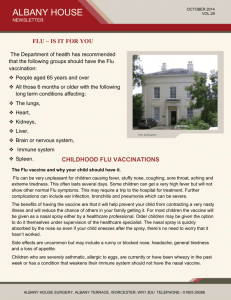
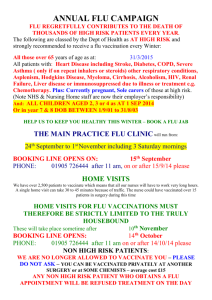
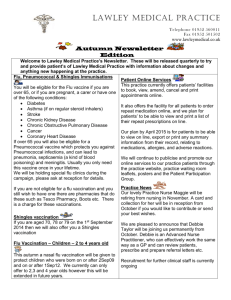
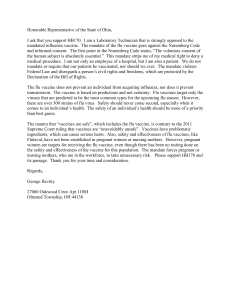
PHE Flu Marketing Campaign 2015/16
advertisement

day Integrated Communications Strategy Seasonal Flu campaign 2015 -16 The marketing toolkit for flu vaccination will be published separately in late summer 2015 and will include the 2015/16 campaign resources. Contents 1. 2. 3. 4. 5. 6. 7. 1 page Ensuring an integrated communications approach Key partners Background Communications objectives Key audiences What is different for 15/16 - extension of the programme to children Key messages: - Generic - Vaccine effectiveness - Important information on vaccine safety lines - Porcine gelatine - Healthcare professionals encouraging patient uptake - Health and social care workers - Charities - Teachers and schools 8. Internal communications 9. Key partners: roles and responsibilities 10. Pilot areas for 2015/16 11. Marketing campaign 2015/16 12. Findings of marketing campaign 2014/15 13. Tactics 14. Key resources (including patient information leaflets) 15. Letters to healthcare professionals 16. Stakeholder analysis and mapping 17. Surveillance systems and reporting 18. Evaluation and Research 2 2 2 3 3 5 Annex 1: Key communications contacts Annex 2: Campaign planning action log Annex 3: Eligible groups Annex 4: Q&A’s (vaccine programme, children’s, JCVI, porcine gelatine, pilot areas, healthcare workers) Annex 5: Resources and links to patient information leaflets Annex 6: Stakeholder engagement coordination plan, mapping and analysis 24 26 29 7 9 10 10 10 11 11 12 12 13 17 17 18 19 21 21 22 22 23 31 44 Purpose: Ensuring an integrated communications approach This integrated communications strategy supports the flu plan and tripartite letter that was published on 27 March and can be found here. The strategy sets out the overall communications strategy for this year’s seasonal flu campaign to be launched on 5 October 2015, and is for the use of communications colleagues in the main partner organisations, namely PHE, DH, NHS England, NHS Employers, DfE and also the Local Government Association for the health and social care audience. The vaccination programme involves a range of partners who need to work closely together and the strategy aims to provide clarity on roles and responsibilities, and defined audiences and it provides information on how we will aim to improve uptake across the groups who will be offered the vaccination in 2015/16. It iterates the timeframe that all the partners need to work to, key timelines over the coming year, and the resources available to the public and healthcare professionals, aiming to provide clarity and eradicate duplication or missed opportunities. This strategy, together with the Flu Plan and letter, outlines the component parts of the flu programme: we will continue to provide regular updates and reminders in advance of, and throughout, the flu season and will ask partners to share their communications plan with us. In 2015/16, marketing activity for flu vaccination will form part of an integrated ‘winter’ marketing campaign which aims to bring together all winter related marketing activity previously led by PHE, DH or NHS England. A marketing toolkit for flu vaccination will be made available separately in late Summer 2015 and will include the 2015/16 campaign resources. A separate communications strategy about PHE’s Cold Weather Plan and winter preparedness will follow. Key partners • • • • • • Public Health England (PHE) Department of Health (DH) NHS England Department for Education (DfE) NHS Employers Local Government Association (LGA) Background In 2015/16, the following groups are eligible to receive the flu vaccination: those aged 65 years and over those aged six months to under 65 in clinical risk groups pregnant women all two, three and four-year-olds (on 31 August 2015) all children of school years 1 and 2 age: - Year 1 school age: 5 year olds, rising to 6 year olds (i.e date of birth between 1 st September 2009 and on or before 31 August 2010) 2 st - st Year 2 school age: 6 year olds, rising to 7 years olds (i.e date of birth between 1 st September 2008 and on or before 31 August 2009) those in long-stay residential care homes carers primary school-aged children in areas that previously participated in primary school pilots in 2014/15 Health and social care workers who are in direct contact with patients or service users are expected to be offered flu vaccinations by their employer, including GP practice staff. Annex 3 includes a list of all the eligible groups included in the national flu immunisation programme. In 2014, the Joint Committee on Vaccination and Immunisation (JCVI) also advised that morbidly obese people (defined as BMI 40+) could benefit from a flu vaccination. Estimates suggest that half of people with a BMI over 40 suffer from long-term conditions such as diabetes which already makes them eligible to receive the flu jab for free. GPs are not currently required to routinely identify those with a BMI over 40. Practices will need to use clinical judgement to decide whether to vaccinate this group of patients. Communications objectives for 2015/16 We will implement a comprehensive communications campaign that seeks to achieve the following primary objectives: • • • • • create an environment in which flu immunisation is a) known about and understood and b) seen as the ‘right thing to do’ just like so many of the other vaccinations in the national programme ensure all those who are eligible for flu vaccine this year, and their carers, know how important flu vaccination is and take up the vaccination themselves explain the wider benefits of the seasonal flu programme and maintain public confidence in the programme, to try and limit any effect that low vaccine effectiveness in 2014/15 has on uptake in 2015/16 ensure that schools and parents understand the importance of why the vaccine should be given to children, and that schools understand the role they have to play in hosting the vaccination programme. ensure health and social care professionals are aware of their duty of care to protect their patients or service users and know the importance of their role, as a trusted healthcare professional, in actively encouraging them to have the vaccination In addition the campaign will aim to: • • • • ensure people understand the high risk associated with flu, particularly for people over 65, at risk groups and women who are pregnant, and the benefits of the vaccine provide information on why children are being offered the nasal Fluenz Tetra® and address concerns that people, and the schools audience, may have about the porcine gelatine content of the vaccination reinforce NHS Employers’ messages to health and social care professionals about the important reasons why they should get vaccinated support charities to educate their members about the risks associated with flu and so encourage them to get vaccinated Key audiences 3 The national communications campaign will target the following groups: Pregnant women Parents and carers of eligible children (see above) People under 65 years of age and their families and carers who are at greatest risk because they have one of the following conditions: o diabetes o weakened immune system (eg HIV or cancer patients) o heart disease o chronic respiratory disease (eg severe asthma, COPD, bronchitis) o kidney disease o liver disease o chronic neurological diseases such as Parkinson’s o people in long stay residential homes o people with a learning disability o a body mass index greater than 40 kg/m² * * Many of this patient group will already be eligible due to complications of obesity that place them in another risk category 4 Health and social care workers who have a responsibility to encourage their patients to get vaccinated (and get vaccinated themselves): o GPs and primary care teams o nurses o midwives o health visitors o social care workers o hospital doctors and secondary care teams o community and hospital pharmacists o other healthcare professionals who have direct patient contact as laid out in the Flu Plan People aged 65 and over Charities who can promote the benefits of flu vaccine to their members, including: Age UK Alzheimer’s Society Asthma UK British Heart Foundation British HIV Association British Kidney Patients Association British Liver Trust British Lung Foundation Cancer Research UK Carers Trust Carers UK Crossroads Cystic Fibrosis Diabetes UK Hepatitis B Foundation Hepatitis C Trust Juvenile Diabetes Macmillan Cancer Support Mencap Motor Neurone Disease Association MS Society Mumsnet National AIDS Trust National Childbirth Trust National Kidney Federation Netmums Neurological Alliance National Council for Voluntary Organisations (NCVO) Parkinson’s UK Rarer Cancers Foundation SCOPE Stroke Association Sue Ryder Care Teenage Cancer Trust Terrence Higgins Trust Professional stakeholders, including the Royal Colleges, trade unions including Unison, and the LGA and Association of Directors of Public Health (ADPH) who can support and reinforce our messages to health and social care professionals that they should have the flu jab to protect their at risk patients or clients. Recent research has also shown that a communication from a healthcare professionals is most influential when encouraging patients to be vaccinated. Organisations and groups who we can work in partnership with to reach our target audiences: o Local radio o Local and national print media o Digital forums like NHS Choices, mumsnet and netmums o Parents’ groups like NCT and Bounty o Specialist media like Saga and Readers Digest o Local Screening and Immunisation Leads (SILs) o NHS England o TV news programmes and talk shows o 4Children o Organisations and groups who can help us address concerns about porcine content with religious groups. WHAT’S DIFFERENT 2015/16: Extension of the national flu immunisation programme to children In 2015/16, all two-, three- and four-year-olds continue to be eligible for flu vaccination, through general practice, as are primary school-aged children in areas that participated in primary school pilots last year. In addition, local NHS England teams will commission the phase 2 extension of the programme to children of school years 1 and 2 age. Delivery models will vary by area, but are likely to be mainly through schools, for example, through school nursing teams or specialist immunisation teams, or in some instances through primary care services. A number of elements of the programme will be dependent upon local commissioning arrangements. 5 We anticipate that the children’s programme, once fully implemented, will ultimately avert many cases of severe flu and flu-related deaths in older adults and people in clinical risk groups. We should continue, however, to work hard to ensure that we are communicating the benefits of the vaccine among all recommended groups, making vaccination as easily accessible for as many as possible. There may be lots of questions from partners and stakeholders, as well as national and regional media, about the extension of the programme to children. The Q&A in Annex 4 aims to provide the background on the childhood part of the programme and address some of the questions about the vaccine to eligible children. 6 Target Groups • • • • Our key messages will target the following groups, where an increase in uptake vaccination rates needs to be driven in terms of the public facing campaign and this strategy: pregnant women people under the age of 65 (including children) in the at risk groups parents and carers of children aged 2, 3 and 4 and children of school year 1 and 2 age health and social care professionals people aged 65 years and over We know the majority of people view flu as a ‘bad cold’ and are unaware of the risks and potentially serious consequences of catching it, particularly for older people, those who have other health conditions or who are pregnant. Our communications to those in at risk groups will focus on the potentially serious or fatal consequences of flu, using statistics from previous flu seasons to emphasise the message. For many parents and carers of healthy children, the idea of annual flu vaccination is still new. Our communications will give them a number of strong and compelling reasons to get their children vaccinated if eligible – emphasising the benefits to the child, the benefits to the parents and the benefits to potentially vulnerable family members, such as grandparents and young siblings. We will use information about the efficacy of the nasal vaccination, and the painless method in which it is delivered, as strong supporting messages. We have produced a new information leaflet and posters for GP surgeries and community pharmacies to raise awareness of the vaccine in 2015/16. We will also promote the vaccine in the places where we know parents with young children go, including online through well used websites like mumsnet, Bounty and NHS Choices and through local radio channels that we know parents listen to. Key messages The key messages below will be communicated throughout the campaign to help raise awareness of the benefits of the flu vaccination and to encourage people to take up the offer of a free flu vaccine if they fall into one of the eligible groups. Primary Messages Secondary Messages 7 Don’t put off getting the flu vaccination; if you’re eligible get it now. It’s free because you need it If you have a long-term health condition, even one that is well managed, or you are pregnant, you are at greater risk of severe complications if you catch flu The nasal spray vaccination is a quick, painless and effective way for children aged 2-4, and in school years 1 and 2, to be protected from flu without the need for injections The flu vaccination is particularly important for those who are at increased risk of flu It is vital that those who are eligible have the flu vaccine every year as the vaccine protects against different strains of flu which evolve each year Key messages around the flu vaccination • Key messages for those with long term health conditions • Key messages for pregnant women • • • • • • Key messages for parents of children aged two to four and in school years 1 and two Impact of flu: 2014/15 season 8 The flu vaccination is one of the most effective ways to reduce harm from flu The flu vaccine reduces risk of serious illness, hospitalisation and even death among those who are most at risk If you have a long-term health condition, even one that is well managed, you are eligible for the flu vaccination free of charge. It’s free because you need it Flu can make the effects of your existing condition worse and makes complications like pneumonia more likely If you are pregnant, you are eligible for the flu vaccination free of charge. It’s free because you need it The flu vaccine reduces the risk of complications and potential harmful consequences for both you and your baby if you catch the flu e.g. premature birth Pregnancy naturally weakens the body’s immune system and as a result you may be less able to fight off