AUDITORY HALLUCINATION IN MR. A AT MENTAL HOSPITAL
advertisement
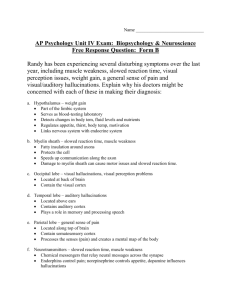
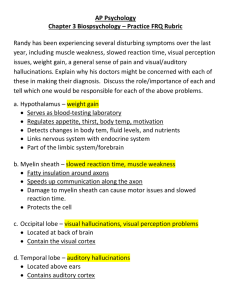
MANUSCRIPT CASE REPORT THE MANAGEMENT OF SENSORY PERCEPTION DISORDER: AUDITORY HALLUCINATION IN MR. A AT MENTAL HOSPITAL PROF. DR. SOEROJO MAGELANG By: SITI ATIQOH 0121668 NGUDI WALUYO NURSING ACADEMY UNGARAN 2015 THE MANAGEMENT OF SENSORY PERCEPTION DISORDER: AUDITORY HALLUCINATION IN MR. A AT MENTAL HOSPITAL PROF. DR. SOEROJO MAGELANG Siti Atiqoh (*), Abdul Wakhid (**), Wulansari (***) Nursing Academy Ngudi Waluyo Sitiatiqoh15@yahoo.com ABSTRACT Welfare soul becomes a determinant of health status of a person. In Indonesia there are 1.728 people who have disturbed soul welfare and have been diagnosed with a severe mental disorder. Of the mentioned amount, more than 90% of the clients experience hallucinations. The purpose of this writing is to examine the management of the disorder of sensory perception: auditory hallucination in Mr. A at Mental Hospital Prof. Dr. Soerojo Magelang. The technique used in data collecting was by interviewing, doing physical examination, and observating the patient's behavior. The method used to provide management for 2 days in Mr. A as an action to help the client to identify his hallucination, to help patient to control hallucinations by rebuking and taking medication. The results of the management from the implementation and evaluation of the patient obtained that the patient was able to control his hallucination with Sp 1 (rebuking) optimally and Sp 2 (taking medication) still with the guidance of a nurse. A suggestions for the hospital is to provide some examples about the description of the management of patients with mental disorders and they are provided in each room to provide deeper insight to the writen in the in the management of patients with impaired sensory perception: auditory hallucination. Keywords : auditory hallucinations, rebuke, taking medication INTRODUCTION Welfare soul becomes a determinant of health status of a person. In Indonesia there are 1,728 people who have disturbed soul welfare and have been diagnosed with a severe mental disorder. From the mentioned amount, more than 90% of clients have hallucination (Data Basic Health Research (RISKESDAS) (2013)). According to Joseph & Sutini (2009), in a mental hospitals Indonesia, approximately 70% of hallucination experienced by patients with mental disorders are auditory hallucinations, visual hallucinations 20% and 10% are hallucinations of smell, taste, and touch. The amount of the incidence of severe mental disorder, is still relatively high where the auditory hallucination dominates. Hallucination can be very worrying because it has negative impact on the client itself, do the others and the environment. Therefore, the writen in interested in performing management and more discussion about the process of managing disorders of sensory perception: auditory hallucinations. MANAGEMENT METHOD The method used was provide management for 2 days in Mr. A in the form of action to help the client to identify hallucinations, to help the patient to control hallucinations by rebuking and taking medication. The techniques used in data collecting were interview, physical examination, and observation of the patient's behavior. RESULTS MANAGEMENT From the results of the management of the implementation and evaluation, the patient was already able to control his hallucinations with Sp 1 (rebuking) optimally and Sp 2 (taking medication) still with the guidance of a nurse. DISCUSSION From the results of the assessment in Mr. A, the patient heard a male voice telling him to walk and prohibit to sleep. Basically the voice heard by the patient voice was only the sound or false perception because it was only experienced by patients, in which healthy people could not hear it. Patients who experience a false perception are those with impaired sensory perception. According to Maramis (2009) in Hindra, people who have impaired sensory perception are that they are experiencing an error in perception involving the five senses tools although they are not tied to stimulus from the outside but look so real for patients with schizophrenia. A false