2_Circulatory System - V14-Study
advertisement

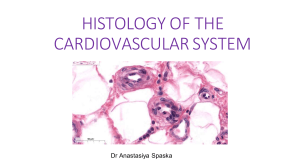
Cardiovascular System - - Basic circulation High pressure low pressure Function o Delivers blood o Exchanges oxygen, metabolites, wastes Cardiovascular system o Transport of blood throughout body Pulmonary circuit - Carries blood from the right side of the heart to the lungs Systemic circuit - Carries blood from left side of heart to all organs of the body Lymphatic vascular system o Adjunct to blood vessels o Collects extracellular tissue fluid and returns it to the cardiovascular system o Picks up protein/lipids from GI tract o Lymph Thin, watery, and relatively cell-free Flow is unidirectional, only moving away from tissue toward large veins (internal jugular and subclavian) o Involved in immune function o Examples Thoracic duct Right lymphatic trunk Structure of the heart Chamber walls o Cardiac musculature Cardiac skeleton o Fibrous, cartilaginous or osseous o Provides framework against which cardiac muscle contracts o 3 parts Annuli fibrosi - 4 fibrous rings from which valve leaflets originate - Provide support for the valves Trigona fibrosa - 2 structures that join the annuli fibrosi rings - Support myocardium and valves - One between each of the atria and ventricles - Composition is species specific Dense CT Dog (fibrocartilage) Horse (hyaline cartilage) Cow (bone) os cordis consists of 2 bones Membranous septum - Membranous part of the interventricular and interatrial septa “Membranous” = CT membrane - Valves o o o o o AV bundle of cardiac conduction system pierces cardiac skeleton near membranous septum and descends into the septum One-way flow Attach to fibrous, cartilaginous, osseous supports at heart base Typically avascular (except at base) Endothelium covers both sides 3 layers (superficial deep) Spongiosa - Loose CT, elastic CT, proteoglycans - On side that faces atria or blood vessel (pulmonary artery or aorta) - Acts as shock absorber and confers flexibility Fibrosa - Fibrous extensions of os cordis or collagenous support (core of valve) Ventricularis - Dense CT (more collagen) - On side adjacent to ventricles Impulse conduction system o Autorhythmicity Intrinsic rhythmicity generates a pacemaker potential Contraction synchronized by special electrically-active fibers - Origin of electrical activity (primary pacemaker) SA (sinoatrial) node - Electrical activity passes from cell to cell along internodal tracts AV (atrioventricular) node Only electrical connection between atria and ventricles Bundle of His Purkinje fibers Heart DOES NOT require nerve/hormone input to beat Development of the heart The heart is a tubular organ that arises during development as a primary tube that folds o Typical tubular organs have 3 major layers o Size of each layer is determined by function, genetics, environment (physical forces) 3 layers (deep superficial) o Endocardium Epithelial layer - Endothelium is the single-cell epithelial layer that lines heart - There is an epithelial layer that lines vessels of cardiovascular system Deeper layer (subendocardial layer) - Subendocardial CT - Continuous with myocardium connective tissue - Contains conduction system Purkinje fibers Lots of glycogen Conduct impulses 4x faster than cardiac muscle cells Function - Integrity - Impulse conduction o Myocardium Cardiac muscle of heart wall Wall structure reflects local forces ( pressures in atria, pressures in ventricles) - Thin myocardium in right atrium (RA) - Thick myocardium in right ventricle (RV) - Anastomosing network of myofibers - Striated, short, branched myofibers - Intercalated discs - Nuclei visible in each fiber - “Spongy appearance” Gap junctions - Allows the cardiac action potential to propagate from cell to cell through a low-resistance pathway Continuous, non-fenestrated capillaries is CT between muscle fibers Function - Contraction o Epicardium (visceral pericardium) Outer surface - Mesothelial cells (“visceral mesothelium”) Flat, simple squamous Primary function is to provide slippery, protective surface Metabolically active Involved in protection/healing Become cuboidal/round during pathological processes Inner surface - Fibrous CT, blood vessels, nerves, adipose tissue (varies in thickness) Function - Homeostasis - Protection of the heart o Pericardium Fibrous pericardium (outer) - Continuous with mediastinum Serous pericardium (inner) - Parietal layer - Visceral layer (continuous with epicardium) - Lined by mesothelial cells - Pericardial fluid Between visceral and parietal layers Lubricates and allows heart to move freely in pericardial cavity General structure of blood vessels 3 layers (deep superficial) o Tunica intima Simple, squamous endothelium attached to basil lamina Subendothelial CT cushion Occasional smooth muscle cells Internal elastic lamina (hard to see in smaller arteries) - Defines outer edge of intima - More prominent than external elastic lamina Functions - Regulates permeability of vessel wall by control of cell-cell junctions and transcellular transport in endothelium Tight junctions of large arteries maintain pressure (NO leakage) Lack of tight junctions in glomerulus of kidney, where endothelial cells are responsible for allowing filtration of blood - Production of various active compounds o Tunica media Helically-arranged layers of smooth muscle Collagenous/elastic/proteoglycan CT (extracellular matrix) - - - Can