infections, increasing the risk of becoming seriously ill as a result of flu The flu vaccine is safe during any stage of pregnancy, it does not carry any risks for you or your baby If you have children aged two, three or four, or in school years one and two, don’t put off taking up their free flu vaccination The nasal spray vaccination is quick, effective and painless and available to children aged 2-4 years, and to those in school years one and two It’s important to protect your little ones from flu and the vaccination is available free on the NHS Flu can be a very unpleasant illness in children as they suffer the same symptoms as adults including fever, chills and aching muscles The flu vaccination will help protect your child from flu and also reduce the chance of flu spreading to others There is evidence that the primary school pilots have had a positive impact on transmission of flu in the wider community. The 2014/15 flu season was of moderate flu intensity. However, in common with other European countries, the number of flu outbreaks in care homes and levels of excess mortality exceeded recent flu seasons, demonstrating how severe the illness can be for those at greatest risk. Hospital surveillance in 2014/15 reported a total of 1,187 ICU/HDU admissions of confirmed influenza across England during the season, including 100 (8.4%) deaths. The cumulative number of cases and deaths were higher compared with the same scheme in 2013 to 2014 when 905 admissions and 98 deaths were reported. A similar proportion of deaths (10.8%) were reported among ICU/HDU cases compared with 2013 to 2014. Vaccine effectiveness For the 2015/16 flu season, a key objective of our communications strategy is to sustain communications to maintain public confidence in the programme and try and limit the impact that vaccine effectiveness findings and subsequent media coverage in 2014/15 will have on uptake in 2015/16. Through the Flu Project Board communications subgroup and cross government winter planning communications group, DH, PHE NHS England and other colleagues will develop more detailed plans to uphold, and continually monitor, public perception and confidence in the vaccine. Providing public reassurance will be a continuous ‘drip-feed’ process in the lead up to the launch of the 2015/16 programme, which has been initiated already by the publication of key documents such as the Flu Plan and letter. The documents will address the issue of vaccine effectiveness seen last winter upfront and we will be making use of any comms and media opportunities these key publications events present, where appropriate. Key messages for 2015/16 on flu vaccine effectiveness are outlined below, but will be reviewed and updated following the publication of PHE’s end of season vaccine effectiveness report in July: - - - - - Flu vaccine is still the best protection we have against an unpredictable virus which can cause severe illness and deaths each year among at-risk groups, including older people, pregnant women and those with a health condition, even one that is well managed. Throughout the last decade, there has generally been a good match between the strains of flu in the vaccine and those that subsequently circulate, so it’s important that we do all we can to ensure people in at-risk groups are not discouraged from having flu vaccination now, or in the future. The World Health Organization monitors flu globally and each year recommends the strains of flu virus that should be included in the flu vaccine for the forthcoming flu season. It takes from February through to August/September for vaccine manufacturers to produce sufficient quantities of the vaccine. There is always the possibility that the virus will change (drift) after the point at which a good and effective vaccine has been produced. If a change in the virus is detected once production has started it is not possible to change the vaccine. But this does not happen every season. The last time a drifted strain circulated like this was in 2003/4, when we saw the A/Fujian strain circulate. That means that in the past nine out of ten seasons the vaccine has provided good to moderate protection against the circulating strains. Communications leads are encouraged to explore opportunities to educate their various audiences on; the fact that flu virus is constantly changing, the complex process of vaccine manufacturing; the possibilities of drift after the point at which a good and effective vaccine has been produced and the potential for delays in vaccine availability at the beginning of the season, as was also seen in 2014/15. To assist with this, vaccine manufacturers are producing an online video for use in the 2015/16 season, to explain the complex manufacturing process. It’s also important that the role of WHO (see above) is defined clearly in these communications. 9 All public information (leaflets, schools resources etc) for 2015/16 will incorporate agreed lines on vaccine effectiveness, and the messaging will also be considered when marketing materials are developed for 2015/16. Vaccine safety In 2014/15, PHE became aware that some partners are referring to the flu vaccination as ‘completely’ or ‘perfectly’ safe in communications to promote the vaccine. It remains true that the vaccines used for the annual flu vaccination programme in the UK have excellent safety records, but this phrase does not recognise that all vaccines or medicines have some risks that are reflected in the product information. Any risks of flu vaccination are outweighed by the expected benefits, and so it is important that we continue to promote vaccination to eligible groups. Please ensure that all promotional materials for the current season are used to do so, and review any current resources (including websites) to ensure these phrases are not used in 2015/16. It is accurate to state that the vaccines are ‘safe’ or ‘have excellent safety records’. Porcine gelatine PHE has responded to media reports about porcine gelatine used in vaccines, including Fluenz Tetra® https://www.gov.uk/government/news/vaccines-and-gelatine-phe-response Porcine gelatine has been certified as acceptable by many multi-faith groups. Gelatine is used to stabilise live viral vaccines and is contained in many pharmaceutical products, not just Fluenz Tetra®. It is the considered view of PHE and the Department of Health that because the children’s part of the programme is designed to protect as many people in the community as possible including those who cannot have flu vaccine, the inactivated injected vaccine is not a suitable alternative to Fluenz. Therefore, the recommendation is that the nasal spray vaccine Fluenz is used to vaccinate healthy children. As in previous years, inactivated vaccine can be used in children over six months of age who have underlying illnesses that put them at particular risk of influenza; in most cases two injections will be required. Further information and links to FAQs for both parents and healthcare professionals can be found at the link above. Encouraging patient uptake through healthcare workers We know that the public trust the advice given to them by the healthcare professionals they see on a regular basis, such as their GP, practice nurse, midwife or local pharmacist, and attitudinal research conducted in 2014/15 has reinforced this further. A crucial part of our campaign to encourage the public to get vaccinated will be about ensuring health and social care professionals are getting the right message to their patients and are playing an active role in inviting people to get vaccinated. More information about how we will communicate to healthcare professionals, whilst also complementing the NHS Employers Flu Fighter campaign, is included below. 10 Subject to Cabinet Office approval, the PHE marketing campaign will target the general public, but PHE will also be working with NHS Employers to find new ways of encouraging healthcare workers to encourage uptake of patients, as an additional strand to the healthcare worker campaign. As part of the evaluation process for the 2015/16 campaign, PHE and NHS England will be considering how they can further engage with primary care colleagues directly, to consult them on the information and resources available to assist them in delivery of the programme. A survey of GPs and other frontline professionals will be explored. Health and social care workers Our aim is to ensure health and social care professionals get vaccinated themselves and actively encourage their eligible patients to get vaccinated. This means building on and complementing the NHS Employers communications campaign (Flu Fighter) and working closely with NHS England and other partners, like the Royal Colleges, to ensure health care professionals are receiving the right information and are actively promoting flu vaccination. The NHS Employers Flu fighter campaign will be the primary route through which health care workers are encouraged to get themselves vaccinated. National and local activity will take place as part of this campaign and we will work closely with NHS Employers to reinforce and complement their activity where appropriate. Working closely with NHS England and other partners we will ensure health and social care professionals know the risk factors for particular patient and client groups and can clearly communicate the benefits of flu vaccination to such groups. Our key message to them is that it is their responsibility to play an active part in increasing vaccine uptake for these groups. The Local Government Association is a member of the flu programme board’s communications sub group and will be supported to include its social care workers in a campaign for 2014/15 if they choose to do this as part of their health and wellbeing board remit. Charities Charities that support particular conditions or patient groups provide important routes to those members of the public who are at the most risk and we want them to encourage their members to get vaccinated. We will work closely with these organisations and provide communications materials (including key messages and cases studies relevant to that particular condition) that they can use to promote flu vaccine. The reason it is important to focus on key charities, for example, is that those with neurological conditions are approximately 40 times more likely to die if they develop flu than individuals who have no other underlying health condition. Those with chronic liver disease are 48 times more likely to die. Charities looking after those with chronic liver and neurological disease will be encouraged to support the campaign this year. Teachers and schools Good relationships with schools will be key, as parents and children are likely to look to the school workforce (as well as school nurses) for advice and guidance on flu vaccination in schools, and so will need to be able to understand, support and reinforce key messages. A high volume of immunisations will take place in schools. Messages to schools will also need to convince the school workforce of the benefits to them (eg possible reduced absenteeism) as well as giving confidence that the programme will be well-managed and that the school workforce will be well-informed and able to advise parents accordingly (where appropriate), or direct queries to relevant healthcare services. 11 Partners, including the media, parents groups and digital communities We will work closely with those organisations or groups who can help us to ensure our messages about flu vaccine are reaching the right people. This includes national, local and specialist media where we will provide stories that reinforce messages to the public and professionals, digital communities such as mumsnet and netmums which are useful to reach parents of eligible children, and local radio, which we can target with the right advertising, depending on listeners’ demographic. Internal Communications It is vital that partner organisations’ staff understand the rationale and the delivery of the flu programme from both a professional basis (talking to other organisations) but also from a personal perspective. Where partner bodies offer its staff vaccination for flu it is important that their internal communications run along the same timeframe as the national programme. 12 Key Partners: Roles and responsibilities We will work closely with our partners to ensure that we are all aware of what each other is doing and to plug gaps and avoid duplication. We will ask partners to share their communications plan with us and a cross party meeting of flu comms leads will take place on a regular basis in the lead up to the 2015/16 flu season. The respective responsibilities for the flu programme generally are set out in the Flu plan. Below we have outlined the roles and responsibilities for the different organisations supporting flu vaccination communications activity this winter. As an overview: The Department of Health is responsible for: policy decisions on the response to the flu season holding NHS England and PHE to account through their respective framework agreements, the Mandate, and the Section 7A agreements oversight of the supply of antiviral medicines CMO updates and DH supports via Twitter (where appropriate) CMO/CPhO letters and updates Ensuring DH policy teams are fully in the loop with communications and are responsible for the liaison with OGDs NHS England is responsible for: commissioning the flu vaccination programme under the terms of the Section 7A agreements assuring that the NHS is prepared for the forthcoming flu season building close working relationships with local authorities particularly Directors of Public Health (DsPH) to ensure that local population needs are understood and addressed by providers of flu vaccination services ensuring the following receive timely information including the flu plan and letter: o GPs, practice nurses and practice managers o Community and hospital pharmacies o CCGs o Screening Leads o Directors of Nursing o Accountable Officers o LA CEOS through NHS News Public Health England is responsible for: 13 planning and implementation of the national approach monitoring and reporting of key indicators related to flu, including flu activity and vaccine uptake oversight of the vaccine supply and the strategic reserve advising NHS England on the commissioning of the flu vaccination programme supporting DsPH in local authorities in their role as local leaders of health and ensuring that they have all relevant expert input, surveillance and population data needed to carry out this role effectively. Also liaising with ADPH. promotion via the established communications channels including web and PHE News. NHS Employers The NHS Employers organisation is the voice of employers in the NHS, supporting them to put patients first. Their vision is to be the authoritative voice of workforce leaders, experts in HR, negotiating fairly to get the best deal for patients. They are responsible for communicating the Flu Fighters campaign to all NHS Employees. All employers of individuals working in the NHS are responsible for: management and