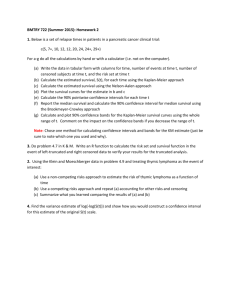
Peds 814 combined document 1.20.15
advertisement

Peds 814: In infants and children during cardiac arrest (P), does the presence of any specific intra-arrest prognostic factors (I), compared with the absence of these factors (C), change survival to 180 days with good neurological outcome, survival to 60 days with good neurological outcome, survival to hospital discharge with good neurological outcome, survival to 30 days with good neurological outcome, Survival only at discharge, 30 days, 60 days, 180 days AND/OR 1 year (O)? Summary of evidence: No randomized clinical trials were found. The initial search strategy (detailed in SEERS) generated 6476 abstracts. After screening the papers from the search strategy and excluding repeated studies, studies done in another language than English, studies with mixed adult and pediatric populations or OOHCA and IHCA when the data could not be analyzed separately, publications before the year of 2000 (guidelines then were different) and papers that reported exclusively cases with trauma, drowning populations or SIDS (these are populations with known different prognostics related to cardiac arrest): 22 papers were reviewed to determine which intra-arrest prognostic factors could be assessed from the published data. Therapeutic interventions were not reviewed as part of this work, as a number of these were assessed in other PICO questions. Duration of CPR, age, and initial arrest rhythm were selected as being most amenable to assessment from published data. We selected 5 studies for out of hospital cardiac arrest (OOHCA), one of the studies was determined to be not applicable to the PICO question and was excluded after assessment of risk of bias. 1. 2. 3. 4. 5. Young2004 157. Subsequent analysis of randomized study comparing airway interventions in OOHCA, 601 patients, data from 1994-97 (older CPR guidelines with different compression:ventilation ratios). Setting: USA. Subjects: age < 12 years or smaller than 40kg. Total number of cases: age: 601/601; rhythm: 548/601; duration: not available (NA); survival to discharge: 596. No multivariate analysis performed. For survival to discharge, shorter CPR duration and older age were associated with survival. Lopez-Herce2005 807. Reanalysis of a published 2004 report limiting data to OOHCA, Observational study of 95 children with respiratory arrest or OOHCA, data from 1998-1999. Setting: multicenter in Spain. Subjects: age: 7 days to 16 years. Total number of cases: age: 95/95; rhythm: 83/95; duration: 94/95, 78 had cardiac arrest. Outcomes of survival to discharge and one year survival were not available for all factors selected. Multivariate analysis showed best predictor of mortality was duration of resuscitation of > 20 minutes. Mortality was higher for infants. Mortality was higher for asystole, PEA, and slow rhythms vs. VF. Tham2005 289. Retrospective study of OOHCA, 85 patients with only 4 survivors. Setting: Single center in Singapure. Subjects: does not define age group for “children.” Only significant finding was shorter duration of CPR associated with survival. This non-RCT was not included on our GRADE evaluation due to the imprecision of definitions, missing data, and very low number of survivors making comparison between groups problematic. Atkins2009 1484. Prospective observation study from Resuscitation Outcomes Consortium, from 2005-2007. Setting: Multicentric USA and Canada. Subjects: age less than 20 years with OOHCA; trauma excluded. Total of 624 patients, not all data available for all patients: age: 621/624; rhythm: 469/624; duration: not available (NA). Age > 12 months was associated with survival; VF/VT rhythm was associated with survival compared to combined PEA/asystole. Moler2011 141. Retrospective analysis of OOHCA data collected for future hypothermia trial from 2003 to 2004. Setting: 15 sites PECARN. Subjects: ages: 24 hours to 18 years. Total of 138 patients, but not all data available for all variables for selected variables: age: 137/138; rhythm: 138/138; duration: 69/138. Patients were less likely to survive is they had non-VF rhythms or had longer duration of CPR. Moderate/large effect size Publication bias Study Limitations Imprecision Number of participants Indirectness Potential prognostic factor Odds Ratio (95% Number of confidence studies interval) Inconsistentency Potential Prognostic Factor: Age Overall quality Survival to discharge (Important) Very low Age > 1 year (Young2004) 601 1A Non-RCT 1.3 (0.8 -2.1) Very SeriousB Not Not Serious Serious Not Not Serious Serious Age > 1 year (Atkins2009) 621 1C Non-RCT 2.7 (1.3-5.7) Not serious Not Not Serious Serious SeriousD Not Serious Low Moderate ⨁⨁◯◯ effect size Age > 1 year (Moler2011) 137 1E Non-RCT 1.4 (0.8-2.4) Very SeriousF Not Not Serious Serious SeriousG Not Serious No A: Young2004 157. No control for confounders and data from 1994-1997. C: Atkins2009 1484. D: Wide confidence interval. E: Moler2011 141. F: No control for confounders and data from 2003-2004. G: Small number of events. B: No ⨁◯◯◯ Very low ⨁◯◯◯ Moderate/large effect size Publication bias Imprecision Number of participants Indirectness Potential prognostic factor Relative Risk (95% Number of confidence Study studies interval) Limitations Inconsistentency Potential Prognostic Factor: Rhythm Overall quality Survival to discharge (Important) Very low VF/VT compared to Asystole/PEA 548 (Young2004) 1H Non-RCT 1.3 (0.5-3.0) Very SeriousI Not Not Serious Serious Not Not Serious Serious VF/VT compared to Asystole/PEA 417 (Atkins2009) 1J Non-RCT 4.0 (1.8-8.9) SeriousK Not Not Serious Serious