Reply to reviewer`s report Date: Comments sent in by reviewer: 23
advertisement
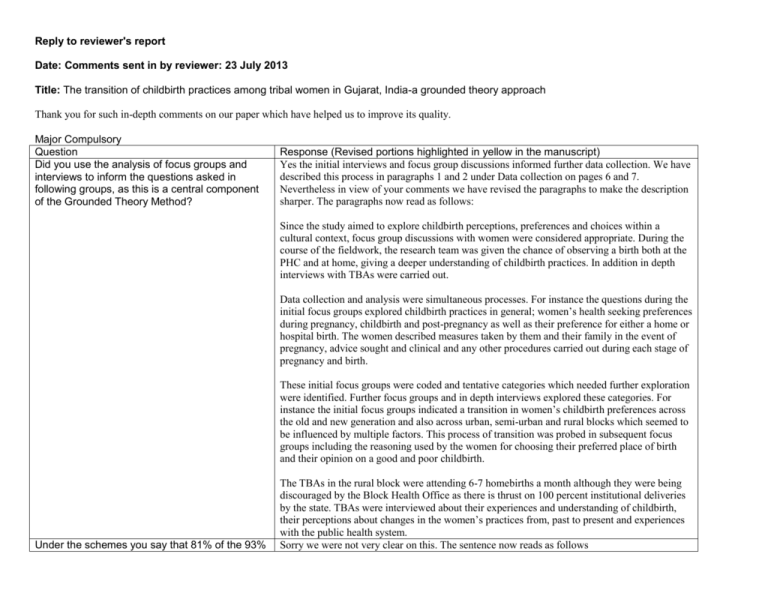
Reply to reviewer's report Date: Comments sent in by reviewer: 23 July 2013 Title: The transition of childbirth practices among tribal women in Gujarat, India-a grounded theory approach Thank you for such in-depth comments on our paper which have helped us to improve its quality. Major Compulsory Question Did you use the analysis of focus groups and interviews to inform the questions asked in following groups, as this is a central component of the Grounded Theory Method? Response (Revised portions highlighted in yellow in the manuscript) Yes the initial interviews and focus group discussions informed further data collection. We have described this process in paragraphs 1 and 2 under Data collection on pages 6 and 7. Nevertheless in view of your comments we have revised the paragraphs to make the description sharper. The paragraphs now read as follows: Since the study aimed to explore childbirth perceptions, preferences and choices within a cultural context, focus group discussions with women were considered appropriate. During the course of the fieldwork, the research team was given the chance of observing a birth both at the PHC and at home, giving a deeper understanding of childbirth practices. In addition in depth interviews with TBAs were carried out. Data collection and analysis were simultaneous processes. For instance the questions during the initial focus groups explored childbirth practices in general; women’s health seeking preferences during pregnancy, childbirth and post-pregnancy as well as their preference for either a home or hospital birth. The women described measures taken by them and their family in the event of pregnancy, advice sought and clinical and any other procedures carried out during each stage of pregnancy and birth. These initial focus groups were coded and tentative categories which needed further exploration were identified. Further focus groups and in depth interviews explored these categories. For instance the initial focus groups indicated a transition in women’s childbirth preferences across the old and new generation and also across urban, semi-urban and rural blocks which seemed to be influenced by multiple factors. This process of transition was probed in subsequent focus groups including the reasoning used by the women for choosing their preferred place of birth and their opinion on a good and poor childbirth. Under the schemes you say that 81% of the 93% The TBAs in the rural block were attending 6-7 homebirths a month although they were being discouraged by the Block Health Office as there is thrust on 100 percent institutional deliveries by the state. TBAs were interviewed about their experiences and understanding of childbirth, their perceptions about changes in the women’s practices from, past to present and experiences with the public health system. Sorry we were not very clear on this. The sentence now reads as follows of birth occurring in institutions occurred in private hospitals while 45% occurred in the public sector (page 13). The numbers do not add up here and so this needs to be looked at. but also what are the differences in the intervention rates between the private and public services and discussion about the impact of essentially privatising maternal health care needs to be included. Later on, on page 22 you say women of higher socioeconomic status were more likely to use oxytocin but this may be more to do with private obstetrics in private hospitals than women’s request. Page 14 breech presentations - is not spelt breach Page 16 when you say a “stable plus a trusted Auxillary Nurse Midwife” do you mean permanent. Not sure what is meant by stable? According to the statistics provided by the District Health Office (not validated), out of 93% births in institutions, 81% occurred in the private sector out of which 45% occurred in CY enrolled facilities which were private facilities approved under the CY scheme (Table3). Our response to this is as follows: We agree that C-sections and privatization is important but we feel it is a bit out of the scope and objectives of our study? We have not quantified respondents’ experience of delivery i.e. the number of home and institutional deliveries but focused more on their perceptions. Moreover the information on differences in intervention rates; complicated births and Csections (Is that what you refer to?) between private and public sector is not readily available as part of the