oversight of the flu vaccination campaign for their frontline staff support to providers to ensure access to flu vaccination and to maximise uptake amongst those eligible to receive it NHS Employers has already actively engaged with the flu leads for over 92 Trusts through a series of regional workshops. Local authorities, through their Director of Public Health, have responsibility for: providing appropriate challenge to local arrangements and advocacy with key stakeholders to ensure access to flu vaccination and to improve its uptake by eligible populations providing independent scrutiny and challenge to the arrangements of NHS England, PHE and local authority employers of frontline social care staff and other providers of health and social care providing leadership, together with local resilience partners to respond appropriately to local incidents and outbreaks of flu infection Through the LGA we will seek to reach 14 elected members CEOs Directors of Public Health Directors of Childrens’ Services o Frontline social workers and health and social care workers Directors of Adult Services o Frontline social workers and health and social care workers Clinical Commissioning Groups (CCGs) are responsible for: quality assurance and improvement which extends to primary medical care services delivered by GP practices including flu vaccination and antiviral medicines. They are reached through NHS England primarily, also PHE regional teams, and National Association of Primary Care. GP practices and other providers are responsible for: ordering the correct amount and type of vaccine for their eligible patients, taking into account year on year increases or new groups identified for vaccination and the ambition for uptake ensuring that all those eligible for the flu vaccine are invited personally to receive their vaccine encouraging and facilitating flu vaccination of their own staff ensuring that antiviral medicines are prescribed for appropriate patients, once the CMO/CPhO letter has been distributed alerting them that antiviral medicines can be prescribed. Specific duties: Comms Team Public Health England Activity National: - Develop national communications strategy Develop and promote national advertising campaign Develop national materials including leaflets and posters Liaise with national partners and stakeholders eg NHS Employers, DfE, LGA Provide weekly flu data during the flu season which will include the number of vaccinations delivered, rates of GP consultations and number of hospital admissions etc and manage communications around these outputs and other publications Regional/local: - - - NHS England 15 - Signpost local organisations to the materials Work with NHS England and local authorities on development, co-ordination and sharing of localised messaging eg template articles, targeted press releases Signpost and publicise weekly flu data during the flu season which will include number of vaccinations delivered, rates of GP consultations and number of hospital admissions etc. Work closely with PHE, Local Authority, local Clinical Commissioning Groups (CCGs) and their Commissioning Support Unit (CSU) teams to ensure an integrated implementation of communications to support the flu plan Ensure all NHS commissioning organisations are aware of the national campaign and are able to access new materials including NHS Employers ‘Flu Fighters’ materials. This will be - - - - - - - Local Authorities via LGA - - - 16 achieved through the CCG Bulletin, NHS News Bulletin and CSU Communications Network provide supporting PR around any national communications activity including quotes from Medical Director Sir Bruce Keogh or other appropriate Executive Team members for joint press releases, media interviews, etc. Support Screening and Immunisation Teams in the communications work implementing the flu plan eg helping to update national templates for local GP letters to patients, awareness raising among primary care staff via local NHS England teams communications, etc Support dissemination of materials through NHS England channels (national website /social media) to partners (in particular schools and LAs), the public and patients Support dissemination of material and messaging to NHS England staff in central team, regional and local NHS England teams through channels such as NHS News, Intranet and staff briefings Work closely with PHE, LA and CCG communications teams to ensure an integrated implementation of communications to support the flu plan GP practices, supported by their own communications channels such as websites and patient newsletters, are the most effective and therefore a primary communication mechanism for encouraging vaccination uptake GP surgeries will be able to download national campaign materials via the NHS Choices, PHE and NHS Communications Link website, and order some materials through the publications orderline GP surgeries should be responsible for proactive messages via communications channels such as websites and patient newsletters CCGs should help support GPs in promoting the flu campaign using national materials CCGs and their CSUs should work alongside PHE, NHS England and LA communications teams to ensure an integrated implementation of communications to support the flu plan Liaison through ADPH and Health and Wellbeing Boards Responsible for developing local plans on flu for their local authority Ensure frontline social care staff protect themselves by having the flu vaccine to prevent the spread of flu to colleagues and other members of the community. Also encourage uptake among carers and council staff who fall into a target group Encourage social care staff to be advocates of the vaccine Facilitate appropriate access to information and vaccination services for ‘underserved’ populations Support Health and Wellbeing Boards who have a role in oversight and challenge of commissioners to ensure that they achieve and sustain high uptake. Issue press releases to support the campaign and field DsPH and councillors (if appropriate) as local ’voice’ of the whole health and social care system - - Promote key messages through resident newsletters (template articles available from PHE) / website / social media / PR channels etc. Retweet messages from national PHE/DH/NHS England twitter accounts Encourage community pharmacy teams to be advocates of the vaccine Department of Health Health ministerial updates Liaising with other departments, particularly Education Messaging to schools etc Children and Families (women who are pregnant/families with children 2-5) Supporting social media and messaging Target key charities who represent at risk patients (supported by PHE) Department for Education Education ministerial updates Education messaging to schools with DH Supporting social media and messaging Supporting in ensuring that parents are provided with information/background about the programme which PHE are developing Supporting in aligning planning for the vaccination programme which can only take place within a short timeframe, to fit in with other planned activity in the Autumn (exams and coursework) LGA H&W Boards DoPH DoAS and DoCS Unision and unions for health and social care workers Working with LAs to ensure the best approach to local delivery PHE Flu Marketing Campaign 2015/16 PHE runs marketing programmes annually encouraging vaccination uptake. While UK vaccination rates are generally very high when benchmarked globally, there is still room for improvement. In 2015/16, marketing activity for flu vaccination will form part of an integrated ‘winter’ marketing campaign which aims to bring together all winter related marketing activity previously led by PHE, DH or NHS England. A marketing toolkit for flu vaccination will be made available separately in late Summer 2015 and will include the 2015/16 campaign resources. It will be necessary to produce patient information leaflets etc for this year’s flu season before the marketing assets are distributed. These are in production and are being published as they become available. Leaflets and guidance for: parents, schools and head teachers and healthcare teams working with schools have been produced and are available on the Immunisation pages of .Gov.uk. In addition there are leaflets targeting parents of eligible children, pregnant women and a general information leaflet aimed at all those who are eligible. In 2014/15, it became apparent that there was low awareness amongst healthcare professionals and the public that people with learning disabilities are eligible for a free 17 vaccination. Because of this, a new easy read patient information leaflet is being developed for the 2015/16 flu season. Communications leads are encouraged to promote this through relevant local networks and with mental health partners. All patient information leaflets will be available by mid-June 2015 in hard copy, with the option to order further copies online. The launch of the campaign in 2015/16 will include: • • Press stories, including case studies Social media campaign including activity on Twitter and on Facebook, using charity partners to drive forward targeted messaging (“If you are diabetic, you’re entitled to a free flu jab; protect yourself and your family” etc). Findings from 2014/15 marketing campaign In 2014/15, the national marketing campaign consisted of press, radio and paid search advertising, which was up-weighted with out-of-home and TV advertising in the North East region to test these additional methods in this area. The campaign targeted people aged 1665 with long term health conditions (at risk) and pregnant women. Parents of children aged 2-4 were targeted through PR activity. Media activity undertaken for the 2014/15 campaign achieved the following mass media coverage at both national, and regional and local, level. Whilst overall a percentage increase in vaccine uptake was not observed at the end of the season, this activity is likely to have contributed to the campaign’s positive performance in terms of reach and cut through (number of people reached and influenced), and some improved knowledge and attitudes towards flu vaccination: • 450 pieces of national, regional and local broadcast, print, and online coverage. • 2,000+ Twitter mentions including #spreadthewordnotflu. = In excess of 84,000,000 total opportunities to see and a PR Value of: £2,700, 000+ • National tabloid press adverts with 21million circulation. • Commercial radio ads with 28million audience. • 132,0000 patient information leaflets distributed. In summary, the key findings were: Despite indications that the campaign performed well in terms of reach and cut through, and for some attitudes, knowledge and claimed behaviour, ultimately there was no impact of the increased campaign weight on vaccination rates in the North East. While we don’t know the precise impact of having no campaign, it appears the most important factors influencing flu vaccination uptake are at the local level, and are likely to be related to health care professional and socioeconomic factors, for example levels of deprivation and inequality. Additional findings 18 Vaccination uptake data shows at a total population level: o The overall flu vaccination rates in 2014/15 were generally similar to recent seasons. A great deal of variability is evident by audience (from -4.1% change in vaccination rates in 2 year olds through to +4.3% in pregnant women). Econometric modelling indicates the boosted campaign in the North East did not increase vaccination rates there, among any target group once geo-demographic factors are taken into account. However, tracking data found that: o Up weighting did drive higher reach and cut through in the ‘at-risk’ group and pregnant women in the North East o No change in attitudes towards flu itself, but some improvements in attitudes towards flu vaccination, though no more likely in North East o Some indications that campaign increased self-reported knowledge/behaviour among pregnant women and mothers of 2-4s, for whom flu vaccine message most likely to be new, though this was no higher in the North East From both the tracking and modelling there is strong evidence that other factors are explaining variation in take up, with the tracking finding health professionals to be the key source of information and prompt to action for all audiences and CCGs accounting for 52% of variability in the modelling. Tactics We will promote flu vaccination to public groups using: National advertising Details will be included in phase 2 of this strategy. Leaflets and posters These will be used in community pharmacies, GPs surgeries, schools and online on websites such as NHS Choices. . Leaflets targeting parents of eligible children, pregnant women, and a general leaflet aimed at all eligible groups will be available. Template letters for GP surgeries, schools, and community based delivery can be downloaded from the GOV.UK website and adapted for local use. Digital communications NHS Choices is recognised as the site where the public go to find information about particular conditions or NHS services. We will feature information about seasonal flu vaccine on the NHS Choices homepage from early October and ensure that content reflects the key message about the risks association with flu and importance of the flu vaccination (for all eligible groups). Other digital opportunities such as partnerships with Mumsnet and other family websites will be considered. Social media We will use social media channels such as @PHE_uk and @DHgovuk and @NHSChoices to reach a wide and varied audience and actively encourage partners to retweet key messages. We know that women who are pregnant, parents of young children and children and younger adults are avid users of social media and so we are considering how we can most effectively use Facebook to engage these audiences specifically. The hashtags that the @PHE_uk Twitter account and other PHE Centre accounts will be using around the launch of the 2015/16 campaign will be confirmed and 19 circulated to stakeholders following confirmation of the marketing campaign proposals. Information will include suggested messages to use on social media, including Tweets and Facebook posts. National, local and consumer media stories We will run stories featuring key messages about risk factors associated with flu and the importance of getting the vaccine, starting in early September with a press release highlighting the start of the children’s flu programme. Consumer magazines such as Mother and Baby or Pregnancy magazines will be used to target specific groups. Celebrity ambassadors were successful in securing media coverage in consumer press and on social media in 2014/15, and this will be considered again for 2015/16. Charity partnerships We will send a communications pack, including a letter from CMO, template articles, key messages and a factsheet about risk factors tailored to particular conditions, to key charities like Diabetes UK who represent the people most at risk from flu. We will actively encourage them to use our messages and encourage their members to get vaccinated. Patient cases studies will