Practice Visit Agreement - Council of Medical Colleges
advertisement

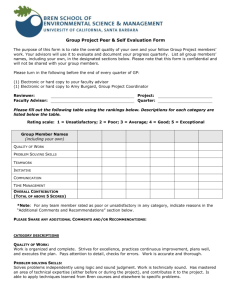
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists New Zealand Practice Visit Visitor Kit for Dr XX For the Practice Visit of: Dr XX – “date” Important note: Practice visits are undertaken under the College’s Protected Quality Assurance Activity Notice. This means that the process is completely confidential. The Royal Australian and New Zealand College of Obstetricians and Gynaecologists The Royal Australian and New Zealand College of Obstetricians and Gynaecologists RANZCOG, New Zealand Office | PO Box 10611 | Wellington 6143 t: +64 4 472 4608 | f: +64 4 472 4609 | w: http://www.ranzcog.edu.au/ 2 © Copyright RANZCOG Table of Contents Page Purpose of the Practice Visit 4 Section 1 Instructions Pre-visit 5 The day of the practice visit 6 Post visit 11 Section 2 Documentation received from visitee Timetable for the day of the practice visit Pocket 1 Timetable for interviews with visitee’s colleagues Pocket 2 Practice Profile Questionnaire & Self Assessment Survey Pocket 3 Patient Satisfaction Questionnaire Report Pocket 4 Weekly theatre lists for three month period Pocket 5 Section 3 Forms to be completed and returned by the visitor by the deadline Practice Visit Agreement Pocket 6 Visitor Assessment Survey Pocket 7 Expense Reimbursement Claim Form Pocket 8 3 © Copyright RANZCOG Purpose of the Practice Visit Fellows of RANZCOG are able to receive a practice visit as part of their continuing professional development. The visits are designed to provide Fellows with a confidential review by two of their peers in relation to various aspects of their practice. The practice visit process also incorporates interviews with the multidisciplinary team the Fellow works with, as well as a review of the clinical works load, case mix and record keeping. Confidentiality – Protected Quality Assurance Activity The practice visit process is a protected quality assurance activity under a formal notice obtained by RANZCOG. This means that all information that becomes known solely as a result of the practice visit process is strictly confidential. RANZCOG has obtained a notice from the Minister of Health protecting the confidentiality of the process, with the objective of encouraging fellows to participate fully and frankly in the practice visit process. It is important that you know that it is an offence under the Health Practitioners Competence Assurance Act 2003 to disclose information that comes to light during the practice visit process outside the College’s processes. There are some exceptions to this, but they are limited. If you are requested to provide information about the practice visit process you must check with the Executive Officer, RANZCOG, before providing such information. Aim of the Practice Visit The aim of the practice visit programme is to provide feedback about the practice and facilitate quality improvements where necessary, in a collegial and supportive manner. Objectives of the Practice Visit Objectives of the practice visit are as follows: To improve the practices and competence of fellows by assessing the health services performed by them To improve outcomes for patients Practice visits are not intended to be used as a mechanism for investigating concerns that have been raised about a fellow’s competence, health or fitness to practise. Where there are such concerns other mechanisms are available. RANZCOG will endeavour to ensure that practice visits are not set up in such situations. However, if you are aware that there are serious concerns that have been raised about the fellow please inform the Executive Office, RANZCOG immediately, and prior to commencing the practice visit process Outcomes of the Practice Visit Contribute to the delivery of safe, quality healthcare outcomes for women, their families, health professionals and the broader community. 4 © Copyright RANZCOG Section 1: Instructions Pre-visit The day of the Practice Visit Post visit 5 © Copyright RANZCOG Pre-visit instructions 1. Read the documentation provided in this kit 2. Meet with the other visitor prior to the practice visit to review schedule and documentation provided by the visitee. This can usually be done the evening before the day of the practice visit. 