information system of health system. It is only available as part of the National Family Health Surveys. We have mentioned inequitable distribution of health professionals and health centres skewed toward developed areas in several places in the paper. In-spite of all these government schemes for maternal health like JSY and CY including the emergency ambulance service which are utilizing the private sector, things do not change for the better in underserved areas like the rural block in our study, because of un-availability of obstetricians both in the private and public sector. This comes from another study quoted in the paper. The study is used to support the category “hospital births as progressive”. Oxytocin has become a routine procedure in all hospitals whether private or public in India. In fact oxytocin is also being used (misused) in home deliveries in some provinces as given on page 23 Our study shows that women think any modern medical procedure including the use of oxytocin is their right because they want the best state-of- the- art treatment. The women also want to follow the modern trend. Therefore as seen in the quote given on page 18 and 19 women see the use of oxytocin (injection, drip) as part of their conceptualizations of ‘good’ childbirth. Thanks we have made the correction. By stable here we meant permanent, available round the clock. This is very rare in the rural areas today. Most of the appointed midwives do not live at their headquarters due to several reasons. We have changed the word to permanent to avoid confusion. Page 16 I have rephrased this sentence Thanks it reads much better “This socialization got further embedded when there was evidence that women who had hospital births were benefiting from the successful handling of life threatening complications. “ Page 18 where you describe fundal pressure We found that traditionally in home deliveries, when a woman is in active labour and is about to occurring both at home and in the hospitals (a dangerous traditional practice) it is interesting to note that medical professionals have incorporated this traditional practice into their care. Was there any evidence that this link between the two was reassuring for women? However, in the paragraph below this is a qote saying this fundal pressure did not happen anymore and hence there was less incontinence as a result? Can you clarify this conflict? In several places you have run the words do and not together to make donot you also join other words together such as come new I think it is important to make the point that similar strategies in Developed nations have been employed in the past to move birth from home to hospital and writers such as Margie Tew in the UK have challenged the resulting outcomes in books such as Safer Childbirth. In the UK the Peel report in 1970 recommended all women have their babies in hospital without evidence to support this practice and virtually eliminated homebirth overnight and now the efforts of the government to increase homebirth are slow and except for Wales where homebirth is up to 10% rates remain low. Also in much of the Western world there is now a resurgence back to a primary health care, midwife led and community based approach to care. There has also been a doubling of homebirth in countries such as Australia and the USA in recent years and increasing moves in countries such as the UK and New Zealand to small standalone midwife led units in the community. The recent Place of Birth study showing that midwife led units separated from hospitals had the best outcomes for mothers and babies. It is ironic that we seem unable to get the balance right in history. The investment in medical models at the expense of midwifery models of care despite strong World Health Organization support is a common problem in the developing world and leads to deliver; TBAs were applying ‘Kalla’ (external fundal pressure) to help her in delivering baby easily. Some of the women shared their own experiences, while some shared their observations when accompanying their relatives for delivery in hospital and they found that even in hospital external pressure was given by nurses/doctors. The difference between the two was that in institutional delivery the practice of giving oxytocin has replaced the need for external fundal pressure in the minds of the women as given in the quote on page 18 and 19. The women express that though fundal pressure is given by the staff in the hospital it is of much lower intensity (just a gentle push) compared to what was given by the