymphocytes, platelets-- see How Blood Works for more information). For example, red blood cells are not capable of reproducing and survive for about 28 days. To replace worn-out red blood cells, hemopoietic stem cells in the bone marrow divide and differentiate into new red blood cells. Bone marrow also contains a second type of adult stem cell known as a stromal or mesenchymal stem cell. Stromal stem cells become bone, cartilage, fat and connective tissues found in bone. Adult stem cells have also been found in many other tissues such as the brain, skeletal muscle, blood vessels, skin, liver, teeth and the heart. Regardless of the source, adult stem cells are multipotent they can develop into a limited number of cell types. Although adult stem cells exist in many tissues, their numbers are small, perhaps one adult stem cell for every 100,000 surrounding cells. These stem cells look like the surrounding cells, so it's difficult to tell them apart. But researchers have developed an interesting way to identify them by "lighting them up." All cells have unique proteins on their surface called receptors. Receptors bind chemical messages from other cells as part of cell-to-cell communication. Researchers use these receptors -- or markers -- to identify and isolate adult stem cells by "tagging" the chemical messages that bind to those specific receptors on the stem cell with fluorescent molecules. Once the fluorescent chemical message binds to the receptor on the surface of the stem cell, the stem cell will "light up" under fluorescent light. The "lighted" stem cell can then be identified and isolated. Like embryonic stem cells, adult stem cells can be grown in culture to establish stem cell lines. Adult stem cells were once believed to be more limited than embryonic stem cells, only giving rise to the same type of tissue from which they originated. But new research suggests that adult stem cells may have the potential to generate other types of cells, as well. For example, liver cells may be coaxed to produce insulin, which is normally made by the pancreas. This capability is known as plasticity or transdifferentiation It used to be believed that there were only two types of stem cells -- embryonic and adult -- but there's another kid on the stem cell block. Keep reading to learn about this "new" type: the induced pluripotent stem cell. Using Stem Cells to Treat Disease The first step in using stem cells for disease treatment is to establish stem cell lines, which researchers have accomplished. Next, scientists must be able to turn on specific genes within the stem cells so that the stem cells will differentiate into any cell they wish. But scientists have not learned how to do this yet; so, studying stem cell differentiation is an active area of research. Once scientists can create differentiated cells from stem cells, then there are many possibilities for their use, such as drug testing and cell-based therapies. For example, let's say you want to test new drugs to treat heart diseases. Currently, new drugs must be tested on animals. The data from animal research must be interpreted and then extrapolated to humans prior to human clinical trials. But suppose you could test them directly on human heart cells. To do this, human stem cell lines could be treated to differentiate into human heart cells in a dish. The potential drugs could be tested on those cells and the data would be directly applicable to humans. This use could save vast amounts of time and money in bringing new drugs to market. Stem-cell-based therapies are not new. The first stem-cell-based therapy was a bone marrow transplant used to treat leukemia. In this procedure, the patient's existing bone marrow is destroyed by radiation and/or chemotherapy. Donor bone marrow is injected into the patient and the bone marrow stem cells establish themselves in the patient's bones. The donor bone marrow cells differentiate into blood cells that the patient needs. Often, the patient must take drugs to prevent his or her immune system from rejecting the new bone marrow. But this procedure uses existing hemopoietic stem cells. How would you use stem cell lines? Let's look at how stem cells might be used to treat heart failure. Ideally, to treat a failing heart, scientists could stimulate stem cells to differentiate into heart cells and inject them into the patient's damaged heart. There, the new heart cells could grow and repair the damaged tissue. Although scientists cannot yet direct stem cells to differentiate into heart cells, they have tested this idea in mice. They have injected stem cells (adult, embryonic) into mice with damaged hearts. The cells grew in the damaged heart cells and the mice showed improved heart function and blood flow. In these experiments, exactly how the stem cells improved heart function remains controversial. They may have directly regenerated new muscle cells. Alternatively, they may have stimulated the formation of new blood vessels into the damaged areas. And the new blood flow may have stimulated existing heart stem cells to differentiate into new heart muscle cells. These experiments are currently being evaluated. One major obstacle in stem cell use is the problem of rejection. If a patient is injected with stem cells taken from a donated embryo, his or her immune system may see the cells as foreign invaders and launch an attack against them. Using adult stem cells or IPSCs could overcome this problem somewhat, since stem cells taken from the patient would not be rejected by his or her immune system. But adult stem cells are less flexible than embryonic stem cells and are harder to manipulate in the lab. And IPSC technology is too new for transplantation work. Finally, by studying how stem cells differentiate into specialized cells, the information gained can be used to understand how birth defects occur and possibly, how to treat them. Stem Cell Research Controversy Stem cell research has become one of the biggest issues dividing the scientific and religious communities around the world. At the core of the issue is one central question: When does life begin? At this time, to get stem cells that are reliable, scientists either have to use an embryo that has already been conceived or else clone an embryo using a cell from a patient's body and a donated egg. Either way, to harvest an embryo's stem cells, scientists must destroy it. Although that embryo may only contain four or five cells, some religious leaders say that destroying it is the equivalent of taking a human life. Inevitably, this issue entered the political arena. In 1996, Congress passed a rider to the federal appropriations bill called the Dickey-Wicker amendment. Representatives Jay Dickey and Roger Wicker proposed banning the use of federal monies for any research in which a human embryo is created or destroyed. Federal monies are a primary source of funding for stem cell research. The amendment has been renewed every year since that time. In 2001, President George W. Bush further restricted federal stem cell research. In an executive order, Bush stated that federal funds could only be used for research on human embryonic stem cell lines that had already been established (only 22 cell lines). This prevented researchers from creating more embryonic stem cell lines for research. In 2009, President Barack Obama issued an executive order to expand embryonic stem cell research. Obama's administration allowed federal funding of embryonic stem cell research if the following conditions applied: The cell line was one of the 22 in existence during the Bush administration or was created from embryos that had been discarded after in vitro fertilization procedures. The donors of the embryos were not paid in any way. The donors clearly knew that the embryos would be used for research purposes prior to giving consent. According to the administration, the new policy did not violate the Dickey-Wicker amendment because the money did not finance the creation of new embryos (they had already been created by private means) and did not finance the destruction of them. In 2009, two researchers from Boston, Dr. James Sherley of the Boston Biomedical Research Institute and Dr. Theresa Deisher of the Ava Maria Biotechnology Company, and other agencies filed a lawsuit against the government. Initially, the lawsuit was dismissed because the judge ruled that the plaintiffs had no legal standing (i.e. they were not affected materially by the new rules). However, a court of appeals overturned the initial ruling. The two scientists remained plaintiffs. The scientists claimed that, because they used adult stem cells exclusively in their research, the new rules would increase competition for federal research dollars, thereby affecting their ability to obtain funding. Federal Judge Royce Lamberth upheld the appeals court ruling. He placed an injunction preventing the new rules from going into place. He claimed that the rules violated the Dickey-Wicker amendment because embryos must be destroyed in the process of creating embryonic stem cell lines. In September 2010, The New York Times reported that the U.S. Court of Appeals ruled that federal funding of embryonic stem cell research could continue under the new rules while the court considers Judge Lamberth's ruling [source: New York Times]. This ruling allows researchers to continue feeding embryonic stem cell cultures, experimenting with mice, and other research activities until this court rules, the U.S. Supreme Court weighs in, or Congress passes legislation that clarifies the issues. In the meantime, stem cell research and the careers of stem cell researchers hang on a legal roller coaster. Although stem cells have great potential for treating diseases, much work on the science, ethical and legal fronts remains.