perception can occur because the patient can not distinguish between internal and external stimuli. Patients can not distinguish between a real stimuli and unreal stimuli. According to Moyet (2006), take sound or false perceptions can emerge due to secondary misinterpretation because of changes in sensory organs, neurological changes, metabolic changes, impaired oxygen transport. Besides secondary mobility limitations, due to paraplegia or quadriplegia, secondary misinterpretation (drugs, surgery), secondary misinterpretation due to pain or stress, social environmental restrictions, excessive noise, excessive activity, frequent demands, monotonous environment and loss of socialization can also affect the occurrence of false voices heard by patients. According to Ngadiran (2010) in Fa'izah (2013) false perceptions can emerge after a hostile relationship, stress, isolation, useless, hopeless, and helpless feeling. Mr. A experienced hostile relations with his neighbors because of the exhaust of motor, felt not able to support his family, and his relationship with his girlfriend was not approved by his mother, so that these conditions are triggered the patient to experience a disorder in determining the sensory perception. The patient heard the false sound when the patient was alone and before going to bed. According to Twistiandayani and Widati (2013), this perception can arise due to lack of stimulus environment around the patient. Patients often feel lonely so that the patient is not able to create a positive stimulus to the environment. After the assessment, the data will be analyzed to determine the nursing diagnoses. For the case of Mr. A, the writer raised the diagnosis of a disorder of sensory perception: auditory hallucinations. According to Kusumawati (2010) in Rahmawati (2014), hallucination is the loss of the human ability to distinguish internal stimuli and external stimuli. Hallucinations experienced by a patient characteristics. According Twistiandayani and Widati (2013) the forms of hallucinations that occur can be noises or buzzing that may affect the client's behavior, such as talking to himself, fighting and other harmful responses-responses, as well as the responses shown by the patient are pacing and irritability. The writen raised the diagnosis of sensory perception: auditory hallucinations because the data obtained both subjectively and objectively showed that Mr. A showed the characteristics of experiencing hallucinations. According to Moyet (2006), the problem of sensory perception disorders can be enforced if there are major characteristics of sensory perception disorders: hallucination is inaccurate interpretation of environmental stimuli and / or negative changes in the number or pattern of coming stimuli, then the defining characteristics are minor disorientation of time , people, and places, changes in behavior or communication patterns, hallucinations to hear or see, changes in the ability to solve problems, anxiety, sensitive to stimuli, poor concentration. The next step was the preparation of interventions which refer to the general purpose (TUM) and Special Purpose (TUK). In general, the preparation of intervention aimed to protect the patient from possible risk of injuring himself and others. According to Rasmun (2009) in Fa'izah (2013) the rational of building mutual trust is as the basic therapeutic interaction between nurses and clients. Next intervention was to help the client to recognize his hallucinations. The ways to do that: were are observation of behavior associated with the client’s hallucinations, identification of contents, the triggered circumstances, time and frequency of hallucinations experienced by the client. When the nurse and the client have already know the experienced hallucinations, this will facilitate nurses in determining interventions that should be developed. According to Rasmun (2009) in Fa'izah (2013) the rationale of the action was that the active participation of the client determined the effectiveness of nursing actions performed. Further intervention, was by explaining and training the client to control hallucinations, namely: rebuking, by taking medicine, chatting and doing activities. The aim was that the