TBA in old times, because oxytocin (or the drip) compensates for external fundal pressure. Thanks to bring it to our notice. We have made the changes This is exactly the focus of the current paper. It is a complex issue with no clear answers. We partly agree to this argument against hospital births but beg to differ on the grounds of different situations in the developed and developing countries. When we talk of poor women and their choices in the developing countries such as India, homes are not like the homes in the UK or New Zealand. Homes of poor families can be dusty, with no facility of adequate clean water round the clock. With lack of water it is difficult to maintain aseptic precautions. In addition to the poverty of homes there is also unavailability of professional care at home, assurance of quick transport when emergency arises. The women in our focus groups have understood all these issues and therefore accepted hospital births. You are right when you say that a good alternative would be community based midwifery services close to the woman. India made a beginning after independence when they recruited and trained Auxiliary Nurse Midwives (ANMs) for 2 years and posted them in the subcentre (a health centre with basic facilities for BEmOC for every 5000 population). But with the pressure to stabilize population growth and control communicable diseases such as malaria, TB, Childhood diarrhea and pneumonia, these ANMs were converted to Multi-purpose workers which took away from them their core role that of maternal and child health services. We have revised the discussion on page-20 paras 2 & 3 to make this more clear. We have also revised the paragraphs on page 24. We agree with this completely. This is what we argue for when we conclude by the need to invest in midwives and when we discuss the “loss of community self reliance” unnecessary intervention and other resulting problems from this. Some critique about this will strengthen the paper. I cannot see where you give a definition of an allopathic hospital Page 23 you discuss the policy of giving TBAs oxytocin to manage the third stage of labour but go on to describe that high dosages cause hyper stimulation etc but this is only when used during 1st and 2nd stage of labour. So are you saying this was misused beyond 3 rd stage? We give it now on page 6, 2nd paragraph in parenthesis The authority to use oxytocin has been given to the Auxiliary Nurse Midwife with 18 months formal education. She is different from the TBA who is a lay woman who learns childbirth as an apprentice to her mother or mother-in-law who is experienced. Yes oxytocin is misused to hasten contractions in the 2nd stage of labour. The paragraph has been revised as follows to avoid confusion. Oxytocin has been freely available as part of the Skilled Birth Attendant policy of the Government of India [50]. The Auxiliary Nurse Midwife also known as the Female Health Worker at peripheral institutions were given permission and training to inject oxytocin as part of managing the third stage of labour to prevent postpartum haemorrhage (PPH), one of the leading causes of maternal deaths in India. Question: You describe attending a birth at home with a TBA and one in hospital. I could see no evidence this informed the study and a small case study on each would have been so interesting. No limitations are described and this is important. However as described in this and other studies oxytocin is used during the 2nd stage of labour also to shorten the duration of labour. This may not really reduce maternal deaths. High dosages create hyper stimulation, which can lead to precipitate labour, perineal tears, uterine rupture and fetal distress [51]. Observations of home and hospital births gave us an opportunity to contextualize women’s experiences of home delivery and those who had institutional delivery. We could empathize with women’s experiences of delivering whether at home or at an institution. We could not include case studies because we focused more on model development using grounded theory. Case studies would have been a different style of presentation of the results. We have described methodological limitations in the last paragraph on page 7 where we discuss difficulties in restricting the numbers of women in each focus group and retaining the same participants from the beginning to the end separating older and younger women The same have been discussed on page 19 and 20 under “discussion” in paragraph 2. We have added some more limitations in the beginning of the discussion