PHT 312-lab notes (l..
advertisement
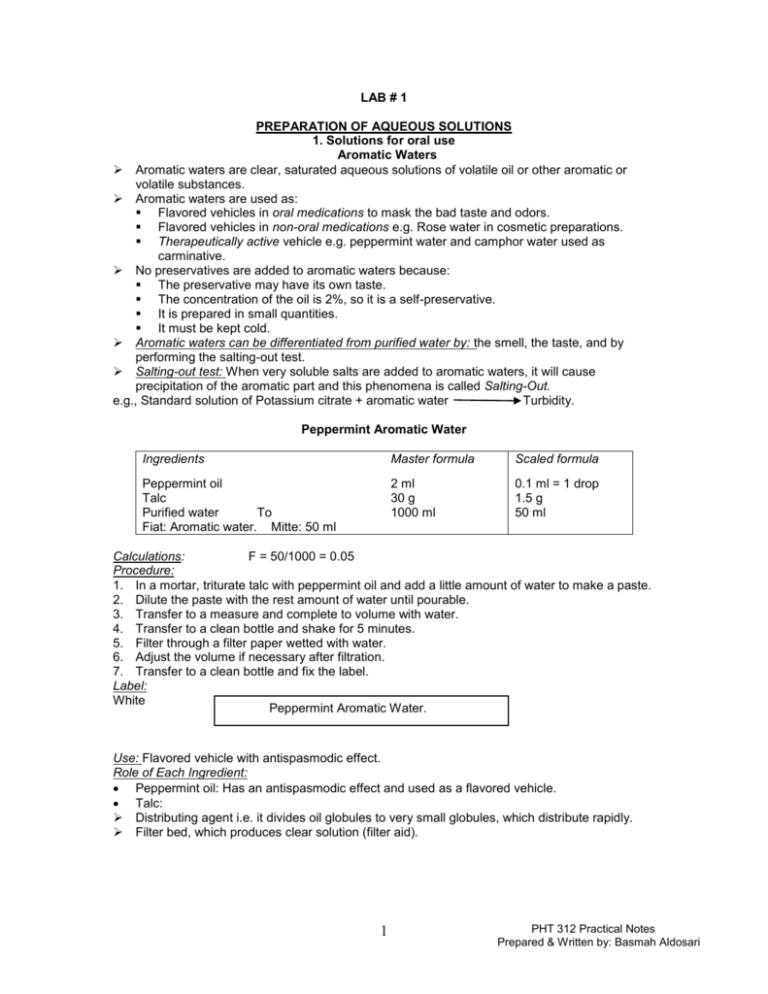
LAB # 1 PREPARATION OF AQUEOUS SOLUTIONS 1. Solutions for oral use Aromatic Waters Aromatic waters are clear, saturated aqueous solutions of volatile oil or other aromatic or volatile substances. Aromatic waters are used as: Flavored vehicles in oral medications to mask the bad taste and odors. Flavored vehicles in non-oral medications e.g. Rose water in cosmetic preparations. Therapeutically active vehicle e.g. peppermint water and camphor water used as carminative. No preservatives are added to aromatic waters because: The preservative may have its own taste. The concentration of the oil is 2%, so it is a self-preservative. It is prepared in small quantities. It must be kept cold. Aromatic waters can be differentiated from purified water by: the smell, the taste, and by performing the salting-out test. Salting-out test: When very soluble salts are added to aromatic waters, it will cause precipitation of the aromatic part and this phenomena is called Salting-Out. e.g., Standard solution of Potassium citrate + aromatic water Turbidity. Peppermint Aromatic Water Ingredients Master formula Scaled formula Peppermint oil Talc Purified water To Fiat: Aromatic water. Mitte: 50 ml 2 ml 30 g 1000 ml 0.1 ml = 1 drop 1.5 g 50 ml Calculations: F = 50/1000 = 0.05 Procedure: 1. In a mortar, triturate talc with peppermint oil and add a little amount of water to make a paste. 2. Dilute the paste with the rest amount of water until pourable. 3. Transfer to a measure and complete to volume with water. 4. Transfer to a clean bottle and shake for 5 minutes. 5. Filter through a filter paper wetted with water. 6. Adjust the volume if necessary after filtration. 7. Transfer to a clean bottle and fix the label. Label: White Peppermint Aromatic Water. Use: Flavored vehicle with antispasmodic effect. Role of Each Ingredient: Peppermint oil: Has an antispasmodic effect and used as a flavored vehicle. Talc: Distributing agent i.e. it divides oil globules to very small globules, which distribute rapidly. Filter bed, which produces clear solution (filter aid). 1 PHT 312 Practical Notes Prepared & Written by: Basmah Aldosari 2. Solutions for use in the mouth and throat Mouthwashes These are aqueous solutions used to treat conditions of the mouth and to clean and refresh the buccal cavity. The active ingredients are usually antiseptic or bactericidal agents in a pleasantly flavored vehicle. Mouthwashes are similar to gargles (aqueous solutions used to treat infections of the throat). They are often presented in concentrated form with instructions to the patient for dilution with warm water before use. Compound sodium chloride mouthwash BP Ingredients Master formula Scaled formula Sodium chloride Sodium bicarbonate Conc peppermint emulsion Double strength chloroform water Water To Fiat: Mouthwash. Mitte: 50 ml Sig.: 15 ml to be diluted with equal volume of warm water BID. 1.5 g 1g 2.5 ml 50 ml 100 ml 0.75 g 0.5 g 1.25 ml 25 ml 50 ml Ref: pharmaceutical practice (Winfield & Richards), pp. 189-190 Calculations: F = 50/100 = 0.5 Amount of vehicle = 50 – (25+1.25) = 23.75 ml of water Procedure: 1. Weigh the solids on a suitable balance. 2. In a beaker or conical measure, dissolve the solids in about 2/3rd the vehicle. 3. Add the double strength chloroform water & concentrated peppermint emulsion, mix. 4. Make up to volume with water. 5. Pack in an amber ribbed bottle with a child – resistant closure, and label. Label: Red Compound Sodium Chloride Mouthwash BP One tablespoonful to be diluted with equal volume of warm water and used twice daily. Name: Date: Use: for cleansing and freshening the mouth. Role of Each Ingredient: Conc peppermint emulsion: is a flavoring agent. Double strength chloroform water: is a sweetener and preservative. Sodium chloride is soluble 1 in 3 of water, and sodium bicarbonate is soluble 1 in 11 of water. Additional information: Concentrated peppermint emulsion (BP): peppermint oil 2 ml, polysorbate ‘20’ 0.1 ml, double strength chloroform water 50 ml, freshly boiled and cooled water to 100 ml. Double strength chloroform water (BP): chloroform 0.5% v/v in freshly boiled and cooled water. 