6 © Copyright RANZCOG The day of the practice visit – instructions The practice visit will take most of one day per visitee. The practice visit will include the following components; 1. An initial interview with the visitee (one hour) 2. A review of the practice surroundings, equipment and processes (30-60 mins) 3. Review of 10 randomly selected obstetric and gynaecological case records 4. A patient consultation (30 mins) 5. Interviews with the visitee’s colleagues (15 mins each colleague) 6. Observation in theatre (2 hours) 7. Concluding interview (30-60 mins) Practice visit schedule The visitee has provided a schedule for the day of the practice visit. Please find a copy of the schedule in Pocket 1 Guidelines To obtain the best results from the practice visit, it is important that the visitors act in a supportive, helping role. The initial interview provides the opportunity for the visitors to establish rapport and credibility with the visitee. Throughout the practice visit, visitors should: explain the process and clarify the visitor’s role allay concerns when they arise ask open questions and let participants tell their story summarise what has been said Instructions for each component of the practice visit 1. Initial interview with the visitee (one hour) Discussion during the initial interview should cover the following: a) Discussion around the confidentiality of the practice visit, and ensuring understanding of what the protected quality assurance activity protections mean. 7 © Copyright RANZCOG b) Discussion regarding aspects of the Practice Profile Questionnaire c) Comments on the Patient Satisfaction Questionnaire Report d) Review of theatre lists from the previous 3 months e) Review of the Self-assessment Survey analysing the visitee’s rooms and practice f) Any surgical complications over the previous two years g) Discussion regarding medical disciplinary issues over the previous two years. These discussions should include ACC cases, Health and Disability Commissioner cases and also Medical Council and Disciplinary Tribunal cases. h) Discussion regarding personal life and health issues 2. Review of the practice surroundings, equipment and processes This should take approximately 30-60 minutes and will include a review of record systems. A worksheet has been provided as a guide and to record information. This can be found in the Visitor Assessment Survey Pocket 3 3. Review of 10 randomly selected obstetric and gynaecological case records These should include cases from both private and public practice where possible. A worksheet has been provided to record impressions. This can be found in the Visitor Assessment Survey Pocket 3 4. Patient Consultation A review of the doctor/patient relationship is an important component of the practice visit process. A 30 minute consultation will be organised with a patient who has provided written consent for one of the visitors to be present throughout the consultation. Ideally this will be a new gynaecological patient. A worksheet is provided to record impressions and can be found in in the Visitor Assessment Survey Pocket 3 5. Interviews with visitee’s colleagues A schedule of interviews has been provided by the visitee and can be found in in the Visitor Assessment Survey Pocket 2. The interviews are possibly the most important part of the practice visit process. They will include a number of key people who work closely with the visitee, e.g. a nurse manager, clinical director, anaesthetist, paediatrician, midwifery manager, theatre staff, registrars and administrative staff. 8 © Copyright RANZCOG The interviewees will have been briefed about the practice visit process by the visitee. Each interview should take approximately 15 minutes, and sometimes more than one visitee will be discussed in one session. A worksheet of questions is provided in Pocket 7 6. Observation in theatre During a two hour period in theatre, the visitors will observe the visitee performing a major and a minor surgical procedure. Visitors should not assist with the surgery. Permission from the hospital and/or patient may be required, so please check with the visitee. A worksheet to record observations is provided in in the Visitor Assessment Survey Pocket 7 7. Concluding interview The concluding interview is a very important part of the practice visit process and should take between 30-60 minutes. Impressions and feedback from each area of the visitee’s practice that has been assessed during the day should be shared and any positive and negative aspects discussed. It is essential that any areas of vulnerability are discussed at this time. The visitee should be informed that a report will be written following the practice visit which will be submitted to the RANZCOG NZ Practice Visit Sub-committee in December, and a formal letter from the chair of the sub-committee will then be sent to the visitee. The visitee should be advised that they will be credited with 25 Practice Review and Clinical Risk Management (PR&CRM) points and a certificate will be sent to them at the conclusion of the process. The visitee should be thanked for their time and effort involved in arranging the day’s activities. 