client was able to control hallucinations and the rational was a common action of the client as an attempt to overcome hallucinations (Rasmun (2009) in Fa'izah (2013)). And for the last intervention was the collaboration with the family in supporting the client’s healing client, to encourage families to always provide support to control his hallucinations when the client had gone home. Rasmun (2009) in Fa'izah (2013) stated this important intervention aims to provide clients with the support of the family in controlling hallucinations, the rational family is able to care for clients with hallucinations while in the house. Once the intervention is determined, the next step is by implementing interventions that are suitable and followed by evaluation. The implementation was carried out in Mr. A was by doing Sp 1 (trained to control hallucinations by rebuking). The rebuke was done by expelling the coming noises. According to Anggraini (2013) rebuke is one attempt to control hallucinations by rejecting appeared hallucinations. Rebuke can be taught by nurses in the management of patients with impaired sensory perception: auditory hallucinations. According to Anggraini (2013) rebuke can be done in 2 ways by covering ears and without covering ears. Both methods have proven capable to derease the level of hearing hallucinations experienced by patients. Rebuke can be done by rejecting the coming noise. According to Twistiandayani and Widati (2013) rebuked technique is called as thought stopping as one example of cognitive behavior in psychotherapy technique that can be used to help the client to change thought processes it is. Done by saying stop and expelling the hallucinations. The basis of this technique is to consciously ask himself to, "stop!", While experiencing negative over and over, is not important, and distorted thoughts . Then replace the negative thoughts with other thoughts which are more positive and realistic. At the first meeting the patient, was taught Sp 1, because the hallucinations of the patient still often appeared and the patient could not perform the way to rebuke. After Sp 1, the evaluation process was obtained in which the patient was able to rebuke optimally and independently. Currently the second meeting, the nurse did Sp 2 (train control hallucinations by taking medication). Sp 2 was done because the patient was able to perform Sp 1 optimally , thus continued by Sp 2. The rational of this ability to take medicine to reduce the patient’s anxiety and to reduce the risk of the emergence of hallucinations. According to the standard of nursing care at Mental Hospital of Prof. Dr. Soeroyo Magelang, to take this medication Sp was implemented by discussing the benefits, disaduarages of not taking medication, name, color, dose, method, therapeutic effects and side effects of using drugs. Medication onedience supports the recovery of a patient, a nurse must monitor and discuss properly to the patient. According to Keliat in Kaunang, Kanine and Kallo (2015) a client with mental disorders (schizophrenia) is usually difficult to follow the rules of taking drugs because of the reality and the inability to take decisions. The evaluation process was obtained from the second meeting that the patient had not been able to control hallucinations to take medication in an optimal way. Guidance as well as assistance in taking medication still need to be done. CONCLUSION After assessment in auto and allo anamnesis, the data obtained that the Patient often heard a male voice telling him to pace and forbid to sleep when bedtime and alone. The male voice came over 15 minutes, missing, then appearing again. The client folt disturbed and sometimes the client responded the voice grumpyly. Where the sound can not be heard by healthy people. From the results of the assessment, the data obtained from the patient can be used as supporting data in diagnosing disorders of sensory perception: auditory hallucinations. And the data used in this diagnosis are correct theoretically. Major and minor characteristics mentioned in theory are partly suitable with the assessment of the patient in the outcome data. The writer gave nursing action plans (interventions) in order for the patient to