2 PHT 312 Practical Notes Prepared & Written by: Basmah Aldosari LAB # 2 Preparation of Non aqueous solutions Non aqueous solutions are prepared in non aqueous solvents for either internal or external use. Preparations for internal use may contain solvents such as ethanol, glycerin, propylene glycol, certain oils, and liquid paraffin. Preparations for external use may contain additional solvents such as isopropyl alcohol, polyethylene glycols, various ethers, and certain esters. Solvents such as acetone, benzene and petroleum ether are not used for internal products. Non aqueous solutions include: 1. The alcoholic or hydroalcoholic solutions (e.g., elixirs and spirits), 2. Ethereal solutions (e.g., collodions), 3. Glycerin solutions (e.g., glycerins), 4. Oleaginous solutions (e.g., liniments, oleovitamins, and toothache drops), 5. Inhalations and inhalants. Elixirs: Are clear, pleasantly flavored, sweetened hydroalcoholic liquids for oral use. They are used as flavors and vehicles for drug substances, such as Aromatic elixir USP; when drugs are incorporated into the specified solvents, they may be classified as medicated elixirs, e.g., Dexamethasone Elixir USP & Phenobarbital Elixir USP. Elixirs are more fluid than syrups due to the use of less viscous ingredients such as alcohol and the minimal use of viscosity improving agents such as sucrose. The main ingredients in elixirs are ethanol and water, but glycerin, sorbitol, propylene glycol, flavoring agents, preservatives, and syrups are often used in the preparation of the final product. An elixir may contain water and alcohol soluble ingredients. Ingredients Phenobarbitone Elixir Master formula Scaled formula Phenobarbitone 400 mg 200 mg Ethanol 90% 40 ml 20 ml Compound orange spirit 2.5 ml 1.25 ml Glycerol 40 ml 20 ml Amaranth solution 1ml 0.5 ml Water to 100 ml 50 ml Fiat: elixir Mitte: 50 ml Sig.: 10 ml to be given at night. Ref: pharmaceutical practice (Collet & Aulton), pp. 87-97 Calculations: F = 50/100 = 0.5 Amount of water = 50 – (20+20+1.25+0.5) = 8.25 ml Procedure: 1. In a small beaker, dissolve phenobarbitone in ethanol. 2. Add compound orange spirit, glycerol, amaranth solution, and part of the vehicle. 3. Transfer to a cylinder. 4. Make up to volume with water. Use: anticonvulsant. Label: White Phenobarbitone Elixir Two teaspoonfuls to be given at night Name: Date: Role of Each Ingredient: 1. Phenobarbitone: active ingredient, anticonvulsant. 3 PHT 312 Practical Notes Prepared & Written by: Basmah Aldosari 2. Ethanol & Glycerin: co-solvents. 3. Compound orange spirit: flavoring agent. 4. Amaranth solution: colouring agent. Advice for patients when dispensed: Phenobarbitone causes drowsiness. Anticonvulsant therapy should not be discontinued without medical advice. Liniments Are solutions or mixtures of various substances in oil, alcoholic solutions of soaps, or emulsions and intended for external application. They are applied with rubbing to the affected area, the oil or soap base provide ease of application and massage. Alcoholic liniments are used generally for their rubefacient and counterirritant effects. Such liniments penetrate the skin more readily than do those with an oil base. The oily liniments are milder in their action and may function solely as protective coatings. Liniments should not be applied to skin that are bruised or broken. Rubefacient: A substance for external application that produces redness of the skin e.g. by causing dilation of the