Insurance Type is a Major Predictor of Lower Extremity Amputation
advertisement
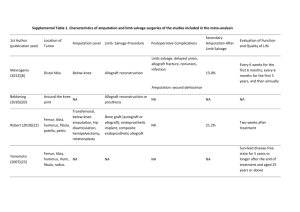
INSURANCE TYPE IS A MAJOR PREDICTOR OF LOWER EXTREMITY AMPUTATION FOLLOWING INFRAPOPLITEAL ARTERIAL TRAUMA John O. Hwabejire, MD, MPH; Augustine Obirieze, MBBS, MPH; Wendy R. Greene, MD; Weonpo Yarl, BS; Christine E. Nembhard, MD; Folake Kofo-Idowu, MD; David A. Rose, MD; Suryanarayana M. Siram, MD; Edward E. Cornwell III, MD, Kakra Hughes, MD. Howard University Hospital, Washington, DC. Introduction: The salvageability of the lower extremity after leg trauma with vascular compromise is often attributed to pathophysiologic and injury-related variables. We hypothesized that potentially modifiable factors influence salvageability following infrapopliteal arterial injuries. Materials and Methods: The National Trauma Data Bank research data sets, 2007-2010, were retrospectively examined. ICD-9 diagnostic codes 904.51, 904.53, and 904.50 were used to identify subjects aged ≥ 18 with tibial artery injuries. Subjects who died on arrival or in the Emergency Department were excluded. Demographic, injuryrelated, co-morbid, and other clinical variables were analyzed. The major outcome was lower extremity amputation. Univariate and multivariate analyses were done to determine predictors of amputation. Results: A total of 1921 subjects were included, with a mean age of 38 years in a primarily male population (82%). Whites comprised 58% and Blacks 22%. Insurance status included Private Insurance (24%), Self-Pay (20%), Medicare/Medicaid (17%), Other insurance types (14%), and “Not-billed-for-any- reason” (1%). About of 65% of cases were blunt injuries and 35% penetrating injuries. Mortality was low (2.5%), average ICU stay was 4 days, and average length of hospital stay was 15 days. Major lower extremity amputation was performed in 262 patients (13.6%): below knee in 10.6% and above-knee in 3.0%. Independent predictors of lower extremity amputation were Medicare/Medicaid insurance (OR:1.66, CI:1.03-2.66, p=0.039), Self-Pay (OR:1.76,CI:1.11-2.79, p=0.016), Other Insurance type (OR:1.61,CI:1.01-2.58, p=0.047), Not-billed-for-any-reason (OR:1.52,CI:1.01-2.28, p=0.043), Male Gender (OR:1.66,CI:1.11-2.34, p=0.012), and Injury Severity Score (OR:1.62,CI:1.02-2.38, p<0.001). Pre-existing conditions such as diabetes mellitus or peripheral vascular disease were not significant predictors of amputation. Conclusion: Insurance type is a major determinant of lower extremity amputation following infrapopliteal arterial injury. This study supports a growing body of evidence that trauma care and outcome are influenced by ability to pay and underscores the urgent need to escalate policy efforts to eliminate these inherent disparities.