histologically differentiate b/w elastic and smooth muscle fibers by looking at cell nuclei, which are plump, elongated, and actively euchromatic, while those of elastic CT are more darkly-stained fibroblasts Functions - Regulates vessel compliance Number of elastic fibers Contractile state of smooth muscles o Tunica adventitia Longitudinally-arranged CT Predominant cell type is fibroblasts External elastic lamina In large vessels, this layer will be pierced with vessels (vasa vesorum) because blood supply from inner layer/lumen cannot migrate huge distances to supply nutrients to the tunica adventitia Function - Cushioning/protection via adipocytes - Avenue for neural regulation (nervi vascularis) of vessel wall Specific blood vessel structure Structure of vessels adapts to function o Pressure gradients create structural variation Pumping action of heart Movement of muscles Gravity Arteries Elastic arteries (large) o Walls contain multiple sheets of elastic lamellae Internal and external elastic membranes are indistinguishable because there are elastic fibers everywhere o Expand and recoil to allow for smoother flow o Aorta, pulmonary arteries, subclavian Muscular arteries (medium) o Thin, undulating tunica intima o Prominent tunica media More smooth muscle, less elastin o Internal elastic lamina is prominent o Brachial, anterior tibial, coronary arteries Small arteries o 8-10 smooth muscle layers o Contain an internal elastic lamina o Tunica adventitia merges with surrounding CT Arterioles o Only 1-2 layers of smooth muscle o Not going to see internal elastic lamina o Regulate blood flow into the capillary beds Slight thickening before capillary bed is precapillary sphincter Amount of blood that enters capillary bed depends on constricted or dilated nature of arterioles Veins ~60% of blood volume found in veins Travel with like-sized arterial vessels Comparison to arteries o Tunics not as distinct, distorted border, thinner walls, larger lumen o Less muscle, more adventitia - Large veins o Travel with elastic arteries o Diameter > 10mm o Tunica media is thin o Tunica adventitia is thickest layer o Vena cava, jugular, pulmonary, portal, renal Medium veins o Travel with medium/muscular arteries o Diameter up to 10mm o Contain valves o 3 tunics are evident Small veins o Diameter up to 1mm o 2-3 muscle layers o Thin tunica media o Contain valves Postcapillary venules o Receive blood from capillary beds o Structure similar to capillary, but wider lumen o Diameter 0.2-0.5 mm o CT, pericytes o No true tunica media (no muscle) o Endothelium Fewer cell junctions Target of vasoactive agents o Important in inflammatory response and emigration of leukocytes Cause clinical signs associated with inflammatory reaction Vein specialization o Valves Especially found in large veins of the distal limb Hydrostatic pressure poses problems for return of blood to heart, particular from the legs. Veins have valves to prevent backflow. Tissue and muscle also pump to assists in blood return, especially when fighting gravity (from distal limbs) Capillary beds Provide optimal environment for exchange of nutrients, gases, waste products Density of network determines the total SA available for exchange and is directly related to the metabolic activity of the tissue (liver, kidney, cardiac tissue have rich capillary networks) Organization Interconnecting network of collateral arteries feeding arterioles o Metarterioles Involved with AV shunts - Involved in thermoregulation (skin) When hot, shunt closed, and transport into capillary bed When cool, shunt open, bypass transport to capillary bed More smooth muscle around them acts as sphincter “Gate keepers” that regulate blood flow to either capillary bed or shunt o Capillaries Lined by single endothelial cell with blood cell in lumen Continuous capillaries - Tight junctions between cells - Regulate exchange of material across vessel Active transport, pinocytosis, receptor-mediated endocytosis - Found in microcirculatory systems Muscle, lung, CNS, lung Fenestrated capillaries - Semipermeable, selectively-permeable - Fenestrations (holes) in wall of capillary - Kidney glomerulus, GI tract (want to absorb nutrients), small intestine, gall bladder, hypothalamus, endocrine cells, choroid plexus Sinusoidal capillary - Larger pores between endothelial cells - Basal lamina is discontinuous (porous) - Allows for rapid passage of fluid, macromolecules, and cells - Spleen (RBCs can freely move through capillaries), liver, bone marrow Pericytes Located between endothelial cell and basal lamina Undifferentiated - May be involved in angiogenesis - Can transform into smooth muscle or fibroblasts Venules o - o Portal system Two capillary beds linked by portal vein o Liver, pituitary Lymphatics Travel with blood vessels Unidirectional o Only carry lymph from tissues to heart o Have valves to promote unidirectional flow Very thin-walled o More permeable than blood capillaries o Carry protein-rich fluids, lipids, lymphocytes Lymphatic capillaries o Begin as blind-ended tubes o Endothelium o Incomplete basal lamina More permeable than blood capillaries o Carry protein-rich fluids, lipids, lymphocytes o NO red cells Lymphatic vessels o Larger than lymphatic capillaries o Punctuated by lymph nodes o Can contract, but never with the strength of an artery o Valves o Drain into large veins (internal jugular, subclavian) o Thoracic duct (largest)