also be provided to assist. We will ensure staff groups (including teachers) are actively promoting flu vaccination using: 20 Information and training materials FAQs and training materials are available online at www.gov.uk/phe providing specific details about the seasonal flu programme and extension to eligible children. These are supported by the recently published flu letter and plan. Digital communications We will work with the CMO, Deputy CMO and PHE Directors to produce video and/or audio content for the PHE and DH websites, aimed specifically at staff groups. This will be clear about the active role health and social care staff must play in encouraging their patients to get vaccinated. We will support and/or complement digital communications from NHS Employers Flufighter campaign. Trade media stories We will announce the start of programme with press releases targeted to trade media like GP, Pulse and the Nursing Times. Communications from our partners in the health system We are working closely with NHS Employers to support the NHS Flu fighter campaign and ensure there are consistent messages about the active role staff should play to encourage flu vaccination. We are working closely with NHS England to ensure that professional leads, such as the NHS Medical Director, Chief Nursing Officer, Chief Pharmaceutical Officer and the Chief Allied Health Professions Officer are promoting flu vaccination, using publications such as the Chief Nursing Officer bulletin and NHS News to provide regular updates – Also key DH people – Health Ministers (SofS and PS(PH)), CMO and deputy CMO, Chief Pharmaceutical Officer. Stakeholder partnerships We are working closely with stakeholders, like the Royal Colleges and BMA, and health and education workforce unions, to ensure they are including regular updates and reminders about the importance of the flu vaccination programme, for both themselves and their patients. We will use the Stakeholder Communications Forum as a way to ensure regular messages are reaching communicators in stakeholder organisations and actively encourage them to feature information about flu vaccination in their own communications. • Media partnerships Consideration will be given to working with key national press, targeting their health professionals websites and society blogs to raise the awareness of the flu campaign and why people should have the vaccinations they are entitled to. This is a good way to do some mythbusting by allowing people to post comment and countering with the science. Case Studies A number of case studies are being proposed that could be shared across the internet as per last year’s examples of case studies for patients with diabetes and liver disease (links below): https://www.youtube.com/watch?v=slYDg7rYwwU https://www.youtube.com/watch?v=X5-QTGpobh8 PHE is also working with NHS England and DfE colleagues to produce case studies of schools that have delivered flu immunisation to children in previous years by participating in pilot areas. Once complete, the case studies will be available online and promoted by relevant partners including the DfE. Key Resources including Public Documents to be updated The following resources have been available in previous years to support local communications to healthcare professionals, parents and at-risk groups. It is expected that these will be updated and made available via download or the DH/PHE Orderline for the 2015/16 flu season. As mentioned above, patient information leaflets will be produced for: - All eligible patient groups (generic leaflet) Pregnant women Parents of eligible children People with learning difficulties (easy read version) Letter template for GP surgeries to download will be available from the GOV.UK website. These will be available to invite 2, 3 and 4 year olds for flu vaccination as well as a general one for people eligible for flu vaccination. In addition, there are dedicated resources now available for schools: - - leaflet for schools and head teachers Public information leaflets for parents - Template letters for schools to send to parents of eligible children Consent forms See annex 5 on page 45 for further information. Letters to healthcare professionals NHS Employers will again be producing a series of letters to all frontline healthcare staff, including doctors, allied health professionals, nurses and midwives. The letters will include clinical evidence, and will be circulated within hospitals and Foundation Trusts and all NHS 21 outlets to encourage staff to fulfil their professional duty of care, and to protect themselves, their patients, their colleagues, and their family, by taking up their flu vaccination this winter. Last season’s letters and clinical evidence can be found on NHS Employer’s website here. NHS Employers will encourage managers to discuss these letters with their teams, as a way of keeping flu in conversation over the vaccination season. The PHE website, PHE Vaccine Update bulletin and PHE social media channels (eg Twitter, Facebook) will also be used to promote the uptake of flu vaccination by healthcare professionals, including raising awareness of these letters. A charity campaign pack will be available for all health related charities to download and this may include posters targeted to specific health conditions which charities can use to promote the flu campaign with their own audiences. Charities will also be encouraged to make use of an online liver disease patient case study where relevant, and a diabetes case study. As well as healthcare professionals, the campaign must reach those allied healthcare workers including porters, cleaners, catering staff etc, and so liaison with unions such as UNISON is crucial. It must be determined who “owns” this relationship as they are not NHS employees. Stakeholder analysis and mapping A wide range of stakeholders have influence on the delivery of influenza immunisation, either directly on those who will be vaccinated or on other parts of the delivery chain, such as with vaccine suppliers. A tripartite Stakeholder Engagement Plan has been produced to ensure all stakeholders are identified and engaged with at the appropriate level. This is appended to this strategy (annex 6, page 46) together with a stakeholder analysis and mapping document. Surveillance PHE's Weekly National Influenza Reports and Weekly All-Cause Mortality Reports are published weekly during the winter period (Oct-Jun) and fortnightly during the summer (June - Oct). These reports capture community influenza surveillance (through syndromic surveillance), overall weekly influenza GP consultation rates across the UK, influenzaconfirmed hospitalisations, all-cause mortality data, microbiological surveillance, vaccination rates (from Immform) and information on the international situation. The PHE Winter Health Watch Summary captures all PHE data outputs, with planning resources and is issued on a weekly basis from the beginning of November to the end of April, including data on indicators of influenza and respiratory syncytial virus (RSV) activity, together with overall weekly influenza GP consultations. In addition, flu vaccine uptake reports for GP patient groups will be published on a monthly basis as follows for the 2015/16 flu season: - Thurs 26th November Thurs 24th December Thurs 28th January Thurs 25th February And for healthcare workers as follows: 22 - Thurs 19th November Thurs 17th December Thurs 21st January Thurs 18th February Thurs 17th March In January 2016 a mid-season vaccine effectiveness report will be published, with a final end of season report published in June/July 2016. An annual flu report, together with two end-ofseason reports on vaccine uptake for both patient groups and healthcare professionals will be published in June 2016. Publication dates for these reports will be scheduled later in the season. Communications colleagues within PHE’s regional network should be fully integrated into these surveillance reporting processes, so that in partnership with their counterparts in NHS England, they can provide an immediate response in supporting colleagues, to drive immunisation uptake where outliers arise throughout the season. It is particularly important that efforts to promote and raise awareness of flu vaccination are sustained throughout winter, since any flu vaccination marketing campaign is likely to be implemented within a limited timeframe, with flu season extending far beyond this period. Evaluation and Research The findings from pre and post campaign evaluation and research conducted as part of the marketing campaign evaluation for the 2014/15 campaign is being used to help form messaging for the programme in 2015/16. Further attitudinal research on the subject of vaccination more generally has been commissioned by PHE and will also be used to inform messaging and resources once the findings are available. Media coverage will be monitored as part of PHE’s routine media evaluation service, and by any relevant PR agencies as part of the evaluation for the marketing campaign. Evaluation and research undertaken in 2014 further reinforced the importance of a communication from eligible healthcare professionals in advising patients to have the vaccination. Therefore in 2015, communications colleagues will be considering how they can further engage with primary care colleagues directly, to consult them on the information and resources available to assist them in delivery of the programme. A survey of GPs and other frontline professionals will be explored. In addition, PHE’s patient representative group, ‘The People’s Panel’ will be utilised to consult the public on how likely it is that last season’s vaccine effectiveness findings and resulting media coverage will discourage vaccination in 2015/16, and in future years. 23 ANNEX 1: Key Communications Contacts PHE Department of Health NHS England PHE Communications Lead – Lisa Ettridge - 020 7210 5281 Charlotte Hutchinson - 0113 8557362 Bash Khan - 020 7210 5222 Juliet Nowell - Programme Comms Manager j.nowell@nhs.net 0113 825 0965 Press/PR – John Ratchford Deputy Director - Dorian Kennedy 0208 327 6217 Policy – Helen Lovell Marketing/Advertising – Andrew Wilson 020 3682 0619 Seasonal flu implementation lead – Angela Edwards Public information (leaflets/factsheets etc) – Chris Owen/ Phil Hemmings Ministerial briefings - Zubeda Seedat Letters to professional bodies – Zubeda Seedat DH email addresses are: Firstname.surname@dh.gsi.gov.uk PHE email addresses are firstname.surname@phe.gov.uk NHS Employers Mike Foster Mike.Foster@nhsemployers.org 020 7799 8671 Department for Education Jane Garvan Head of Campaigns, Engagement and Publishing Jane.GARVAN@education.gsi.gov.uk 24 Local Government Association Samantha Ramanah Samantha.Ramanah@local.gov.uk 0207 664 3079 Mike Forster – Media Relations Advisor mikeforster@nhs.net 0113 824 9464 Pauline Macdonald - Programme Director, National Child Flu Immunisation Taskforce paulinemacdonald@nhs.net 01138248717 Sarah Jones - Childhood Flu Programme Manager sarah.jones86@nhs.net 07920 252006 NHS Choices Via Chris Owen/ Phil Hemmings for PHE kathrynbingham@nhs.net Tel: 020 7783 8484 07990 082898 Kathy McTaggart, School staffing, health and safety team Kathy.Mctaggart@education.gsi.gov.uk Tel: 0207 3408231/ ext: 308231 25 Annex 2: Campaign Planning Actions Log DUE DATE MILESTONE UPDATE LEAD ORG Campaign evaluation Evaluation of flu vaccine campaign 2014/15 Ongoing Stakeholder analysis Integrating existing stakeholder analysis work into the flu comms strategy and consulting with education partners on engaging new stakeholders for 2015/16. PHE Ongoing Comms resources Work with partners to develop comms materials to explain the flu vaccine manufacturing process undertaken in short timeframe each year and associated risks. PHE 31 March Produce schools resources Briefing for schools and headteachers (updated from last year) 31 March Flu letter Publish flu letter for 15/16 and ensure PHE communicates with audience defined PHE 31 March Flu Plan Publish flu plan for 15/16 and ensure PHE communicates with audience defined PHE 19 June Marketing campaign Efficiency and Reform Group (ERG) sign off for marketing spend granted From June and then ongoing Regular meetings with partner comms teams Ongoing 30 June Comms Plan for 15/16 signed off by all parties Phase 1 comms strategy published 2015 April 26 PHE PHE Cabinet Office PHE PHE 31 July Public information materials Public info leaflets published and available through Orderline. Letter templates available to download and use locally. 31 July Web updates (incl NHS Choices) Copy signed off and updated 30 September Stakeholder engagement Letters to Education, H&SC Professionals, charities, professional bodies etc, 30 September Engagement with charities and education partners Case studies and toolkits 3 August Marketing campaign research Winter marketing campaign research commences 17 August PHE NHS Choices DH PHE PHE Marketing campaign research PHE Winter marketing campaign research results available 31 August Marketing campaign Winter marketing campaign – flu vaccine creative work finalised PHE September Marketing campaign Winter marketing campaign – flu vaccine toolkit cascaded PHE 5 October Launch flu Campaign PHE More detailed communications plans for launch to be shared in due course. 27 2016 January 2016 Mid -season vaccine effectiveness report published June 2016 Annual Flu Report and final vaccine uptake reports for 2015/16 published 28 PHE Develop tripartite comms handling plan for publication. PHE Develop tripartite comms handling plan for publication. Annex 3 - Groups included in the national flu immunisation programme 1. In 2015/16, flu vaccinations will be offered at NHS expense to the following groups: • people aged 65 years or over (including those becoming age 65 years by 31 March 2016) • people aged from six months to less than 65 years of age with a serious medical condition such as: o chronic (long-term) respiratory disease, such as severe asthma, chronic obstructive pulmonary disease (COPD) or bronchitis o chronic heart disease, such as heart failure o chronic kidney disease at stage three, four or five o chronic liver disease o chronic neurological disease, such as Parkinson’s disease or motor neurone disease, or learning disability o diabetes o splenic dysfunction o a weakened immune system due to disease (such as HIV/AIDS) or treatment (such as cancer treatment) • all pregnant women (including those women who become pregnant during the flu season) • all those aged two, three, and four on 31 August 2015 (i.e. date of birth on or after 1 September 2010 and on or before 31 August 2013) through general practice1 • all children of school years 1 and 2 age through locally commissioned arrangements2 • primary school-aged children in areas that participated in primary school pilots in 2014/15 • people living in long-stay residential care homes or other long-stay care facilities where rapid spread is likely to follow introduction of infection and cause high morbidity and mortality. This does not include, for instance, prisons, young offender institutions, or university halls of residence • people who are in receipt of a carer’s allowance, or those who are the main carer of an older or disabled person whose welfare may be at risk if the carer falls ill • consideration should also be given to the vaccination of household contacts of immunocompromised individuals, specifically individuals who expect to share living accommodation on most days over the winter and, therefore, for whom continuing close contact is unavoidable 2. The list above is not exhaustive, and the healthcare practitioner should apply clinical judgement to take into account the risk of flu exacerbating any underlying disease that a patient may have, as well as the risk of serious illness from flu itself. Flu vaccine should be offered in such cases even if the individual is not in the clinical risk groups specified above. 