MCQs in Rheumatology: Metabolic bone diseases
advertisement

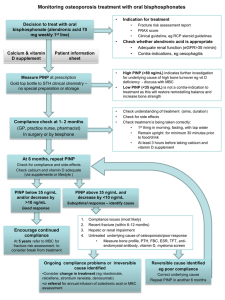
MCQs in Rheumatology: Metabolic bone diseases Contributors: These MCQs were written by Dr Zoe Paskins, Dr Michelle Hui, Dr Pravin Patil, and Dr Fran Rees, and were reviewed by Dr Ira Pande, and Dr Ed Roddy. The MCQs were edited by Dr A Abhishek who also facilitated the review process. www.rheumatology.org.uk/education Question 1 A 49 year old woman has been referred to the osteoporosis clinic for assessment of her fracture risk and advice on management. She fractured her ankle while skiing 6 months previously and has subsequently had a DEXA scan which shows her T score at the hip is -2.4. She had a menopause aged 41 which was not treated with HRT. There is no family history of osteoporosis but her mother fractured her hip aged 64. She is a vegan and takes no dairy products in the diet. She is a non-smoker and drinks one bottle of wine per week. Which of her risk factors is most significant for her fracture risk, independent of her bone mineral density reading? 1. 2. 3. 4. 5. Excessive alcohol intake Family history of fracture Low dietary calcium intake Premature menopause Previous low trauma fracture Question 2 A 63 year old lady is referred by her GP. She has been taking strontium for osteoporosis for 4 months and has a 5 day history of a widespread erythematous, itchy rash. Her GP has already stopped her strontium and checked her routine bloods which are normal. She is otherwise well. On examination, she has a macular papular erythematous rash, mostly over the trunk and back. Her vital signs are normal and rest of the examination is unremarkable (including chest, cardiovascular and abdominal examination). What is the most appropriate immediate course of action? 1. 2. 3. 4. 5. Antihistamines Drug washout High dose corticosteroids Low dose corticosteroids Restart strontium when the rash settles www.rheumatology.org.uk/education Question 3 A 74 year old woman is referred to osteoporosis clinic for advice on management of osteoporosis. She has a history of hiatus hernia, hypertension, hypercholesterolemia, chronic kidney disease stage 4 and COPD. She has recently been found to have osteoporosis after a Colles’ fracture. She is taking calcitriol, and other medication for her comorbidities. Based on the information above, which would be the most appropriate agent for treatment of her osteoporosis? 1. 2. 3. 4. 5. Alendronate Calcium and vitamin D supplements Denosumab Intravenous zoledronate Strontium ranelate Question 4 A 72 year old lady comes back to the osteoporosis clinic as a follow up. She has a history of postmenopausal osteoporosis and has had both vertebral and wrist fractures, although none in the last 3 years. Her DEXA scan shows the T score at spine is -4.2, a significant 6% deterioration since the last scan 2 years ago. She is currently treated with intravenous zoledronate, and calcium and vitamin D for last 3 years. Her bloods show serum calcium 2.15 (2.14-2.60), phosphate 0.8 (0.8-1.0) alkaline phosphatase of 110 (<120) and PTH 8.6 (6.1-8.1). What is the most appropriate immediate course of action? 1. Arrange blood test for magnesium 2. Arrange blood test for vitamin D 3. Prescribe teriparitide 4. Prescribe denosumab 5. Prescribe calcium and vitamin D www.rheumatology.org.uk/education Question 5 A 58 year old lady is referred to the osteoporosis clinic for investigation after a DEXA scan revealed her to have high bone density with a T score of +2.5 at the spine and +2.1 at the hip. She had this DEXA scan after she sustained a wrist fracture following a road traffic accident. She has no family history of fracture. She takes regular analgesia and is awaiting left hip replacement. Her dietary intake of calcium and serum biochemistry is normal. She weighs 75kg and is 1.6 m tall. What is the most likely explanation for her high bone density? 1. 2. 3. 4. 5. Obesity Osteoarthritis Osteomalacia Osteopetrosis Paget’s disease Question 6 A 28-year old female with SLE was referred for a second opinion. She feels tired all the time, and has difficulty climbing stairs, but is otherwise well. On examination, there is generalised myalgia. She has no synovitis, mouth ulcers or alopecia. Hb 11.1 g/dL, MCV normal, U&E normal, ALT 28 iu/L, ALP 180 iu/L (high), corrected calcium 2.08 mmol/L (low), phosphate 2.0 mmol/L (high) parathyroid hormone 37 pg/ml (high) ESR 8 mm/h, CRP <5 mg/L, CK 80 iu/L, ANA positive, dsDNA negative Which of the following is the most appropriate treatment? 1. 2. 3. 4. 