the Oxytocin PowerPoint Presentation Here
advertisement

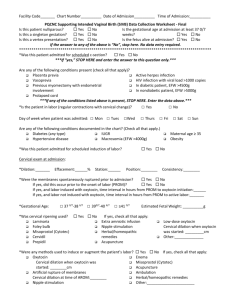
Guidelines for Oxytocin Shared Quality Initiatives in Obstetrical Care The Obstetrical Society of Philadelphia Deborah A. Driscoll, MD November 17, 2012 Background In 2008 UPHS Ob service established an interdisciplinary work group to develop a standardized protocol for oxytocin use • Rationale: – Protocols for oxytocin use were inconsistent across the health system. – Paid claims often allege oxytocin misuse. – Recent studies suggest that implementation of a uniform specific checklist-based protocol improves newborn outcome and decreases overall adverse outcomes, and can reduce claims (Clark et al. 2007; 2008). – Meta-analysis demonstrated that low dose protocols result in fewer episodes of hyperstimulation, higher rate of vaginal birth, less post-partum hemorrhage and maternal infection (Crane 1998). 2 UPHS Oxytocin Protocol Checklist based protocol for administration of oxytocin for induction or augmentation of labor was introduced in summer 2009 at HUP. • • • • Ob providers evaluate indication for oxytocin use, maternal and fetal status, and complete PreOxytocin checklist Nursing assessment recorded every 30 minutes using Oxytocin checklist Specific recommendations for: – Recurrent decelerations – Oxytocin-induced tachysystole with reassuring FHR tracing Triggers to notify Ob provider to reevaluate plan of care Deviation from the protocol requires Ob provider documentation in the chart including justification. Protocol was modified after 4 month pilot and then introduced at PAH. 3 HUP Experience Collected data for 14 months pre- and post-implementation • Pre: 1/08-3/09 and Post: 1/10-3/11 5077 of 8717 women received oxytocin Results: • Time of admission to delivery among those who received oxytocin – median admission to delivery increased in the postimplementation group (534 vs 466 min, p<0.001) • Cesarean delivery rates – 18.1% vs 19.3%, p=0.28 Challenges and Controversies Fall 2012 - Work Group convened to review experience and consider modifications to protocol. 4 Guiding Principles for Administration of Oxytocin Attending physician must be present in the hospital FHR and uterine activity will be monitored electronically Oxytocin solution should be given in pre-mixed piggy back infusion Pre-Oxytocin checklist should be completed prior to initiation If criteria are not met then discuss management plan, document deviation from protocol High or low dose oxytocin regimens are appropriate (ACOG Practice Bulletin 107, 2009) If prostaglandin used for cervical ripening then oxytocin should not be initiated sooner than 4 hrs after last misoprostol or 1 hr after removal of dinoprostone Follow NICHD FHR interpretation guidelines and adjust oxytocin infusion according to the Oxytocin Maintenance Checklist Dosages > 20mU/min require patient reevaluation and notification of provider Maximum infusion rate 40mU/min, notify provider after 2 hrs If at any time team is not in agreement then initiate chain of command 5 Perspectives on Ob Guidelines Engage your providers in guideline development and implementation – build consensus early in the process Take an interdisciplinary approach Involve residents in the process Collect and share data Assess the impact Review guidelines on a regular basis and modify as needed Be open to learning from others – value your colleague’s perspective and experience These guidelines should not be construed as dictating an exclusive course of treatment. Deviation should be appropriately based on needs of the individual patient and documented in the medical record. 6