9 © Copyright RANZCOG Post visit instructions Following the practice visit, the visitors should work together to prepare a draft practice visit report which will be submitted to the RANZCOG NZ Practice Visit Sub-committee for review in December. A letter from the chair of the sub-committee based on the practice visit report will then be sent to the visitee. The following documentation must be completed and returned to the RANZCOG NZ Office by the deadline: 2 November 2015 1. Practice Visit Agreement 2. Visitor Assessment Survey 3. Practice Visit Report Follow-up Survey As part of the evaluation process, a brief survey will be sent to all visitors approximately six weeks after completion of the annual programme,. It is hoped that all visitors will take the time to complete and return this survey so that the practice visit programme can be continually evaluated and improved where necessary. A similar survey will be sent to the visitees also. Reporting Template A template for the practice visit report is provided. An electronic version is available from the RANZCOG NZ Office on request. Please note that the report is strictly confidential and will be reviewed by the RANZCOG NZ Practice Visit Sub-committee. A letter based on the report will be sent to the visitee, signed by the chair. A template for the report follows. 10 © Copyright RANZCOG In the formal assessment section there are sections (a) to (h) to incorporate into the report. Written responses to these components will be drawn from observation and review of the visitor and the visitee’s documentation. With regard to the section headed Recommendations, this section is designed to capture recommendations that will inform the continuous quality improvement of the visitee’s practice. In this regard we ask that in putting forward recommendations, the focus be on quality improvement initiatives in relation to the practice. The visitee may be offered a follow up practice visit to assist further change and improvements. Please note that the recommendation section is optional. 11 © Copyright RANZCOG Reporting template Confidential: Prepared under RANZCOG’s Protected Quality Assurance Activity Notice Practice Visit by Dr <Name of Visitor 1> and Dr <Name of Visitor 2> Name of visitee and place of work You have a (e.g. mixed general obstetric and gynaecological specialist workload) in (e.g. both the public and private) sectors and are developing a special interest in e.g. laparoscopic surgery). You have been in the post (number of) years. The (Name of Hospital/Place of Work) group consists of (1, 2, etc) part time O&G consultations working an identical on call roster. The weekly roster consists of (e.g. one fixed day per week on call (resident 0800 – 1700), one antenatal clinical (whilst on call adjacent to the Delivery Unit), one gynaecological clinic and one theatre list. In total 20-24 hours, plus call.) Formal Assessment: Please comment on the following: (a) Surgical Logbook: (b) Patient Satisfaction Review: (c) ACC/HDC/Medical Council: (detail any complaints or enquiries pending). (d) Continuing Professional Development (note if requirements are up to date). (e) Communication: Report on the visitee’s communication skills with staff and patients. (f) Surgery: Make comment on the visitee’s performance in the operating theatre and (g) Clinical notes: Comment on the quality of the records reviewed (private and public, (h) Clinical surroundings: Provide feedback on the appearance and functionality of the Refer to the Patient Satisfaction Questionnaire summary communication with surgical nursing staff paper and electronic) including back-up, legibility etc rooms and whether they appear to be well maintained and fit for purpose. 12 © Copyright RANZCOG Strengths: Please note strengths you have observed in the visitee and their practice. Please consider organisational skills, professional performance, personal integrity and approach to clinical audit. Areas of Vulnerability: Please note any areas of vulnerability or risk. Please consider record keeping, communication, workload, work balance etc. Recommendations: Please note any recommendations that will inform the continuous quality improvement for the visitee’s practice. 