5. Calcium 1,000mg and vitamin D 800 units PO daily Cholecalciferol 50,000 units PO monthly Hydroxychloroquine 200mg PO daily Parathyroidectomy Prednisolone 30mg PO daily www.rheumatology.org.uk/education Question 7 A 28-year old Asian female was referred for a second opinion. She gives a 1 year history of tiredness, aches in the thighs, and has difficulty climbing stairs. She has a vegetarian diet. On examination, there is evidence of proximal lower limb weakness grade 4 on the MRC scale. Recent investigations are as follows Hb 11.1 g/dl, U&E normal, ALT normal, ALP 180 iu/l (high), bilirubin 9 µmol/l, albumin 30 g/l, corrected calcium 2.08 mmol/l (low), ESR 8 m/hr, CRP <5 mg/l. Which of the following is the next most appropriate test? 1. Acetylcholine receptor antibodies 2. Anti nuclear antibodies 3. Creatine kinase 4. Muscle biopsy 5. Vitamin D Question 8 A 69-year-old man presented with a dull achy right shin pain. This was localised away from the knee, and was non-exertional. Musculoskeletal and general physical examination was unremarkable. A plain film of the knee, and the right leg was normal. The serum alkaline phosphatase checked by the GP was 300 IU/l (normal, 38 to 126 IU/l). Rest of the blood tests which included a FBC, UEC, CRP and ESR were normal. A 99m Tc- bone scan suggests Paget's disease of bone. Which one of the following is not an indication for drug treatment of Paget’s disease? 1. Hypercalcaemia 2. Asymptomatic Paget’s disease of the base of skull 3. Pain 4. Planned surgery near affected bone 5. Steadily rising alkaline phosphatase www.rheumatology.org.uk/education Question 9 A 45 year old Indian lady presents with widespread aches and pains. There is no history of sleep disturbance. On examination there is no evidence of synovitis. Fibromyalgia trigger points are negative. Investigations Calcium 2.01 mmol/L Vitamin D 15 mmol/L Alkaline phosphatase 260iu/L Serum creatinine 75 µmol/L Which of the following is the next most appropriate treatment? 1. 2. 3. 4. 5. Elemental Calcium 1 gram + cholecalciferol 800 IU/day Elemental Calcium 1 gram/day Calcitonin 100 IU/day Cholecalciferol 50, 000 IU/week Cholecalciferol 800 IU/day www.rheumatology.org.uk/education Answers: Q1. 2. Family history Her alcohol intake is not excessive. The previous fracture is unlikely to be a low trauma fracture as it was sustained during skiing. Low calcium intake and premature menopause though important, do not confer additional fracture risk in addition to bone mineral density. Maternal history of hip fracture increases the fracture risk 4fold. Q2. 1. antihistamines Although DRESS syndrome has been reported with strontium, this lady shows no signs of it. Guidance states that strontium should not be given again to anyone that has experienced a rash with it previously. Antihistamines would be appropriate for the treatment of the itch. Q3. 3. Denosumab Calcium and vitamin D supplements should not be given to someone with CKD stage 4, due to risk of hypercalcaemia. She is already on calcitriol. Of the other options, only denosumab is licensed for use in patients with eGFR <30ml/min. Q4. 1. Arrange blood test for vitamin D She has deteriorated on iv bisphosphonates. Before jumping to change therapy it is important to check there are no other secondary causes of bone loss first – her bloods suggest vitamin D deficiency. This should be treated (if present) before altering treatment. She may still have deficiency even on supplements and a blood test is required first to elucidate if she needs high dose replacement or standard maintenance dose. High PTH is a contraindication to teriparatide. Q5. 2. osteoarthritis Degenerative change commonly causes spuriously high BMD readings and this lady has OA hips. She is not obese by BMI and the affect of obesity on BMI is not clear cut. Osteopetrosis is extremely rare and Paget’s is unlikely in this age group with normal bone biochemistry. Q6. 2. Cholecalciferol 50,000 units PO monthly Patients with SLE and photosensitivity are advised to keep covered, and to use sunblock, so they are at risk of vitamin D deficiency. With these symptoms and biochemical profile, the patient will need high dose vitamin D replacement. Q7. 5. Vitamin D Risk factors, clinical feature and biochemistry are consistent with osteomalacia. PTH should be checked and is expected to be high as a result of negative feedback. Adequate vitamin D replacement usually leads to resolution of bone pain and proximal weakness within weeks. www.rheumatology.org.uk/education Q8. 5. Steadily rising serum alkaline phosphatase Paget's disease is usually asymptomatic and is frequently discovered incidentally. Mild-to-moderate, deep, aching bone pain, away from the joint (unless complicated by OA in the adjacent joint), characteristically begins late in the clinical course. Symptomatic (painful) disease is the most common indication for pharmacotherapy which has been shown to be effective. Rising alkaline phosphate level alone in an asymptomatic patient with Paget’s disease is not in itself an indication for treatment with bisphosphonates. This should be investigated further. Hypercalcaemia frequently occurs in the immobile. Asymptomatic involvement of the skull base should be treated as it may result in cranial nerve compression if the disease progresses. Michael P. Whyte, N Engl J Med 2006; 355593-600 August 10, 2006 Q9. 4. Cholecalciferol 50, 000 IU/week This patient has osteomalacia. Vitamin D may be replaced with high dose Vitamin D3 (Cholecalciferol). Ergocalciferol (Vitamin D2) requires to be further metabolized and is less potent than vitamin D3. Elemental Calcium 1 gram + cholecalciferol 800 IU/day does not contain enough Vitamin D3 to treat deficient levels. Calcium alone would not treat vitamin D deficiency, and calcitonin isn’t used to treat osteomalacia. However, practice may vary between units. www.rheumatology.org.uk/education