3. Also recommended to be vaccinated as part of an employer’s occupational health obligation: • health and social care workers with direct patient/service user contact 4. The JCVI has also advised that morbidly obese people (defined as BMI 40+) could also benefit from a flu vaccination. This has not been included as part of the GP contract in the 2015/16 DES. Many in this patient group will already be eligible due to complications of obesity that place them in another risk category. Practices will need to use clinical judgement to decide whether to vaccinate this group of patients, but vaccinations for morbidly obese patients with no other recognised risk factor will not attract a payment under the DES in 2015/16. The inclusion of this patient group into the flu programme from 2016/17 is currently under consideration. 29 Healthcare practitioners should refer to the Green Book influenza chapter for further detail about clinical risk groups included in the national flu immunisation programme. This is regularly updated, sometimes during the flu season, and can be found at: www.gov.uk/government/collections/immunisation-against-infectious-disease-the-green-book Further information on the service specification for delivery of the seasonal influenza immunisation programme and the seasonal influenza programme for children can be found at:www.gov.uk/government/publications/public-health-commissioning-in-the-nhs-2015-to-2016 The list above is not exhaustive, and the healthcare practitioner should apply clinical judgement to take into account the risk of flu exacerbating any underlying disease that a patient may have, as well as the risk of serious illness from flu itself. Flu vaccine should be offered in such cases even if the individual is not in the clinical risk groups specified above. For further information, see the Influenza Chapter 19 of the Green Book. 1 Some four-year-olds who have started school may be offered flu vaccination through a school-based provider depending on local commissioning arrangements 2 Year 1 is defined as five- rising to six-year-olds (ie date of birth between 1 September 2009 and on or before 31 August 2010) Year 2 is defined as six- rising to seven-years-olds (ie date of birth between 1 September 2008 and on or before 31 August 2009) Some children in years 1 and 2 might be outside of these date ranges (eg if a child has been accelerated or held back a year). It is acceptable to offer and deliver immunisations to these children with their class peers. 30 Annex 4: Q&As Q&A: FLU VACCINATION PROGRAMME 1. What is the aim of the flu vaccination programme? The flu vaccination programme is based on independent expert advice from the Joint Committee on Vaccination and Immunisation (JCVI). The current flu vaccination policy aims to reduce the serious morbidity and mortality due to flu by immunising those people most at risk of serious illness or death should they develop flu. This policy is in line with most other countries that have seasonal influenza vaccination programmes. Another benefit of vaccination is to reduce transmission of the infection, thereby contributing to the protection of vulnerable patients who cannot be vaccinated or may not respond well to their own immunisations. This is the reason that we recommend that frontline health and social care workers are vaccinated to minimise the spread of flu to patients and service users. In July 2012, the JCVI recommended extending the programme to healthy children. This programme will lower the potentially serious impact of influenza on those children but should also have a more profound effect on influenza transmission. Children are the main source of transmission in the population, and this programme will therefore reduce the spread of infection from children to other children, to adults and to those in clinical risk groups of any age. The Secretary of State accepted this recommendation, and the implementation of the extension commenced in September 2013 with a general practice roll-out to children aged 2 and 3 years, followed by the addition of four year olds in September 2014. This year, the programme in general practice will continue and local NHS England teams will commission the phase 2 extension of the programme to children of school years 1 and 2 age. Delivery models will vary by area, but are likely to be mainly through schools, for example, through school nursing teams or specialist immunisation teams, or in some instances through primary care services. A number of elements of the programme will be dependent upon local commissioning arrangements. In areas that delivered flu vaccination to children in primary schools through pilots in 2014/15, these will continue in 2015/16, but there will be no continuation of pilots delivered through secondary schools in 2015/16. 2. Who should consider having a flu vaccination? Although everyone is at risk of catching flu, for most healthy people, flu is an unpleasant but usually self-limiting disease. However, older people, the very young, pregnant women and those with underlying disease are at particular risk of severe illness if they catch flu. You should have the flu vaccination if you are: A child aged 2, 3 or 4 years. A child of school years 1 or 2 age: - Year 1 school age: 5 year olds, rising to 6 year olds (i.e date of birth between 1 st st September 2009 and on or before 31 August 2010) - Year 2 school age: 6 year olds, rising to 7 years olds (i.e date of birth between 1 st September 2008 and on or before 31 August 2009) aged 65 years or over living in a residential or nursing home 31 st the main carer of an older or disabled person (by having the vaccine, paid and unpaid carers will reduce their chances of getting flu and can then continue to help those they look after.) a household contact of an immunocompromised person a frontline health or social care worker pregnant. or if you have: a heart problem a chest complaint or breathing difficulties, including bronchitis or emphysema a kidney disease lowered immunity due to disease or treatment (such as steroid medication or cancer treatment) liver disease had a stroke or a transient ischaemic attack (TIA) diabetes a neurological condition, for example multiple sclerosis (MS), cerebral palsy or a learning disability a problem with your spleen, for example sickle cell disease, or you have had your spleen removed. a body mass index greater than 40 kg/m² * * Many of this patient group will already be eligible due to complications of obesity that place them in another risk category For further information, please see the influenza chapter in Immunisation against infectious disease (the Green Book), which is updated regularly. https://www.gov.uk/government/publications/influenza-the-green-book-chapter-19 3. What is flu? What is its impact on the population? Flu is a viral infection of the respiratory system (mouth, nose, bronchial tract, lungs). It occurs mostly in the winter and is passed from person to person through coughs and sneezes. For most people (including most children), it causes fever, headache, sore throat, joint pain and fatigue with recovery in two to seven days. However, for others, especially older people, infants, pregnant women, and people with underlying health conditions, it can cause serious even life-threatening complications and death. The impact of flu on the population varies widely from year to year and is difficult to measure. However, estimates considered by JCVI suggest that, on average, annually about 0.75 million people may consult their GP, about 27,000 people may be hospitalised and about 4,700 people may die in England because of flu. However, there is considerable uncertainty about these estimates and it is impossible to predict how many serious cases there will be next year. 4. I am pregnant. Do I need a flu vaccination this year? Yes, pregnant women are at increased risk from the complications of flu such as pneumonia. Having flu during pregnancy may be associated with premature birth and smaller birth weight so all pregnant women should have the flu vaccine to protect their unborn and newborn babies. The flu vaccine can be given safely at any stage of pregnancy, from conception onwards. Women should be offered the vaccine every time they are pregnant as the flu 32 virus constantly mutates and therefore the strains included in the vaccine are reviewed annually. Pregnant women benefit from the flu vaccine because it: reduces the risk of miscarriage or having a baby born too soon or with a low birth weight will help protect their baby who will continue to have some immunity to flu during the first few months of its life reduces their risk of serious complications such as pneumonia, particularly in the later stages of pregnancy will reduce the risk of the mother passing infection to the newborn baby will help protect any other children in the household. Talk to your GP or midwife if you want more information about the vaccination. 5. Do you have any targets for vaccine uptake this year? In 2014/15 it was our ambition that all eligible individuals are offered flu vaccine and that we reach a minimum 75% uptake for those: aged 65 years and over; and health and social care workers. This ambition continues for 2015/16. Again this year, for patients aged 6 months to under 65 in clinical risk groups, we are asking that GP practices and other providers prioritise improvements in vaccine uptake in those with chronic liver and neurological disease, including people with learning disabilities, who are at the highest risk of mortality from flu but have the lowest rate of vaccine uptake, and in pregnant women. In terms of the extension of the programme to children, there must be a 100% offer of immunisation to eligible children. A minimum uptake of 40% has been shown to be achievable in pilots conducted to date. We would expect uptake levels between 40 -60% to be attained. Uptake levels should be consistent across all across all localities and sectors of the population. 6. What were the vaccine uptake rates last year (2014/15)? This data is collected by PHE and is available at the following links. Vaccine uptake figures for patient groups in England, 2014/15 Vaccine uptake figures for healthcare workers in England, 2014/15. In summary for patient groups, flu vaccine uptake was generally similar to recent seasons (with the previous year’s figures [for 2013/14] in brackets) with the notable exception of an encouraging increase in pregnant women. Patients aged 65 or older: 72.8%, (73.2%) Patients in at risk groups: 50.3%, (52.3%) Pregnant women: 44.1%: (39.8%) Children aged 2: 38.5%: (42.6%) Children aged 3: 41.3%: (39.5%) Children aged 4: 32.9%: (N/A) 7. How many children were vaccinated in the pilots for primary school aged children in 2014/15? 33 Also in the 2014/15 flu season in England, vaccinations continued to be offered to some primary school-aged children in a cross-section of urban, rural and inner city settings in a series of pilots. For the first time, pilots for children in years 7 and 8 (aged around 11 to 13 years) took place in selected secondary schools around the country. Pilots for primary and secondary school aged children took place in Cumbria, Northumberland, Tyne and Wear Bury, Lancashire, Sheffield, Rotherham, Doncaster and Bassetlaw, West Yorkshire, Arden, Herefordshire and Worcestershire, Birmingham, Solihull and The Black Country, East Anglia, Leicestershire and Lincolnshire, Shropshire and Staffordshire, and in selected primary and secondary schools, and all special schools, across London. Overall uptake in these pilots was 53.2% - an increase over the level achieved in 2013/14 pilots of 52.5%. In Scotland, an uptake of 71.8% was achieved in all primary school age children, in Northern Ireland an uptake of 79.7% also in all primary school age children and in Wales, children aged 11-13 were offered vaccine, achieving an uptake of 74.3%. Encouragingly as a possible early indicator of the impact of vaccination of primary school age children, both Scotland and Northern Ireland experienced a shorter period of flu activity, with GP activity above baseline levels compared to England and Wales. 8. How many healthcare workers were vaccinated against flu? The uptake by frontline healthcare workers (reported by 100% of trusts) showed 54.9% were vaccinated, compared to 54.8% in the previous year, and a good increase over the 45.6% who were vaccinated in 2012 to 2013. However, the overall uptake level is still below the 75% aspiration and we know there is still scope for improvement. 34 CHILDREN’S FLU VACCINATION General Q&A 9. Which children will be offered the vaccine this winter? In 2015/16, all two-, three- and four-year-olds continue to be eligible for flu vaccination, through general practice, as are primary school-aged children in areas that participated in primary school pilots last year. In addition, local NHS England teams will commission the phase 2 extension of the programme to children of school years 1 and 2 age. Delivery models will vary by area, but are likely to be mainly through schools, for example, through school nursing teams or specialist immunisation teams, or in some instances through primary care services. A number of elements of the programme will be dependent upon local commissioning arrangements. 10. Why is flu vaccine being offered to healthy children? The Department of Health (DH), based on a recommendation received from the Joint Committee on Vaccination and Immunisation (JCVI) in July 2012, decided to extend the national flu programme to all children from the age of 2 to less than 17 years. Extending the programme to children will not only protect them from flu, but will also help to reduce the spread of flu and protect many others, such as younger brother and sisters, grandparents and those who are at increased risk of becoming seriously ill from flu. The programme is expected to appreciably lower the public health impact of flu by: preventing a large number of cases in children; lowering flu transmission in the community; and, reducing cases of flu infection in unvaccinated children, people in clinical risk groups and in older adults. It will reduce illness and death, reduce the demand for GP consultations, and hospital admissions. It will help keep people in work and is likely to be highly cost effective. 