13 © Copyright RANZCOG Section 2: Documentation from visitee Timetable for the day of the practice visit Pocket 1 Timetable for interviews with visitee’s colleagues Pocket 2 Practice Profile Questionnaire & Self Assessment Survey Pocket 3 Patient Satisfaction Questionnaire Report Pocket 4 Weekly theatre lists for three month period Pocket 5 14 © Copyright RANZCOG Name of Visitee and date of Practice Visit: 15 © Copyright RANZCOG Section 3: Documentation to be submitted by deadline: 2 November 2015 Practice Visit Agreement Pocket 6 Visitor Assessment Survey Pocket 7 Expense Reimbursement Claim Form Pocket 8 Practice Visit Report 16 © Copyright RANZCOG Practice Visit Agreement Thank you for agreeing to be a visitor as part of the Practice Visit Process. As a visitor you are acting on behalf of the Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Purpose of the Practice Visit Practice Visits have been designed to identify strengths as well as assess relative risks within a practice which if modified may lead to improved patient outcomes and satisfaction as well as a reduction in medico legal problems for the Fellow concerned. Purpose of the Visitor Your role as a visitor is to review colleagues and to thoroughly assess their practice with the aid of the College assessment tools. This will entail providing feedback on systems, and both team and individual performance. This feedback will aid the systems and clinical care they provide. Quality Assurance You are aware that the Practice Visit process will be a “protected quality assurance activity” under the provision so of Part 3 of The Health Practitioners Competence Assurance Act 2003. As a consequence all information collected remains the property of our College and those engaging in this quality assurance activity are immune from civil liability. Confidentiality You will agree to keep the discussions and notes that you make during the practice visit confidential. This means that you will not discuss cases or the conduct of colleagues outside the practice visit process or outside any reports that you submit to the Practice Visit and Risk Management Sub-committee of the New Zealand Committee. Your Conduct You agree to act in accordance with the guidelines for the Practice Visit process (refer Guidelines for Visitors), and at all times act in a professional manner with colleagues. This means assessing the situation in a fair and open manner while respecting your colleagues who are being reviewed. You will report your findings and provide feedback with integrity and responsibility. Dispute Resolution Where there is any dispute arising out of your activities the Practice Visit sub-committee will take responsibility for addressing this. Name ....................................................................................................... Signed ....................................................................................................... Date ....................................................................................................... 17 © Copyright RANZCOG Visitor Assessment Survey Dr xx Patient Consultation Session Assessment: Consultation with new patient (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) Personability Please circle relevant number 1.1 Greeting 0 1 2 3 4 5 1.2 Allows "patient story" 0 1 2 3 4 5 1.3 Makes early and repeated eye contact 0 1 2 3 4 5 1.4 Body language 0 1 2 3 4 5 1.5 Minimises interruptions 0 1 2 3 4 5 1.6 Indicates understanding (eg short summarising statement) 0 1 2 3 4 5 1.7 Asks clarifying questions 0 1 2 3 4 5 1.8 Demonstrates empathy 0 1 2 3 4 5 1.9 Provides information to "prudent patient" standard 1.10 Asks what additional information required 0 1 2 3 4 5 0 1 2 3 4 5 1.11 Encourages questions 0 1 2 3 4 5 1.12 Allows care planning options 0 1 2 3 4 5 1.13 Provides "negotiated" care plan 0 1 2 3 4 5 1.14 Tests understanding 0 1 2 3 4 5 Listening and understanding Options, information and plan Comments: 18 © Copyright RANZCOG Practice Facilities Assessment: Reception, waiting and general areas are appropriate for patients 8.1 Waiting area has adequate space and reasonable seating 8.2 Waiting area has adequate heating, lighting and ventilation 8.3 Access and seating for disabled and wheelchair use meet legal requirement 8.4 Reading material and patient information available 8.5 Reception area sufficiently independent of waiting area to ensure verbal 8.6 Reception area ensures confidentiality of written privacy information 8.7 Appropriate indication of reception, fire exits and toilets 8.8 A separate patient toilet is available Public Private Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Comments: 9.1 9.2 9.3 9.4 9.5 9.6 9.7 Patient consultation & management areas ensure Consultation roomscomfort, adequately patient safety and privacy sized/lit/heated/ventilated Hand-washing facilities innoise each consultation room, no excessive extraneous available to patient also Patients assured of adequately privacy (physical, visual, auditory) during consultation "Chaperone" policy exists which is compatible with MCNZ guidelines Adequate examination couch and facilities for each exam room Reception area ensures confidentiality of written privacy information