control his hallucinations by teaching Sp 1 (rebuke) and Sp 2 (taking medication). Implementation was done for 2 days and based on the interventions that had been drawn up by teaching the patient Sp 1 (rebuke) and Sp 2 (taking medication). The result was that the patient was able to control hallucinations using Sp 1 optimally and Sp 2 still with the help of nurses, so that the outline of the process of managing Mr. A’s results was suitable conformity with the objectives and met the criteria of the desired results of the writer. BIBLIOGRAPHY Anggraini, Karina. (2013). Pengaruh Menghardik Terhadap Penurunan Tingkat Halusinasi Dengar Pada Pasien Skizofrenia Di RSJD DR. Aminogondohutomo Semarang. 18 Mei 2015. http://pmb.stikestelogorejo.ac .id/ejournal/index.php/ilmukepera watan/article/viewFile/176/20 0 Badan Penelitian dan Pengembangan Kesehatan Kementrian RI. (2014). Hasil RISKESDAS 2013 Provinsi Jawa Tengah. 14 April 2015. http://www.depkes.go.id/reso urces/download/general/Hasil %20Riskesdas%202013.pdf Carpenito, L. J. & Moyet. (2006). Buku Saku Diagnosis Keperawatan Judul Asli: Handbook Of Nursing th Diagnosis, 10 Ed. Alih Bahasa: Yasmin Asih. Jakarta: EGC. Dermawan, D., & Rusdi.(2013). Keperawatan Jiwa Konsep dan Kerangka Kerja Asuhan Keperawatan Jiwa. Yogyakarta: Gosyen Publishing. Dinas Kesehatan. (2013). Profil Kesehatan Kota Semarang 2013. 14 April 2015. http://www.dinkeskotasemarang.go.id/?P=hala man_mod&jenis=profil Direja, Ade, H, S. (2011). Buku Ajar Asuhan Keperawatan Jiwa. Yogyakarta: Nuha Medika. Fa’izah, Siti. (2013). Studi Kasus Asuhan Keperawatan Pada Tn. I Dengan Gangguan Persepsi Sensori : Halusinasi Pendengaran Di Ruang Abimanyu Rumah Sakit Jiwa Daerah Surakarta Program Studi Diploma III Keperawatan Sekolah Tinggi Ilmu Kesehatan Kusuma Husada Surakarta 2013. 18 Mei 2015. http://www.academia.edu/58789 28/STUDI_KASUS_ASUHAN_ KEPERAWATAN_PADA_TN._ I_DENGAN_GANGGUAN_PE RSEPSI_SENSORI_HALUSINA SI_PENDENGARAN_DI_RUA NG_ABIMANYU_RUMAH_S AKIT_JIWA_DAERAH_SURA KARTA_PROGRAM_STUDI_ DIPLOMA_III_KEPERAWATA N_SEKOLAH_TINGGI_ILMU_ KESEHATAN_KUSUMA_HUS ADA_SURAKARTA_2013 Fitria, Nita. (2010). Prinsip Dasar dan Aplikasi Penulisan Laporan Pendahuluan dan Strategi Pelaksanaan Tindakan Keperawatan (LP dan SP) untuk 7 Diagnosis Keperawatan Jiwa Berat bagi program S-1 Keperawatan. Jakarta: Salemba Medika. Hindra, Kukuh.n.d. Bab ii Tinjauan Pustaka. 18 Mei 2015. http://digilib.ump.ac.id/files/d isk1/20/jhptump-ump-gdlkukuhindra-951-2-babii.pdf Kaunang, I., Kanine, E. dan Kallo, V. (2015). Hubungan Kepatuhan Minum Obat Dengan Prevalensi Kekambuhan Pada Pasien Skizofrenia Yang Berobat Jalan Di Ruang Poliklinik Jiwa Rumah Sakit Prof Dr. V. L. Ratumbuysang Manado. 18 Mei 2015. http://ejournal.unsrat.ac.id/in dex.php/jkp/article/download/ 8196/7753 Keliat, B. A., Panjaitan, R. U., dan Helena, N. (2005). Proses keperawatan kesehatan jiwa. Edisi 2. Jakarta: EGC. Nisa’, Hilyatun. (2012). Asuhan Keperawatan Pada Nn. Z Dengan Gangguan Persepsi Sensori: Halusinasi Pendengaran Di Ruang Sembadra Rumah Sakit Jiwa Daerah Surakarta. 18 Mei 2015. http://eprints.ums.ac.id/20610 /12/11._NASKAH_PUBLIK ASI.pdf Nisa’, R. R. (2013). Asuhan Keperawatan Pada Ny. S Dengan Halusinasi Pendengaran Di Ruang Sembadra Rumah Sakit Jiwa Daerah Surakarta. 18 Mei 2015. http://eprints.ums.ac.id/25747 /12/NASKAH_PUBLIKASI. pdf Prabowo, Eko. (2014). Konsep & Aplikasi Asuhan Keperawatan Jiwa. Yogyakarta: Nuha Medika. Rahmawati, Yeni. (2014). Asuhan Keperawatan Pada Ny. L Dengan Gangguan Persepsi Sensori: Halusinasi Pendengaran Di Ruang Srikandi Rumah Sakit Jiwa Daerah Surakarta. 18 Mei 2015. http://eprints.ums.ac.id/30925 /21/NASKAH_PUBLIKASI. pdf Rumah Sakit Jiwa Prof. Dr. Soeroyo Magelang. (2009). Standar Asuhan Keperawatan. Twistiandayani, Retno dan Widati, Amila. (2013). Pengaruh Terapi Tought Stopping Terhadap Kemampuan Mengontrol Halusinasi Pada Pasien Skizofrenia. 18 Mei 2015. http://download.portalgaruda. org/article.php?article=98548 &val=426 Videbeck, S. L. (2008).Buku Ajar Keperawatan Jiwa, Jakarta: EGC. Yosep, I., & Sutini, T. (2009). Buku Ajar Keperawatan Jiwa Dan Advance Mental Health Nursing. Bandung: PT Refika Aditama. Yosep, Iyus. (2009). Keperawatan Jiwa, Edisi Revisi. Bandung: PT Refika Aditama.