11. How and when will the full extension to the programme be delivered? This is an important addition to the national programme and is being carefully planned. PHE, NHS England and the Department of Health will work together to ensure that this programme is effective and sustainable, and is implemented as quickly and successfully as possible. 12. Why not vaccinate all children straight away? There would be significant implementation challenges associated with rolling out a full programme straight away. Since 2013, pilots have been allowing us to determine the best approach to implementing the programme for school-aged children, so that we can implement the programme safely, efficiently and sustainably, without putting pressure on other essential health services. 13. What about children aged under 2 years of age? The nasal spray vaccine is not licensed for children aged less than 2 years. As the effectiveness of other flu vaccines in very young children is uncertain, JCVI didn’t recommend that children younger than 2 years be part of the extended programme. However, if the extended programme reduces the spread of flu, young children will benefit from the reduced risk of being exposed to older children with flu (this is called indirect or herd protection). 35 14. What happens if my child turns 2 after the 31st August, but during the vaccination period (e.g. in October)? Will they still be able to get vaccinated? No. The vaccine is not licensed for those under the age of two because of a slightly higher risk of side effects, so in the interest of ensuring that vaccine is delivered as safely as possible, we are not recommending that healthy children who become eligible during the year are offered vaccination. So only children who are under two years on the 31 August and are in clinical risk groups who will be offered the inactivated vaccine 15. How often and when will children be offered flu vaccine? Once the programme is fully implemented, children will be offered the flu vaccine each year. This is because flu viruses can change annually so the vaccines are made each year to provide protection against the current circulating flu viruses. To be most effective the vaccine should be given in the autumn/early winter before flu starts to circulate in the community. 16. Will there be a second opportunity for children to be vaccinated? It is important that children in clinical risk groups are immunised for their own benefit to reduce their risk of morbidity and mortality associated with influenza infection. Every effort should be made to ensure all at risk children are immunised where appropriate. Once the first round of vaccination has occurred in all children in eligible school year groups, providers should target children in at risk groups who have not yet been vaccinated – to offer them individual benefit. Then, if considered necessary, a limited number of sessions for children who missed out on vaccination during the first round could be considered towards the end of the programme. Such arrangements would be for local determination, and subject to local commissioning agreement. 17. How many children will this affect? When fully implemented, the recommendation means that between nine and ten million children will be offered flu vaccine each year in England. 18. Will the vaccine be offered in schools for the full programme? Immunisation for children under school age (two to four years) each autumn will be delivered in general practice. Depending on local circumstances, some four-year-olds who have started school may be offered flu vaccination through schools. Children aged between 6 months and 2 years who are in clinical risk groups will also be vaccinated in general practice. JCVI have advised that the vaccine is likely to be most effectively offered to school-aged children in schools. This has been successfully done for other immunisation programmes (eg the HPV immunisation programme). We have successfully conducted pilots in some areas in 2013/14, and in 2014/15, to assess how effective it is to deliver in different locations, both in and out of schools, including in community pharmacies, to help with the long term planning of this programme. 19. Won’t delivering the programme through schools cause upheaval to school programmes and possibly damage children’s education? It is likely that the majority of vaccinations will be given in schools. We appreciate that delivering the programme through schools will involve children being away from lessons for a short time. However, for the individual child this should not be for a long period, as the vaccination itself only takes a few minutes. Successful immunisation of the child will help protect them and other children and staff in the school against flu. This in turn is likely to reduce sickness rates from flu and help children stay in school, improving their educational opportunities. 36 The local health service is already accustomed to working closely with schools to ensure the minimum disruption when delivering vaccinations, Local NHS England Teams and immunisation providers will continue to work with schools to minimise any disruptions caused by the flu vaccination programme. A number of schools involved in the pilots have also confirmed that the programme was of great benefit to them, with minimal disruption. Case studies have been made available. The Joint Committee on Vaccination and Immunisation (JCVI) Recommendation 20. What is the JCVI recommendation? JCVI – the independent expert committee that advises Government on immunisation – has recommended that the annual flu immunisation programme be extended to include all children aged two to less than 17 years. 21. Why did JCVI make this recommendation? The Secretary of State for Health asked JCVI to look at whether the annual flu immunisation programme, that has focussed on people who are particularly vulnerable to flu, should be extended to cover more people, including healthy people under the age of 65. JCVI carried out a comprehensive review of the evidence including on the health burden of flu on the population. This suggested that vaccination of school age children would have the most profound impact on the serious complications of flu. Extending the programme to healthy children should lower the potentially serious impact of influenza on those children. It should also reduce influenza transmission from children to other children, adults and those in clinical risk groups of any age. Vaccinating children against flu should therefore protect both children and their families and the wider community. 22. Does the Government have to accept the JCVI recommendation? Yes. Under the terms of the NHS Constitution, when the Secretary of State for Health asks JCVI to consider a new or changed immunisation programme and JCVI finds that to be cost effective and recommends it, the Secretary of State is obliged to implement the recommendation as soon as practicable. The vaccine 23. Which vaccine is being used to vaccinate children? The JCVI decision was based upon a programme using a live attenuated vaccine, given as nasal spray. This decision was based on evidence on the effectiveness of live attenuated intranasal vaccines in children and adolescents. Currently, the only live attenuated influenza vaccine on the market, Fluenz Tetra®, is manufactured by AstraZeneca. It is licensed for children aged two to less than seventeen years of age. A single dose of Fluenz Tetra® provides better protection to children than inactivated flu vaccine, and, as it is given by nasal spray, it is more acceptable to children than an injection. The vaccine has: high efficacy in children, particularly after only a single dose; potential to provide coverage against circulating strains that have drifted from those contained in the inactivated vaccine; higher acceptability of intranasal administration with parents, carers and children 37 it is likely to offer important longer-term immunological advantages to children by replicating natural exposure/infection to induce potentially better immune memory to influenza that may not arise from the annual use of inactivated flu vaccines. In addition to providing direct protection to children who are vaccinated, the full programme, by interrupting transmission of influenza, will reduce the spread of flu to unvaccinated children and adults, including those in clinical risk groups for whom flu can be extremely serious. Although the patient information leaflet provided with Fluenz Tetra® suggests children should be given two doses of this vaccine if they have not had flu vaccine before, JCVI considers that a second dose only provides modest additional protection. Therefore, JCVI recommends that children should be offered a single dose except for those in clinical risk groups aged 2 to less than 9 years old who have not received flu vaccine before and who should be offered two doses of Fluenz Tetra® (given at least four weeks apart). 24. Will all children be offered Fluenz Tetra®? Most children will be offered this vaccine. However, the nasal spray vaccine is not licensed for children aged less than two years and it is not suitable for a small number of children who have certain conditions (eg some forms of severe immunosuppression, those who are severely asthmatic, or those with severe egg allergy – see the Green Book chapter for details of precautions and contraindications (see: https://www.gov.uk/government/publications/influenza-the-green-book-chapter-19). They will be offered alternative, injectable vaccines. Children aged six months to less than two years of age in clinical risk groups will continue to be offered flu vaccine annually, but with an injectable vaccine. 25. Is the vaccine safe? The vaccine has an excellent safety record and has been used for over ten years in the USA without any serious concerns. Since it does not require an injection, it is more acceptable to children and parents alike. As with all live vaccines, it cannot be given to children with some clinical contra-indications (see above). Health professionals working on the programme will ensure that any contraindications and special precautions are observed. 26. How does the nasal vaccine work? The nasal vaccine contains viruses that have been weakened to prevent them from causing flu but still allow your child to build up immunity, so that when your child comes into contact with any circulating flu virus they are unlikely to get ill. Once a child has had the vaccine it is likely to take up to fourteen days for immunity to be established. 27. What are the side effects of the vaccine? Side effects are uncommon but may include a runny or blocked nose, headache, general tiredness and some loss of appetite. The vaccine is absorbed quickly so, even if your child sneezes immediately after having had the spray, there’s no need to worry that it hasn’t worked. 28. Can the vaccine give you the flu? The vaccine cannot give you flu. Fluenz Tetra® contains live but weakened forms of flu virus that don’t cause flu in those vaccinated. Sometimes people catch flu just before or soon after 38 the vaccine is given because the vaccine has not had the time to work. On these occasions people may think that the vaccine has caused the flu. 29. How many doses of vaccine are given? The patient information leaflet provided with Fluenz Tetra® suggests children should be given two doses of this vaccine if they have not had it before. However, JCVI considers that a second dose of the vaccine provides only modest additional protection. On this basis, JCVI has advised that, when extending the flu immunisation programme to children, most children should be offered a single dose of Fluenz Tetra®. However, children in clinical risk groups aged two to less than nine years who have not received flu vaccine before should be offered two doses of Fluenz Tetra® (given at least four weeks apart). Q: How effective is the vaccine? Because the flu virus can change from year to year there is always a risk that the vaccine does not match the circulating virus. During the last ten years the vaccine has generally been a good match for the circulating strains although last year it was not. 30. Can people opt-out? How would they do that? Yes. Vaccination is not mandatory. Parents and the older age groups of children will need to give their consent for the vaccination. However, immunisation is one of the most important weapons for protecting individuals and the community from serious diseases. The NHS constitution1 sets out your right to receive vaccinations recommended by the JCVI and encourages all to participate in vaccination programmers offered through the national immunisation programme. 31. My family don’t eat pork because of our beliefs. Can my children have the vaccine? PHE has responded to media reports about porcine gelatine used in vaccines, including Fluenz: https://www.gov.uk/government/news/vaccines-and-gelatine-phe-response Porcine gelatine has been certified as acceptable by many multi-faith groups. Gelatine is used to stabilise live viral vaccines and is contained in many pharmaceutical products, not just Fluenz. Public Health England (PHE) has previously published advice on our website from representatives of the Jewish and other communities regarding porcine or other animalderived ingredients in medicinal products such as vaccines. Rabbi Abraham Adler from the Kashrus and Medicines Information Service, said: “It should be noted that according to Jewish laws, there is no problem with porcine or other animal derived ingredients in non-oral products. This includes vaccines, including those administered via the nose, injections, suppositories, creams and ointments.” Dr Mary Ramsay, head of immunisation at PHE, says: “We strongly recommend that anyone whose child is offered immunisation accepts this opportunity to give their child the best protection possible against the flu virus. 1www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/dig italasset/dh_132958.pdf 39 This large programme has potential to protect children against the severe complications of flu and to reduce spread to more vulnerable people such as young infants, pregnant women, and those with underlying medical conditions.” Further information and links to FAQs for both parents and healthcare professionals can be found at the link above. 32. Is there an alternative to Fluenz Tetra®? The universal programme was recommended by JCVI on the basis of using the live attenuated vaccine to achieve a significant effect on transmission of influenza in the community. This is because a live attenuated vaccine offers better protection in children than an inactivated injectable vaccine, particularly after a single dose, and is easier to deliver as it is a non-injectable nasal spray. There is currently no alternative vaccine of equivalent efficacy that does not include porcine gelatine. For children with medical contraindications, inactivated injectable vaccine is a suitable alternative to provide individual protection (two doses will be required for those aged less than nine years of age who have not had a dose of flu vaccine previously). 