Adequate task lighting for examination and procedures 9.8 Disposable equipment used only once Public Private Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Comments: 19 © Copyright RANZCOG Availability & management of instruments patient comfort, safety and privacy 10.1 Medical equipment is well maintained and appropriate for clinical needs 10.2 Correct usage and monitoring of steam steriliser or autoclave for reusable instruments 10.3 Appropriate storing of sterilised instruments/materials 10.4 Appropriate use and placement of bio-hazard labelled puncture resistant sharps containers 10.5 Appropriate (leak-proof) collection, storage and collection of bio-contaminated waste 10.6 Secure/Safe storage of drugs privacy 10.7 Instruments/fluids/chemicals safely contained (e.g. from young children in consulting room) Public Private Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Yes No Comments: Practice Systems and Information Management : Result tracking and recall Public 11.1 The practice has an efficient recall system (e.g. for cervical smear recall) 11.2 Tracking test results is robust (e.g. if smear result not received, would system identify this?) 11.3 Patient Records - based on an audit of 10 medical records, 90% demonstrate 1.1 Full demographic data: Name, NHI, Address, DOB, Ethnicity, Contact phone, Occupation, Date 1.2 Records Readily interpretable by 3rd party (legible) Yes Private No Yes No (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) 0 1 2 3 4 5 0 1 2 3 4 5 Public Private Yes No Yes No Yes No Yes No (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) 1.3 History documentation 1.4 Examination findings documentation 1.5 Diagnosis (differential or actual) documentation 1.6 Demonstration of clinical reasoning 1.7 Informed consent process documentation 1.8 Letters referring to GPs enhance collaborative care and demonstrate management plan (audit of 3 letters to GPs) 1.9 Copies of letters provide to patients (0-never/1=sometimes/2=when indicated/3=usually/4=always) 20 0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 5 0 1 2 3 4 0 1 2 3 4 0 1 2 3 4 0 1 2 3 4 0 1 2 3 4 0 1 2 3 4 © Copyright RANZCOG Comments: Interviews with Colleagues and Staff (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) Professional inter-relationships Theatre coordinator (Public/Private) 13.1 Maintains a positive persona in Theatre 0 1 2 3 4 5 13.2 Relations with Nursing staff are constructive and pleasant 0 1 2 3 4 5 13.3 Relates well to other O&G staff and surgical colleagues 0 1 2 3 4 5 13.4 Is available for discussion/receptive 0 1 2 3 4 5 13.5 Collaborative (cooperative), not command (hierarchical) with stress 0 1 2 3 4 5 Anaesthetist (Public/Private) 13.6 Maintains a positive persona in Theatre 0 1 2 3 4 5 13.7 Relates well with anaesthetic and O&G surgical colleagues 0 1 2 3 4 5 13.8 Is available for discussion/receptive 0 1 2 3 4 5 13.9 Collaborative (cooperative), not command (hierarchical) in challenging clinical situations 0 1 2 3 4 5 Gynae Ward Charge Nurse (Public/Private) 13.10 Maintains a positive persona in Ward 0 1 2 3 4 5 13.11 Relations with Nursing staff are constructive and pleasant 0 1 2 3 4 5 13.12 Relates well to other O&G colleagues 0 1 2 3 4 5 13.13 Is available for discussion/receptive 0 1 2 3 4 5 13.14 Collaborative (cooperative), not command (hierarchical) with stress 0 1 2 3 4 5 13.15 0 1 2 3 4 5 Maintains caring relationships with patients Gynae Outpatient Clinic Staff Nurse 13.16 Maintains a positive persona in Clinic 0 1 2 3 4 5 13.17 Relations with Nursing staff are constructive and pleasant 0 1 2 3 4 5 13.18 Relates well to other O&G colleagues 0 1 2 3 4 5 13.19 Is available for discussion/receptive 0 1 2 3 4 5 21 © Copyright RANZCOG 13.20 Is committed to clinics 0 1 2 3 4 5 13.21 Is usually punctual 0 1 2 3 4 5 13.22 Maintains caring relationships with patients 0 1 2 3 4 5 Delivery Suite Supervisor 13.23 Maintains a positive persona in delivery suite 0 1 2 3 4 5 13.24 Relations with midwifery staff are constructive and pleasant 0 1 2 3 4 5 13.25 Relates well to other O&G colleagues 0 1 2 3 4 5 13.26 Attends for handover of patients 0 1 2 3 4 5 13.27 Is available when needed; attendance is timely 0 1 2 3 4 5 13.28 Manages urgent difficult cases collaboratively and with leadership 0 1 2 3 4 5 13.29 0 1 2 3 4 5 Maintains caring relationships with patients Clinical Director/Leader 13.30 Team skills 0 1 2 3 4 5 13.31 Flexibility/negotiability 0 1 2 3 4 5 13.32 Relates well with senior colleagues 0 1 2 3 4 5 13.33 Relates well with junior colleagues 0 1 2 3 4 5 Paediatrician 13.34 Relates well to Paediatric colleagues 0 1 2 3 4 5 13.35 Approachable/receptive/collaborative 0 1 2 3 4 5 13.36 Visits neonatal unit when has patients 0 1 2 3 