Doctor`s Point of View for Life Support It is common knowledge that
Doctor’s Point of View for Life Support
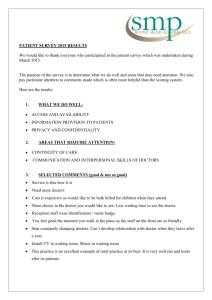
It is common knowledge that the role of doctors is to do anything in their power to keep their patient alive. But what if the family of the patient does not want to keep the patient alive?
Will the doctor just cut the life support without any moral obligations? What if the patient had a chance of recovery? The ethics behind continuing life support cause a controversy between the doctors, patients, and the family members of the individual on a financial and moral basis.
The patient’s view on life support is entirely dependent upon their will to survive. The individual may wish have to determine whether it is best to cut life support so the family does not have to see his/her inevitable death from a terminal illness or injury, or to agree to stay on life support for a slight chance of miraculous recovery.
The family’s view depends on their financial status as well as their love for the family member. If they cannot pay to see the patient on life support for days and even up to months, then it is in the family’s best decision end the procedure and say goodbye to their loved one. But if they cannot bear to see the specific family member go, then they will have to pay for it.
My personal reaction about life support is to inform the doctors about initiating discussions with patients and families facing end-of-life choices. A Stanford University study showed that almost 90 percent of doctors would forgo resuscitation and aggressive treatment if facing a terminal illness (Stanford Medicine). In the past, if doctors knew that the procedure was very likely to not be successful, they were responsible to tell the family the news that the patient will face death soon, but could still live as long as the life support can help. Now, the decision to tell the family when the doctor also finds out benefits both parties. Not enough doctors are trained to talk about death with patients, which may be why some doctors wait to tell families.
“[They’re] trained to prolong life” (npr). In the end, any course of action doctors take on this
situation, the blame will be on them because their point of view might be different from the media’s or the family’s point of view.
Some of these situations from the doctor’s perspective can be considered violations.
People right now only tolerate it because they know and understand that doctors are trained professionals and are reliable. Morally, if the doctors decide to not tell the status of the patient to the family of the individual on life support until the end, then they will feel blame on themselves.
But if they decide to tell the family when they find out, more benefits are open for both financially and morally. These actions are justified because in some cases, only the doctors know what will happen to the patient instead of the family.
Since doctors do not realize the outcome talking with the family has, some actions to take now for the doctors are to just conference with the family before and during the procedure.
Both parties will know the different situations that will happen to the patient such as making a recovery with time or not, and will put less ethical violations on the doctor. A system should be created to punish doctors who do not disclose everything to the family immediately. This way, the patient and family can feel secure knowing that the doctor is not only trying to cater the interests of the family, but also so the doctor can be morally reasonable for the accountability of the patient.
Works Cited
O'Neill, Stephanie. "Knowing How Doctors Die Can Change End-Of-Life
Discussions." NPR . NPR, 6 July 2015. Web. 11 Nov. 2015.
White, Tracie. "Most Physicians Would Forgo Aggressive Treatment for Themselves at the End of Life, Study Finds." News Center . Stanford Medicine, 11 Feb. 2013. Web. 11 Nov.
2015.