capillaries and an increase in blood circulation. Counterirritant: A medicine applied locally to produce superficial inflammation in order to reduce deeper inflammation. Zinc Oxide Liniment Ingredients Zinc oxide Talc Alcohol 70% Glycerin aa Water Fiat: Liniment Mitte: 50 g Sig.: Ut dict. Master formula Scaled formula 12.5 g 50 g 6.25 g 25 g Calculations: F = 50/100 = 0.5 Volume of alcohol = wt / sp.gr = 6.25/1 = 6.25 ml Volume of glycerin = wt / sp.gr =6.25/1.25 = 5 ml Volume of water = 25/1= 25 ml Procedure: 1. In a mortar, levigate zinc oxide and talc with glycerin until a smooth paste is formed. 2. Dilute with alcohol and ½ amount of water until pourable. 3. Transfer to a measure; rinse the mortar with the rest amount of water. 4. Transfer to a clean bottle and fix the label. Labeling: Shake the Bottle Before Use Red Zinc Oxide Liniment To be used as directed Name: Date: Uses: protective against sunburns. Role of Each Ingredient: o Zinc oxide: astringent. o Talc: adsorbent for secretions. o Alcohol: antiseptic. o Glycerin: humectant 4 PHT 312 Practical Notes Prepared & Written by: Basmah Aldosari Characteristics of a good external liquid formulation: 1. Esthetic appearance. 2. Stable formulation (permanent color, and absence of sedimentation). 3. Uniform distribution of active ingredients. 4. Ease of spreading and penetration. 5. Release and availability of medication either rapidly or over a prolonged time on extended contact with dermatomucosal surfaces 5 PHT 312 Practical notes LAB # 3 Preparation of aqueous solutions with incompatibilities (1) Definition: Incompatibility occurs when the components of a medicine interact in such a way that the properties of that medicine are adversely affected. Incompatibility may be detected by changes in the physical, chemical and therapeutic qualities of the medicine. Such changes may affect the safety, efficacy, and appearance of the medicine. Types: therapeutic or pharmaceutical. Therapeutic incompatibility, (drug-drug interaction), arises when a medicine contains two or more antagonistic substances, the effect of which counteract or enhance each other, or when the action of one component in the body affects the action of another component. For example, a medicine containing an expectorant and a cough suppressant drug. Pharmaceutical incompatibility arises when the components of the medicine interact either physically or chemically to give an unsuitable product. Physical incompatibilities: may occur due to physical interactions among ingredients. Types of physical incompatibilities: 1. Incomplete solution: due to wrong or insufficient solvent or vehicle. 2. Immiscibility: e.g., oil + alcohol separation. 3. Precipitation: E.g., acacia mucilage and water form a solution, but when alcohol is added, precipitation occurs. 4. Liquification of the solid product: mixture of solids may liquefy due to the formation of eutectic mixture or liberation of water. 5. Solidification of liquid products: e.g., when acacia solution gelatinize with ferric salts due to carboxylic group in the gum. How Does the Pharmacist Detect and Correct the Physical Incompatibility: I- Change the volume of solvent or change the solvent: 1- Mercuric iodide 195 mg Thymol 325 mg Purified water q.s. 30 ml Problem: Both Mercuric iodide and Thymol are not water soluble. To Solve Incompatibility: Replace water by alcohol. II- Change the form of ingredient Phenobarbital 0.195 g Sodium salicylate 14 g Purified water q.s. 30 ml Mitte: Solution Problem: Phenobarbital is insoluble in water. To Solve Incompatibility: Use Phenobarbital Sodium (salt), but you should add the amount correctly. Phenobarbital 1 g x g Phenobarbital Sodium. 1- III- Addition of filler or diluent Aminopyrine gr v Codiene So4 gr 1/4 Belladonna extract gr 1/6 Acetyl salicylic acid gr iii Problem: Eutectic mixture will be formed. 