CarePlan_Template2030 Feb 4, nausea - VGH-care
advertisement

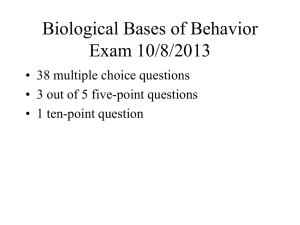
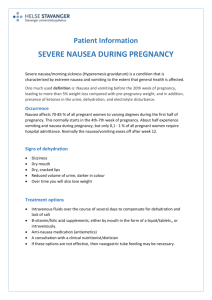
Date: Feb 4 Patient: Mrs S Room: 200-1 Age: Diagnosis: BCIT Level 2 Nursing Care Plan Treatments: PMHx: Medications: Diet: PRN Medications: Date of Surgery: Activity: Type of Surgery: Potential Problems What are the anticipated problems for this patient and what is potentially causing these problems. (due to or related to) Nausea ( actual) -due to medication -pain Nausea and vomiting - controlled by the vomit center (VC) in the medulla of the brain. GI sensory receptors send nerve impulses to the brain in response to abdominal distention/irritation. VC returns impulses that trigger abdominal contraction and reverse peristalsis-induce vomiting - Also triggered by unpleasant olfactory, visual stimuli, pain, emotional factors, ICP, migraine headache, inner ear - can also be stimulated when the CTZ is stimulated by drugs, chemicals, toxins, radiation, disease and VALIDATION PROCESS ASSESSMENT EVIDENCE Wednesday PM – How will Thursday PM – Data I assess each problem? collected to indicate a valid problem * assess History, duration,frequency, severity, precipitating factors, medication, measures used to alleviate the problem *Assess skin colour, pale/cool and clammy, green, temperature and moisture *Assess for loss of or decreased appetite *Assess bowel sounds x4 * Assess pt. for dehydration (ie, skin integrity, increased thirst, decreased urine output of <30cc/hr, increased respirations and heart rate, fatigue, dark coloured urine *Patient complains of nausea *Patient on narcoticshydromorphone, diclofenac Side effect-N&V * patient has lack of appetite * patient has not had bowel movement- on bowel protocol INTERVENTIONS Wednesday PM – What will I do for each of the potential problems – both nursing interventions and medical interventions? * Help Pt into a comfortable position (often side-lying) *small sips of water, ice chips, ginger ale * offer crackers * administer cold cloth * oral care to freshen mouth * ambulate –patient verbalized this was helpful * keep emesis basin within easy reach * instruct patient to change positions slowly -sudden or gross movements may increase nausea * Administer antiemetic as prescribed. Metoclopramide (maxeran) Dopamine antagonist: dopamine receptors in the CTZ and VC. Shortens the bowel transit EVALUATION/FOLLOW UP Thursday PM – What will I do Friday for each valid problem metabolic states During chemotherapy –release of serotonin from small intestine that stimulates NKI ((tachykinin neurokinin receptor found throughout central and peripheral systems and in gut) stimulates vomiting -increased activity of neurotransmitters – dopamine in CTZ and acetylcholine VCinduces vomiting *Assess pt. last dose of Anti-emetic and route given *Assess if pt. has excessive saliva due to nausea *Assess for reports of nausea *pulse rate, >100 beats/min, assess trend and baseline Acute Pain ( actual) *due to incision area *physiological stress increased cortisol * fatigue Continue to Assess Lotarp and Pain scale - Q1Hr Acute pain is frequently associated with anxiety and hyperactivity of the sympathetic nervous system Pain has sensory and emotional components Gate Control TheoryMelzack The interplay among these connections determines when painful stimuli go to the brain: 1. When no input comes in, the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is *Observe and monitor signs and symptoms – -Increased BP -Increased HR -Increased Temperature -Restlessness -Ability to focus -pupil dilation - Relief or distracting behaviour ( moaning, crying, restlessness) - pallor -Assess guarding behaviour – protecting body part *Patients report of pain *Assess last dose and frequency of analgesics and/or narcotics *Complains of pain in abdomen *on PCA weaned off time and in high doses blocks serotonin receptors (metoclopramide)., Gravol Antihistaminics with similar effects to the 5-HT3 receptor antagonists. Efficacy is through high concentrations of histamine and muscarnic cholinergic receptors within the vestibular system (dimenhydrinate) Will cause drowsiness. Patient need to ambulate. Not first choice. * give hydromorphone if Will choose Tylenol 3 Tylenol 3 is inadequate prn over