33. Does this approach discriminate against people who refuse the vaccine because of the porcine gelatine content? The childhood flu programme using the nasal spray will help to protect everyone, vaccinated and unvaccinated, by reducing the spread of flu in the community. Unlike the programme for those in clinical risk groups, the programme does not only provide direct protection to each individual child. For example, healthy children aged under two years, in whom Fluenz Tetra® is not licensed, are not being offered inactivated vaccine – these infants will only be protected by reducing the risk of exposure from older children. Children who have clinical reasons for not receiving Fluenz Tetra® should be offered the injectable inactivated vaccine (with two doses if they have not had a dose of flu vaccine previously), in the same way as they would under the wider flu programme. Pilots 34. Are there any pilots being delivered in 2015/16? No, however areas that conducted pilots in 2015/16, are continuing to offer immunisation to children in their primary school classes in 2015/16. 35. What have you learnt from the pilots so far? Over the past two years the delivery of the programme to children has been tested in a number of areas. In those areas less flu has been detected in all age groups of the population. This suggests that as well as protecting the vaccinated children other people benefited too. A report “lessons learnt from the pilots and future planning” document has been shared with commissioners and their providers (sent out 17th June). A report detailing learning from the pilots will be available published on the Gov.UK website during summer 2015. 40 Q&A: HEALTHCARE WORKERS 36. Why is flu vaccine recommended for healthcare workers (HCWs)? Flu can be an unpleasant disease, even in healthy adults and for this reason many employers offer occupational vaccination. Healthcare workers have an additional duty of care to do everything in their power to protect patients against infection. This includes getting vaccinated against flu and other infectious diseases for example chicken pox and measles. The impact of flu on frail and vulnerable patients, in communities, care homes and in hospitals, can be fatal. It is therefore important that healthcare professionals are vaccinated. Frontline social care workers should also ensure that they protect service users from infection through having the annual flu vaccination. 37. Who is responsible for vaccinating health and social care workers? Responsibility for offering flu vaccination to frontline health and social care workers rests with their employers. Employers have a duty to carry out a risk assessment of each employee’s immunisation needs and make seasonal flu vaccine available free of charge to employees if indicated. Employers should ensure that there is sufficient vaccine and appropriate measure in place to deliver vaccination to those who should have it. Vaccination of HCWs not only offers protection to them and their families, but also reduces the transmission of infection to vulnerable patients. These workers should not generally seek vaccination through GPs (except for those with underlying risk factors for flu), as they will not have been included in GPs’ calculations of the number of doses of vaccines needed to meet their vaccinate their at-risk populations. 38. What evidence is there that vaccinating healthcare workers benefits patients/ the NHS? The effectiveness of flu vaccination in healthy adults is high (depending on the match with the circulating strains each year) and therefore, having the vaccine should prevent an unpleasant illness and reduce the risk of complications. There is good evidence from a number of studies that shows that vaccination of healthcare workers can also reduce flu-like illness (by as much as 50-76% in one study) and deaths in care homes and hospitals by preventing staff being a source of infection. There is also evidence that shows modest reductions in average absenteeism for flu like illness (0.5 days pa) in workers who have been vaccinated. In one London Trust, a study suggested that a proportion of the 11,000 days lost per year for colds and influenza like illness, could have been avoided through better flu vaccination uptake. Absenteeism is higher over winter and increased vaccination of HCWs can contribute to a reduction in absences due to flu-like illnesses. 39. Some say that vaccinating healthcare workers is a waste of time Evidence has shown that flu vaccination generally has a good efficacy record in healthy adults and that vaccination of HCWs can reduce flu-like illness and deaths in care homes and hospitals and lead to modest reductions in staff absenteeism, something which may be a key factor during the winter months when there is increased demand for health services. Despite the circulation of drifted strains in the 2014/15 flu season, flu vaccine is still the best protection we have against an unpredictable virus which can cause severe illness and deaths each year among at-risk groups, including older people, pregnant women and those with a health condition, even one that is well managed. 41 Throughout the last decade, there has generally been a good match between the strains of flu in the vaccine and those that subsequently circulate, so it’s important that healthcare professionals continue to be vaccinated in the future, and that we do all we can to ensure our patients in at-risk groups are not discouraged from having flu vaccination either. 40. Is vaccination of healthcare workers recommended internationally? Healthcare worker vaccination is clearly advocated as an important public health measure on the basis of current evidence by the World Health Organization, the European Commission, and Centre for Disease Control (USA). 41. How many healthcare workers were vaccinated last year? The uptake by frontline healthcare workers in 2014/15 (reported by 100% of trusts) showed 54.9% were vaccinated, compared to 54.8% in the previous year, and a good increase over the 45.6% who were vaccinated in 2012 to 2013. However, the overall level of uptake is still below the 75% aspiration and we know there is scope for improvement. How have you encouraged HCWs to get vaccinated against flu? As in previous years, work to encourage HCW’s to get vaccinated against flu has been undertaken by NHS Employers. They have: provided letters for trusts to circulate to frontline healthcare staff to encourage them to be vaccinated; run the ‘flu fighter’ programme, providing support, advice and guidance for flu leads across the NHS in running their local healthcare worker flu vaccination campaigns; produced specific staff-facing campaign materials, available to access via the internet, and provided a range of case studies, highlighting best practice from local flu campaigns across the NHS; To encourage this programme, CMO, CNO and CPhO wrote to the various professional bodies seeking, once again, their support for the programme to vaccinate HCWs. 42. Will you make vaccination of HCWs compulsory? Seasonal flu vaccination is not compulsory for health and care workers (HCWs). However, there are sound reasons why HCWs should be vaccinated, the most important being that is part of their duty of care to their patients or residents that they do everything in their power to protect them against infection. This includes getting vaccinated against flu. The impact of flu on frail and vulnerable patients, in communities, care homes and in hospitals, can be fatal and there is good evidence that vaccination of HCWs can reduce flulike illness and deaths in care homes and hospitals. It is, therefore, important that HCWs are vaccinated against flu - to protect their patients, their families and themselves. 43. How do you know how many HCWs are vaccinated? PHE collects monthly data on the number of HCWs that are vaccinated by location and by discipline and 100% of trusts reported their data in 2014/15. Uptake data by Trust has been published in a more high profile way so that Trust performance is much more visible. This will provide encouragement to those Trusts that need to improve vaccine uptake, acting as a further lever to improvement. 42 ANNEX 5: Resources 2015/16 The following resources are currently available to support local communications to healthcare professionals, parents, at-risk groups and schools. Further resources will be made available through issue of a marketing toolkit prior to the launch of the campaign, subject to approval of funding from Cabinet Office. 1. Information leaflets for pregnant women and all eligible patient groups that can be found here will shortly be updated for the 2015/16 season. 2. Resources for parents and schools have been made available, including: Immunising primary school children against flu: information for headteachers and other school staff Protecting your child against flu: information for parents* 5 reasons to vaccinate your child against flu poster* *Printed copies of this may be ordered from DH order line**. Orders will be recorded and fulfilled when copies are available in early June. Flu immunisation consent form Letter template to invite children in years 1 and 2 for flu vaccination (school based delivery) Letter template to invite all primary school aged children in pilot areas for flu vaccination (school based delivery) Letter template to invite children for flu vaccination (community based delivery) **Available via download or the DH/PHE Orderline: www.orderline.dh.gov.uk Telephone: 0300 123 1002 Minicom: 0300 123 1003 (8am-6pm, Monday to Friday) www.nhs.uk/vaccinations Further information and resources for the 2015/16 annual flu season can be found at www.gov.uk/government/collections/annual-flu-programme 3. Resources for healthcare workers are available on NHS Employer’s Flu Fighter website, and subject to funding will be updated for the 2015/16 flu season campaign. 43 Annex 6: Stakeholder mapping and analysis Stakeholder Engagement Coordination Plan For the delivery of the Annual Flu Programme 2015/16 Produced in partnership by PHE, DH and NHS England Contents 19. Background and purpose 20. Key Partners: Roles and responsibilities and current engagement 21. Key Stakeholders 22. Analysis 23. Annex A: Stakeholder analysis database and mapping 44 Background and purpose 1. The groups expected to be eligible for flu vaccination in 2015/16 are outlined below and any changes or additional groups to receive vaccination will be confirmed by the publication of the Green Book in 2015: those aged 65 years and over those aged 6 months to under 65 in clinical risk groups pregnant women children of school year 1 and 2 age primary school-aged children in geographical pilots that commenced in 2013/14 those in long-stay residential care homes adult and young carers healthcare workers 2. A wide range of stakeholders have influence on the delivery of influenza immunisation, either directly on those who will be vaccinated or on other parts of the delivery chain, such as with vaccine suppliers. 3. Eligible children: The annual flu immunisation programme is being gradually extended in line with recommendations for all children aged two to less than 17 years to be vaccinated. In 2015/16 the vaccine is going to be offered to children of school Year 1 and 2 age , meaning vaccination will be offered to all children aged 2 to 6. Vaccination will provide important protection to children, and offer indirect protection to people at high risk of complications from flu, including infants, older people, and those in high risk groups. 4. The extension of the programme to healthy children will present some new groups for stakeholder engagement. The delivery of the programme will be determined locally and it is expected that immunisation will be offered in schools in some areas, placing additional importance on engagement with education partners. Some 9 million children will be offered vaccination in a short window every autumn. To be effective, immunisation needs to take place between September and December and it is important that communications to all stakeholders (including education partners) are consistent, concise and timely. 5. It is also anticipated that there will be an increased influence of stakeholders who have previously not been as close to the delivery of flu vaccination, in particular: schools, likely to be the location of a high volume of vaccination; non-GP providers, including schools nursing service, private providers and community pharmacies; and Other Local Authority departments, in particular due to their interest in child health and well-being and the impact on schools and local communities. Public Health teams in LAs are already an established stakeholder. 6. This plan, accompanied by the stakeholder analysis (annex A) identifies stakeholders relevant to the programme and analyses the interest and influence of each one of them, each stakeholder has to communicate with their networks. The plan also provides a RAG rating for the current level of engagement that is carried out with these stakeholders by the various partner organisations responsible for the programme and identifies existing communications channels that can be utilised for the delivery of the 15/16 programme. 45 7. In order to ensure that engagement is well-coordinated, provides positive input to delivery planning, has positive impact and that messages used by partners with stakeholders are consistent. All key partners are asked to work together to: Contribute to stakeholder analyses to: o determine the current extent of engagement with individual or groups of stakeholders; o determine the likely influence and interest of specific stakeholders and agree the extent of engagement required with them; o determine which partner is best placed to engage with specific stakeholders; o determine how stakeholders will be engaged with and when; and o develop an overall plan that provides details on planned engagement. to ensure that stakeholder engagement is coordinated in a way that prevents duplication of effort, focusses on key stakeholders and ensures consistency of messages; to engage with stakeholder groups to Quality Assess messaging; to liaise with partners to monitor progress in stakeholder engagement activities; to engage with specific key stakeholders and make the most of their networks; and to ensure learning from engagement is captured and used to support implementation of seasonal flu and the extension to all healthy children. The stakeholder engagement coordination plan sits within the seasonal flu integrated communications strategy, and all messaging will be managed within that strategy. Delivery partners will be expected to feedback the results of their engagement in order to refine messages within this strategy and support the development of specific segmented messages for their stakeholder groups, as well as sharing learning to support implementation strategies. Key Partners: Roles and responsibilities and current engagement 8. We will work closely with our delivery partners to ensure that we are all aware of engagement activities and to plug gaps and avoid duplication. They include: Department of Health (and Department for Education [DFE]) NHS England (including NHS England Screening and Imms Teams) NHS Employers 9. Delivery partners have met already in 2014 to consider which stakeholders are relevant to the programme for 2015/16, and assess where engagement needs to be strengthened. 