1- 6 PHT 312 Practical notes Eutectic mixture is a term used to describe the liquefaction of some solid substances when in close or prolonged contact with one another. These substances include phenol, menthol, camphor, thymol, aspirin, phenylsalicylate, phenacetin, and other similar chemicals. Therefore, powder prepared from such substances is commonly mixed in the presence of inert diluent such as light magnesium oxide or magnesium carbonate to separate physically the troublesome agents. (Ref: Introduction to Pharmaceutical dosage forms, By: Howard Ansel, p. 170 ). To Solve Incompatibility: Let eutectic mixture formed then add adsorbent (e.g. MgO or MgCO3) to adsorb the formed liquid and then store in tightly Stopperd container. OR Physically divide (Aminopyrine + Codiene SO4) in one capsule and (Belladonna extract + Acetyl salicylic acid) in another capsule. IV- Make an emulsion dosage form Sodium sulfate 5 gm Liquid paraffin 50 gm Cherry syrup q.s. 120 ml Problem: the Rx contains two immiscible liquids, liquid paraffin and cherry syrup. To Solve Incompatibility: add emulsifying agent e.g. acacia, Tween, or Span to formulate a stable emulsion. 1- VVI Make a suspension dosage form Change the dosage form If the ingredients cannot be dissolved or suspended, prepare it in solid dosage form (capsule). Chemical incompatibilities: usually occur as a result of chemical interaction among ingredients. It can be immediate upon compounding (effervescence, precipitation, or color change), or delayed (oxidation, reduction, hydrolysis). Types of chemical incompatibilities: 1. Oxidation: due to exposure to air, light, excessive storage temperature, over dilution, incorrect pH adjustment. E.g., adrenaline, noradrenaline, atropine, and morphine undergo oxidation. Oxidation can be corrected by: a. Use of antioxidants (ascorbic acid, sodium metabisulfite, EDTA). b. Avoid trace metal ions catalysis effects. 2. Reduction: is less common in prescriptions, e.g., Hg salts, Ag salts, and Gold salts are reduced into metallic form upon exposure to light. 3. Racemization: is the conversion of an optically active form to an optically inactive form without change in chemical constituents. Racemizarion usually results in reduced pharmacological activity, e.g., adrenalin, ephedrine. 4. Precipitation: e.g., mixing sodium salicylate with citric acid lead to precipitation of salicylic acid. 5. Change in color: e.g., phenolphthaline is colorless in acid medium but shows purple color in alkaline medium. 6. Evolution of gas: e.g, the reaction of an acid with carbonate releases CO2 effervescence. How Does the Pharmacist Detect and Correct the Chemical Incompatibility: I- Control the reaction e.g. Ammonium carbonate Ammonium chloride Dilute acetic acid Simple syrup q.s. 7 zi z ii Fl z ii Flz iv PHT 312 Practical notes Problem: reaction of Ammonium carbonate and Dilute acetic acid will lead to production of effervescence. To Solve Incompatibility: wait until effervescences pass. IIReplacing one of the reacting ingredient e.g. NH4 salicylate zi KHCO3 zi Peppermint water q.s. Flz vi Problem: NH4 salicylate + KHCO3 ammonia + k salicylate (dark color). To Solve Incompatibility: change to K salicylate or Na salicylate. Ingredients Sodium salicylate Syrup of lemon Examples of pharmaceutical incompatibilities Sodium salicylate solution Master formula Scaled formula (before correction) 5g 1.65 g 20 ml 6.6 ml Scaled formula (after correction) 1.65 g Simple syrup =6.27 ml Lemon tincture =0.33 ml 25 ml Aqua To 75 ml 25 ml Fiat: solution. Mitte: 25 ml Sig.: 5 ml TID Prepare the above prescription before and after correction of the incompatibility. Incompatibility problem: Problem: syrup of lemon contains citric acid, which would interact with sodium salicylate to form salicylic acid (insoluble) and citric acid. This interaction