plain Tylenol * Assess and document the intensity of the pain with each new report of pain and at regular intervals. - Systematic ongoing assessment and documentation provide the direction for pain treatment plans; adjustments are based on the client’s response. *warm blanket on abdomen – patient reported warmth aided in pain reduction * encourage patient to report increase or changes in pain level or location *Every q1hr, go into the room and observe for signs of increased HR, increased RR and restlessness * Prompt responses to complaints may result in decreased anxiety in patient - in the midst of pain, patient’s perception of time - if pain his higher than a closed). may be come distorted. 2. Normal somatosensory input happens when there is more large-fiber stimulation (or only largefiber stimulation). Both the inhibitory neuron and the projection neuron are stimulated, but the inhibitory neuron prevents the projection neuron from sending signals to the brain (gate is closed). 3. Nociception (pain reception) happens when there is more small-fiber stimulation or only smallfiber stimulation. This inactivates the inhibitory neuron, and the projection neuron sends signals to the brain informing it of pain (gate is open). Risk of Infection -Sarcoidosis -incision - high end white blood count (8.4) -malnutrition - chronic disease ( fibromyalgia) *Monitor WBC . * Assess for elevated temperature *Assess wound area and ensure that are is free from signs of infection - Redness -swelling -increased pain -purulent drainage from site * If there is any drainage it should be sent to lab for c&S - antibiotic therapy is determined by pathogens found *Encourage fluid intake of 200 ml per day of water - fluid promote diluted urine and frequent emptying of bladder; reduces stasis of urine -> reduces risk of bladder of infection or 3 Types -at risk -actual infection -sepsis shock death urinary tract infection *Assess appearance of urine - cloudy, foul smelling urine with visiable sediment is indicative of urinary tract infection or bladder infection * assess nutritional statuspatients may be anergic(lack of reaction by the body's defense mechanisms to foreign substances) and therefore more susceptible to infection - use of incentive Spirometer – shown yesterday but will go over again to make sure she is doing it properly -coughing -deep breathing Risk for pneumonia - post surgery -Sarcoidosis High end WBC- 8.4 Bacterial pneumonia is a lung infection caused by bacteria. The most common type of bacterial pneumonia is pneumococcal pneumonia. *Monitor wbc count *Monitor temp - increase? * assess hydration - Water loss is increased with fever Monitor oxygen saturation Symptomsa cough with rust *Ausculate lungs: listen for presence of adventitious or green-coloured phlegm sounds (mucus) high fever - Bronchial lung sounds (temperature often shoots up as high as 41°C (105°F) are commonly heard over areas of lung density or chills consolidation. Crackles are teeth chattering heard when fluid is present. chest pain *assess patient c/o chills *Assist patient with coughing, deep breathing, and splinting - improves productivity of cough *Encourage increased fluid intake 200 cc per hour -fluid are lost by fast breathing and heart beat bluish lips and finger nails from lack of oxygen in the blood feeling confused or strange feeling very tired ) * assess SOB Assess c/o of pleuritic chest pain ( pleura membrane irritated, rub together, nerve endings -> pain) diaphoresis, fever, tachypnea and are needed to mobilize secretions *Incentive Spirometer – improves deep breathing and prevents atelectasis 10x hour *Pace activities for patient with reduced energy *Provide oral care Secretions may cause nausea and vomiting *Consult respiratory therapist for chest physiotherapy and nebulizer treatment Discharge Planning How is she coping? What type of support does she have? What type of support does her husband have? Does she have a supportive friends that can come and help with household chores, making meals. Does she have someone to take her to all the appointments If she needs to go to the hospital will there be someone to take her if her husband is not able to? What does she do for self care? Taking time for herself?
![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)