SeriousL Not Serious Moderate Very low effect size ⨁◯◯◯ VF/VT compared to Asystole/PEA 91 (Moler2011) 1M Non-RCT 2.7 (1.3-5.6) Very SeriousN Not Not Serious Serious SeriousO Not Serious Moderate Very low effect size ⨁◯◯◯ H: No ⨁◯◯◯ Young2004 157 No control for confounders and data from 1994-1997. J: Atkins2009 1484. K: Loss of follow up in 156 cases out of 624 (25%) and rhythm not determined in 51 subjects (more than the total number of subjects in the VF/VT group). L: Large confidence interval. M: Moler2011 141. N: No control for confounders and data from 2003-2004. Asystole at any time during the arrest was more common in nonsurvivors than in survivors (67% vs 26%, p<0.01). O: Small number of events and wide confidence interval. I: Moderate/large effect size Publication bias Imprecision Number of participants Indirectness Potential prognostic factor Relative Risk (95% Number of confidence Study studies interval) Limitations Inconsistentency Potential Prognostic Factor: Duration of Resuscitation Overall quality Survival to discharge (Important) Young2004 157 601 Non-RCT Moler2011 141 138 Non-RCT 63 1S Non-RCT Survivors: median 16 (IQR 1030)min, nonsurvivors: median 36 (29-48)min.P Survivors: median 18.5 (3.5-28.5)min and nonsurvivors: 41 (24-54) min. p<0.01 Very SeriousQ Not Not Serious Serious Very SeriousR Not Not serious Serious Very SeriousT Not Not Not serious SeriousU Serious Serious Very Low NA Not Serious NA NA Not Serious NA ⨁◯◯◯ Very Low ⨁◯◯◯ Survival 1 year (important) Duration < 20 minutes (Lopez-Herce2005) 6.6 (2.9-14.9) Large Very low ⨁◯◯◯ P: Not statistically significant. Longest duration of CPR in a survivor: 56 minutes, longest duration of CPR in a survivor with good neurologic outcome 42 minutes (31 minutes of CPR in ED and 11 minutes before hospital arrival). Q: No control for confounders and data from 1994-1997. R: 50% loss of follow up for the duration of resuscitation data (information on 69 subjects). S: Lopez-Herce2005 807. T: Lopez-Herce2005 807 included both respiratory and cardiac arrests and data is from 1998-1999. U: Small number of events, large confidence interval. Consensus on Science For the important outcome of survival to discharge in OOHCA, we found one low quality observational study (Atkins 2009:1484; 621 OOHCA subjects, downgraded for serious imprecision and upgraded for moderate effect size) that found that age >1 year was significantly associated with improved outcome (Relative Risks 2.7(1.3-5.7). Two very low quality observational studies (Young 2004:157; 601 OOHCA subjects, downgraded for very serious risk of bias) (Moler 2011:141; 137 OOHCA subjects, downgraded for very serious risk of bias and serious imprecision) showed an insignificant trend toward improved outcomes in patients >1 year (Relative Risk: Young 1.3 (0.8-2.1), Moler 1.4 (0.8-2.4) For the important outcome of survival to discharge, we found two very low quality observational studies (Atkins 2009:1484, 417 OOHCA subjects, downgraded for serious risk of bias and serious imprecision and upgraded for moderate effect size) (Moler 2011:141, 91 OOHCA subjects, downgraded for very serious risk of bias and serious imprecision and upgraded for moderate effect size) that found VF/VT as an initial rhythm was significantly associated with improved outcome compared to the combined rhythm group of PEA/asystole with Relative Risks of: Atkins 4.0(1.8-8.9) and Moler 2.7 (1.3-5.6). One observational study (Young 2004:157; 548 OOHCA subjects, downgraded for very serious risk of bias) demonstrated a trend toward improved survival in the VF/VT group that did not achieve statistical significance (Relative Risk 1.3(0.5-3.0)). For the important outcome of survival to discharge and survival to one year we have identified very low quality evidence from three observational studies (Young 2004:157; 601 OOHCA subjects, downgraded for very serious risk of bias) (Moler 2011:41; 138 OOHCA subjects, downgraded for very serious risk of bias) (Lopez-Herce 2005:807, 63 OOHCA subjects, downgraded for very serious risk of bias and serious imprecision and upgraded for large effect size) showing a higher likelihood of survival with shorter duration of CPR. CPR for less than 20 minutes was associated with improved one year survival in one study (Relative Risk 6.6; CI 2.9-14.9, Lopez) while median durations of 16 (IQR 10-30) and 19 (IQR3.5-28.5) minutes were associated with survival to hospital discharge in two studies (Young, Moler). We did not identify enough evidence to address the critical outcomes of survival to 180 days with good neurological outcome, survival to 60 days with good neurological outcome, survival to hospital discharge with good neurological outcome. We did not identify enough evidence to address the important outcomes of survival only at 30 days, 60 days, 180 days nor survival to 30 days with good neurological outcome. Treatment Recommendation For pediatric patients in OOHCA treated with standard CPR (without extracorporeal rescue), the published data are so limited in number and quality that confidence in effect estimates is very low. As a result, the task force feels that any recommendation to identify a maximum length for attempted CPR is speculative. Knowledge gaps Large prospective studies correlating risk factors to event survival and longer-term survival, particularly with neurological outcomes, are needed to predict successful resuscitation for children in OOHCA and guide decisions on termination of resuscitation. Studies need to be performed in time frames that maintain similar resuscitation protocols to reduce the risk of bias from changing treatment strategies.