will lead to precipitation of salicylic acid (Chemical incompatibility). Sodium salicylate + Syrup of lemon Salicylic acid + Citric acid (insoluble) Correction: replace syrup of lemon (sweetening and flavouring agent) with simple syrup (sweetening agent) and lemon tincture (flavouring agent), to avoid precipitation of salicylic acid. Calculations: F = 25/75 = 0.33 Amount of water = 25 – 6.6 = 18.4 ml Amount simple syrup and lemon tincture: Total amount = 20 ml (19 ml simple syrup: 1 ml lemon tincture), then multiply by F: Therefore, total amount = 6.6 ml (6.27 ml simple syrup: 0.33 ml lemon tincture) Procedure: Before correction After correction 1. In a small beaker or conical measure, dissolve 1. In a small beaker or conical measure, dissolve sodium salicylate in ½ amount of water. sodium salicylate in ½ amount of water. 2. Add syrup of lemon, mix well. 2. Add simple syrup, mix well. Then add lemon 3. Transfer to a clean cylinder and make up to tincture. Mix. volume with rest amount of water. 3. Transfer to a clean cylinder and make up to volume with rest amount of water. Final product: suspension form, wrong prep. Final product: solution form, right prep. Label: White Sodium Salicylate Solution One teaspoonful to be taken three times daily Name: Date: Use: sodium salicylate has analgesic, anti-inflammatory and antipyretic properties similar to aspirin. Role of Each Ingredient: Sodium salicylate: active ingredient, analgesic, antiinflammatory and antipyretic. Simple syrup: sweetening agent. Tincture of lemon: flavouring agent. 8 PHT 312 Practical notes LAB # 4 Preparation of aqueous solutions with incompatibilities (2) Quinine HCl Suspension Ingredients Master formula Scaled formula Scaled formula (before correction) (after correction) Quinine HCl 1.3 g 0.43 g 0.43 g Sodium salicylate 8g 2.64 g 2.64 g Aqua q.s. ad 90 ml 30 ml 30 ml 2% acacia powder =0.6 g Fiat: suspension. Mitte:30 ml Sig.: 15 ml q6h. Prepare the above prescription before and after correction of the incompatibility. Problem: quinine HCl is soluble 1 in 23 ml of water, which is weak solubility. Therefore, a suspension will be formed. However, the suspended particles will settle rapidly and form cake sediment which is difficult to redisperse with shaking, i.e., Not true suspension. (Physical incompatibility). Correction: addition of 2% acacia as a suspending agent will decrease the rate of sedimentation of particles and help to form a true suspension. Calculations: F = 30/90 = 0.33 Amount of acacia powder = 2% x 30 = 0.6 g Procedure: Before correction 1. Weigh the required amount of quinine HCl, and then grind it into very fine powder in a mortar with pestle. 2. Add ½ amount of vehicle and mix well with the pestle. 3. Add amount of sodium salicylate, mix. 4. Transfer to a cylinder. Wash the mortar with part of vehicle and add to cylinder. 5. Make up to volume with the rest of water. Final product: suspension form that settle rapidly forming a cake like sediment, wrong prep. After correction 1. Weigh the required amount of quinine HCl, then grind it into very fine powder in a mortar with pestle. 2. add acacia powder and mix well with pestle. 3. Add ½ amount of vehicle and mix well. 4. Add amount of sodium salicylate, mix. 5. Transfer to a cylinder. Wash the mortar with part of vehicle and add to cylinder. 6. Make up to volume with the rest of water. Final product: good suspension which will not settle rapidly. Right preparation. Label: Shake Well Before Use Quinine HCl Suspension White Use: Treatment of malaria. One tablespoonful to be taken four times daily. Role of Each Ingredient: Name: Date: Quinine HCl: active ingredient, anti-malarial. Sodium salicylate: anti-inflammatory. Acacia: suspending agent, which decrease the sedimentation rate of suspension by increasing the viscosity of the product. 9 PHT 312 Practical notes