Schizophrenia and Substance Use Disorders
advertisement
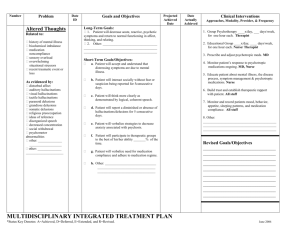
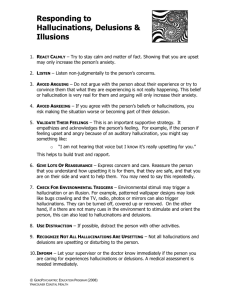
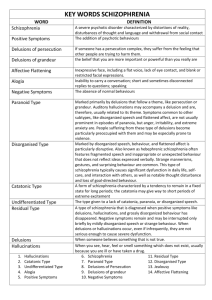
Schizophrenia and Substance Use Disorders How do Thought Disorders and Substance Use Disorders Interact? Topic Areas I. Description of Thought Disorders II. Influential Factors on the Illness III. Effect of Substance Use IV. Implications for Recovery I. Description of Thought Disorders How is it decided if someone has a “thought disorder?” Diagnostic Criteria for Schizophrenia* A. Characteristic symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month period: (1) delusions (2) hallucinations (3) disorganized speech (4) grossly disorganized or catatonic behavior (5) negative symptoms, i.e., affective flattening, alogia, or avolition B. Social/occupational dysfunction: One or more areas of functioning such as work, interpersonal relations, or self care are markedly below the level achieved prior to the onset. C. Duration: Continuous signs of the disturbance persist for at least 6 months. E. The disturbance is not due to the direct physiological effects of a substance or a general medical condition. * Diagnostic and Statistical Manual, 4th Ed. (2000). American Psychiatric Association. Arlington, VA. p. 312 Diagnostic Criteria for Schizoaffective Disorder* A. An uninterrupted period of illness during which, at some time, there is either a Major Depressive Episode, a Manic Episode, or a Mixed Episode concurrent with symptoms that meet Criterion A for Schizophrenia. B. During the same period of illness, there have been delusions or hallucinations for at least 2 weeks in the absence of prominent mood symptoms. C. The disturbance is not due to the direct physiological effects of a substance, or a general medical condition * Diagnostic and Statistical Manual, 4th Ed. (2000). American Psychiatric Association. Arlington, VA. p. 323 Diagnostic Criteria for Substance-Induced Psychotic Disorder* A. Prominent hallucinations or delusions. B. There is evidence from the history, physical examination, or laboratory findings of either (1) or (2): (1) the symptoms in Criterion A developed during, or within a month of, Substance Intoxication or Withdrawal (2) medication use is etiologically related to the disturbance D. The disturbance is not better accounted for by a Psychotic Disorder that is not substance-induced. * Diagnostic and Statistical Manual, 4th Ed. (2000). American Psychiatric Association. Arlington, VA. p. 342 Terms and Definitions “Positive” symptoms (“in addition to” what was experienced before the illness) include; – Delusions – Hallucinations (Auditory, Visual, etc.) – Disorganized Speech – Bizarre Behavior Terms and Definitions “Negative” symptoms (“taken away from” what was experienced before the illness) include; – – – – – Alogia Affective Blunting or Flattening Avolition Anhedonia Attentional Impairment Delusions False beliefs Affects the “Inference” system of the brain (ex.) “Conspiracy theories” are common Hallucinations False perception Affect the “Perception” system of the brain Auditory hallucinations are most common Any of the 5 senses may be involved Disorganized Speech Affects the “Language” system of the brain (ex.) Word salad is a jumble of words/phrases that lacks comprehensible meaning; (ex.) Tangentiality is a style of speech in which a person replies to questions in an irrelevant, “off the topic” manner). Bizarre Behavior Affects the “Behavior-inducing” systems of the brain (ex.) Ritualistic behaviors – may represent “normal” responses to the “abnormal” stimuli of active delusions or hallucinations Alogia the inability to organize one’s thoughts and express them fluently Affective Blunting or Flattening “Flat affect” A deficiency in the ability to express a full range of emotion May be expressed in a monotonal voice, a “poker face,” or a “schizophrenic stare” Avolition The inability to initiate a behavior, or carry it out (exs.) Withdrawal, apathy, decreased energy, decreased motivation Anhedonia The inability to experience pleasure or enjoyment May result in the discontinuation of hobbies or recreational activities Attentional Impairment Difficulty in focusing attention Can lead to inability to complete tasks or activities that require focused attention II. Influential Factors Family History (Genetic) Factors Individuals with schizophrenia are more likely to have relatives with psychiatric illness (or substance use disorders) Indicates a genetic vulnerability to psychiatric illness (and substance use disorders) Supersensitivity Model Biological vulnerability + environmental stress = precipitate the onset of the disorder or trigger relapses Medications decrease vulnerability Substance use increases vulnerability III. Effect of Substance Use Alcohol Use Combining Alcohol and antipsychotic medication can cause life-threatening oversedation Cocaine Use Cocaine abuse can damage the brain and cause psychotic episodes to occur Marijuana Use Marijuana use can contribute to the frequency and intensity of psychotic episodes – More severe positive symptoms – Quicker psychiatric relapses & re- hospitalizations – Earlier age of onset IV. Implications for Recovery Special Considerations More likely to develop addiction with recreational use. Many clients report using substances to facilitate social interactions with peers. Principles of Integrated Treatment* Integration Comprehensiveness Assertiveness Reduction of Negative Consequences Long-Term Perspective Motivation-Based Treatment Multiple psychotherapeutic modalities * Mueser, K.T. et al. (2003). Integrated Treatment for Dual Disorders. Guilford Press: Canada. p. 16-33