10. We will ask partners to share their organisation’s stakeholder engagement strategies with us where relevant. The following details have been gained regarding current stakeholder engagement activity carried out by partners (to note, DH, PHE and NHS England have central stakeholder engagement teams that can support policy, implementation and delivery): Stakeholder engagement activity Department of Health National: - Liaison with national strategic partners (eg DfE and other crossgovernment organisations) and facilitation of working-level engagement with operational deliver partners (ie PHE and NHS England). 46 - - - PHE Engagement with NHS England on the S7A deliverables and funding. Input into the Flu Project Board, representing DH policy. Lobbying and pitch-rolling policy and implementation plans with strategic partners where necessary. Access to cross-government partners comms routes (eg DfE stakeholder groups and comms with schools). Access to and potential use of the National Stakeholder Forum and the Social Partnership Forum. Deputy Chief Medical Officer engagement with national staff groups, such as the British Medical Association and the Royal College of General Practitioners. (DH Public Health Nursing Team) liaison with national professional staff groups and national professional networks, such as Royal College of Nurses, Community Practitioners and Health Visitors Association (CPHVA) and School and Public Health Nurses Association (SAPHNA) (with PHE and the Flu Project Board) – including using social media and webinars. (DH Public Health Nursing team) Liaison with national groups representing young people, such as the British Youth Council. Work with representative members of the Children’s Health and Well-being Partnership (Local Government Association [LGA] Society of Local Authority CEs [SOLACE], Association of Directors of Public Health [ADPH], Association of Directors of Children’s Services [ADCS]) National: - - - - National oversight of programme implementation through the monthly Flu Project Board. Working with DH to engage with cross-government stakeholders on implementation, using specific comms channels where relevant and feeding back stakeholder views to inform implementation. Responsible for developing and managing the Integrated Communications Strategy. Engagement with national staff groups (eg Royal College of Nursing [RCN]) to support implementation (with DH public health nursing team). Engagement with national charities supporting specific risk groups. Engagement with education partners through DfE (and regional PHE network). Engagement with national religious groups regarding vaccine content. PHE Press office – engagement with national specialist press to target segmented comms at specific stakeholder groups (eg Pulse, Jewish Chronicle). Engagement with vaccine producers and suppliers. Regional networks: - Direct contact with Screening and Immunisation Teams (SITs) that sit within Local NHS England Teams. 47 - - - NHS England Engagement with providers, through SITs in pilot areas. Engagement with local education partners. Support and guidance to SITs on managing local stakeholder engagement (including providing supporting comms packs, Q&A, leaflets, etc). Management of network of childhood flu pilots led by AT SITs (7 sites in 13/14), providing leadership, supporting and defining evaluation, providing technical implementation support. Engagement with and support to Directors of Public Health and wider health protection leadership through the Public Health England Centres National: - Engagement with DH on S7A deliverables and funding. Engagement with the Flu Project Board, representing commissioners and delivery planning and assurance. Engagement with the General Practitioners Committee of the BMA on national GP contracts (through NHS Employers). National engagement with Local NHS England Team to develop delivery strategies and to support implementation. Engagement with national level providers on direct commissioning solutions (eg Boots). National engagement with patient and public focus groups, as well as Clinical Commissioning Groups (CCGs), etc, though national stakeholder engagement teams. Regional networks: - - - - NHS Employers Through local NHS England teams, engagement with local healthcare providers to commission work (ie procuring services, managing, coordinating and supporting delivery). Through local NHS England teams, with local providers (including GPs, pharmacy), managing relationships with key local stakeholder (eg Local Authority Education Departments, schools). Through local NHS England teams – supporting local providers communicating with patients and the public. Through providers – e.g. school nursing professional leads and DSPHs. Through NHS communications teams supporting local NHS England teams – implement Integrated Communications Strategy locally. Engage with CCGs to encourage them to work with their GP practices to increase uptake/ reduce variation Engage with CCGs to develop local initiatives to increase uptake, where appropriate. National: - - On behalf of NHS England, NHS Employers with the GPC, negotiate national arrangements for vaccination and immunisation programmes and produce supporting guidance and national service specifications. Act as point of contact for vaccination and immunisation 48 - - - programme, guidance and clinical queries. NHS Employers chair and provide secretariat support to a General Practice Immunisation Group to support communication and resolution of operational matters that arise in the delivery of the national vaccination programmes. National staff-facing flu fighter campaign, encouraging improved uptake amongst healthcare workers through sharing good practice strategies and providing networking opportunities. Supporting employers to provide efficient Occupational Healthbased vaccination programmes for their staff. Wide contacts database with at least two contacts for every trust in England and Wales. Gathering and sharing good practice from trusts across England and Wales, breaking down geographical limitations for sharing information through networks and forums Key stakeholders 11. The full list of stakeholder, with analysis, can be found at Annex A. Stakeholders have been divided into the following categories: Government bodies and health/LG sector Local and regional NHS England/ PHE teams, local commissioners Local authorities Providers National staff representative bodies Professional bodies Unions Negotiating bodies Education Training and education provider Recruitment and staffing Faith group Patient representative group Voluntary organisation Carer Vaccine supplier Key stakeholders in each group are as follows: 12. Government bodies and health/LG sector Key delivery partners all sit within this group (including the devolved administrations) that is predominantly made up of national level strategic stakeholders, generally representing a particular sector. This group also includes partners that are involved in supporting flu immunisation through the Flu Project Boards, such as the MHRA. Key stakeholders that are provider sector representatives (Monitor, NHS Trust Development Authority) and central government bodies that have an interest in government spend and performance (HMT, MPA). 49 13. Local and regional NHS England/ PHE teams/ Local commissioners This section covers the various local teams responsible for commissioning, coordinating and supporting delivery of public health programmes, both within NHS England and PHE. It also includes Directors of Public Health and commissioners of public health for school aged children. They are responsible for ensuring programmes happen locally by managing local provider contracts and performance. Responsible for coordinating local communications with providers, as well as managing local stakeholder relationships (especially with schools and LAs), again with providers. local NHS England teams, and the various teams within them, are part of NHS England and have a key role in determining the extent and scope of implementation planning for childhood flu as well as developing implementation strategies, as they have the best understanding of local situations and therefore deliverability of plans. National engagement with these teams has been arranged on several occasions over the past year in support of childhood flu delivery, and more are planned. SITs and local NHS England teams have been managing pilots in primary and secondary school pilot areas since 2013/14 and are key stakeholders in developing planning to support implementation, including local comms strategies. 14. Local Authorities Details of national groups relating to local authorities or key staff within LAs, such as Directors of Children’s Services, Directors of Adult Social Services, etc. These stakeholder either have a direct role in supporting the extension of the flu programme to children, or are responsible for services where people in clinical risk groups are vaccinated (eg nursing homes). LAs also commission services where staff will need to be vaccinated to protect themselves and service users (eg social workers). DH is working with representative members of the Children’s Health and Wellbeing Partnership to establish the best mechanism for communicating with local authorities and how to provide further support. 15. Providers This group covers all providers likely to be vaccinating children as part of the programme. It includes NHS and non-NHS (private, not for profit, social enterprise) providers, as well as different types of provider, such as general practice, pharmacy, school nursing, immunisation teams, etc. Engagement will be around direct delivery of the programme (both seasonal and the extension to children), including messaging for professionals and patients, parents and the public. This group will also be engaged with on the requirement for healthcare providers to vaccinate front-line staff annually against flu. 16. National staff representative bodies This group covers all national staff bodies that have an interest in the delivery of the programme. The groups are predominantly healthcare focussed. Some of these groups are already represented in the Flu Project Board and are already engaged flu implementation, in particular RCN, SAPHNA and NHS Employers. Healthcare-focussed (including pharmacists) groups will be engaged to support delivery of childhood flu, in particular agreeing acceptable team skills mixes, training and support packages, etc. The staff they represent will also be key in supporting the rationale of the 50 programme with patients and the public, so messaging should be agreed nationally with them. They should also support direct comms to the staff they represent to improve uptake of vaccination amongst healthcare workers. 17. Professional bodies These include national healthcare professional bodies. These bodies will be engaged regarding specific concerns of staff regarding the delivery of the flu programme, therefore it is imperative that we engage with them carefully to understand needs and desires. They also have an interest and a role in training and professional development of staff, which is important particularly in the extension to children. Finally, it would be extremely helpful to get formal endorsements from them for programmes, in particular the extension to children and the vaccination of healthcare workers. 18. Unions As professional bodies above. 19. Negotiating bodies This section covers national bodies that negotiate with PHE, NHS England or DH on behalf of service providers. These groups can be key in developing and agreeing delivery solutions nationally (the GPC and PSNC) and locally. At local level, this includes local representative committees. 20. Education Teachers and other school workers will be a key part of delivery in many areas, as they will be required to support planning and delivery in schools and will be an important source of information for parents and children. Understanding their needs and how best to engage them locally can be supported through the national groups. DfE have suggested that we use their stakeholder groups such as Primary Head teachers Reference Group, Secondary Head teachers Reference Group, the Education Forum (this includes Unions, and local authority representation) and their Governors Group to review draft materials for schools, parents and children. The Flu Project Board will include an official from DfE who has links with key education stakeholder groups, and the Local Government Association are being approached to provide representative who can provide an education perspective to the Child Flu Immunisation Programme Board. 21. Training and education providers National and local providers of education and training. There have been many changes in national provision of training that need to be understood. Both short-term training and longerterm staff development will be key to supporting the extension of the programme due to its size. We will work with HEE to ensure appropriate representation within the workforce stream and ensure that we provide appropriate messaging to providers. 22. Recruitment and staffing bodies Organisations that can support the recruitment of sourcing of staff nationally and locally (eg bank staff). 51 23. Voluntary organisations A wide range of bodies that represent the needs and concerns of the people they represent. Key bodies are charities supporting specific clinical risk groups, or children and their parents included in the extension, and their communications networks. This also includes groups that have specific concerns regarding the programme, for example groups that have an interest in vaccine ingredients. 24. Carers Organisations that represent carers who are eligible for the vaccine (people who are receiving a Carer’s allowance, or who are the main carer for an elderly or disabled person whose welfare may be at risk if the carer falls ill). 25. Vaccine supply Includes vaccine manufacturers and vaccine supply partners. 26. Analysis method – as described above: Interest: 1 = low interest 2= medium interest 3= high interest 4= very high interest Influence: 1 = low influence 2= medium influence 3= high influence 4= very high influence Engagement required: 1 = inform 2 = consult 3 = involve 4 = partner 27. Delivery partners responsible for managing stakeholder relationships (as outlined in Annex A) will be asked to record any engagement activities carried out with these groups in the database. This is not intended to be onerous, but to allow an updateable central repository of engagement activity. Compilation and management of a central record will be carried out by PHE. 28. Stakeholder analysis and mapping is included in the spreadsheet below. Copy of Stakeholder analysis 31102014.xlsx 52