4 5 Junior Medical Staff 13.37 Maintains a positive persona with junior doctors 0 1 2 3 4 5 13.38 Relates well to colleagues 0 1 2 3 4 5 13.39 Is easy to relate to; approachable 0 1 2 3 4 5 13.40 Maintains a caring relationship with patients 0 1 2 3 4 5 Comments: 22 © Copyright RANZCOG (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) Indicator 14: Systems and Risks Theatre coordinator 14.1 Maintains a positive persona in Theatre 0 1 2 3 4 5 14.2 Is readily contactable 0 1 2 3 4 5 14.3 Procedures/indications appropriately and clearly annotated on lists 0 1 2 3 4 5 14.4 Is usually punctual 0 1 2 3 4 5 14.5 Operating time-taken is usually appropriate/reasonable 0 1 2 3 4 5 14.6 Does not frequently run over allocated list time 0 1 2 3 4 5 14.7 Lists regular; balanced case mix 0 1 2 3 4 5 14.8 Complications are not excessive and are appropriately dealt with 0 1 2 3 4 5 14.9 Returns to theatre are neither too frequent nor problematic 0 1 2 3 4 5 Anaesthetist 14.10 Meets requirements for notification of lists/patients 0 1 2 3 4 5 14.11 Appropriate work-up and consultation of high-risk patients 0 1 2 3 4 5 14.12 Procedures appropriately and clearly annotated on lists 0 1 2 3 4 5 14.13 Is readily contactable 0 1 2 3 4 5 14.14 Operating time-taken is usually appropriate/reasonable 0 1 2 3 4 5 14.15 Does not frequently run over allocated list time 0 1 2 3 4 5 14.16 Lists regular; balanced case mix 0 1 2 3 4 5 14.17 Complications are not excessive and are appropriately dealt with 0 1 2 3 4 5 14.18 Returns to theatre are neither too frequent nor problematic 0 1 2 3 4 5 Gynae Charge Nurse 14.19 Appropriate post-operative care (i.e. frequency of visits, care plans communicated 0 1 2 3 4 5 14.20 Is readily contactable 0 1 2 3 4 5 14.21 Ensures and notifies cover arrangements when needed 0 1 2 3 4 5 14.22 Reacts appropriately and in timely fashion when complications occur 0 1 2 3 4 5 14.23 Complications are not excessive and are appropriately dealt with 0 1 2 3 4 5 14.24 Workload 0 1 2 3 4 5 Gynae Outpatient Clinic Staff Nurse 14.25 Case mix of patients seen meets clinic's needs 0 1 2 3 4 5 14.26 Manages difficult patients well 0 1 2 3 4 5 23 © Copyright RANZCOG 14.27 0 1 2 3 4 5 General performance Delivery Suite Supervisor 14.28 Subjectively appears competent 0 1 2 3 4 5 14.29 Is perceived to have at least average technical expertise 0 1 2 3 4 5 14.30 Informal teaching skills 0 1 2 3 4 5 14.31 Is less busy than average, average, or above average workload 0 1 2 3 4 5 14.32 Appears able to handle sleep deprivation reasonably 0 1 2 3 4 5 Clinical Director/Leader 14.33 Conducts ward-rounds when indicated 0 1 2 3 4 5 14.34 Maintains equitable workload 0 1 2 3 4 5 14.35 Attends peer groups (audit/teaching) 0 1 2 3 4 5 14.36 General performance 0 1 2 3 4 5 14.37 Manages difficult patients well 0 1 2 3 4 5 14.38 Case mix meets unit/team needs 0 1 2 3 4 5 Paediatrician 14.39 Consults paediatric services on high risk pre-partum patients 0 1 2 3 4 5 14.40 Timely involvement of paediatric services in high-risk births 0 1 2 3 4 5 14.41 Neonatal complications compare with usual range 0 1 2 3 4 5 Junior Medical Staff 14.42 Is available when needed 0 1 2 3 4 5 14.43 Has a role model or apprenticeship approach 0 1 2 3 4 5 14.44 Provides sufficient clinical supervision, support and backup 0 1 2 3 4 5 14.45 Does necessary ward-rounds (e.g. post-acute) 0 1 2 3 4 5 14.46 Provides sufficient teaching 0 1 2 3 4 5 14.47 Manages difficult cases well 0 1 2 3 4 5 14.48 Manages complications well 0 1 2 3 4 5 Comments: 24 © Copyright RANZCOG Theatre Observations (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) Risk Management Relationships 16.1 Maintains a positive/approachable persona in theatre 0 1 2 3 4 5 16.2 Relations with Nursing staff are constructive and pleasant 0 1 2 3 4 5 16.3 Relates well with anaesthetic and other med/surgical colleagues 0 1 2 3 4 5 Systems 16.4 Structural arrangements 0 1 2 3 4 5 16.5 Lists per week/Case mix 0 1 2 3 4 5 16.6 Staff role organisation and utilisation 0 1 2 3 4 5 16.7 Reads patient records prior to surgery 0 1 2 3 4 5 16.8 Checks procedure with patient & list before proceeding 0 1 2 3 4 5 16.9 Consent form adequate and checks in theatre 0 1 2 3 4 5 16.10 Relevant test results available/referred to in theatre 0 1 2 3 4 5 16.11 Indications for surgery within professional guidelines 0 1 2 3 4 5 Documentation/audit 16.12 Operation notes/records 0 1 2 3 4 5 16.13 Audits 0 1 2 3 4 5 16.14 1st 24 Hours of post-op plan recorded 0 1 2 3 4 5 (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) Technical aspects 17.1 Conventional methodology observed 0 1 2 3 4 5 17.2 Sound operative techniques 0 1 2 3 4 5 17.3 Utilises assistant well 0 1 2 3 4 5 17.4 Appropriate use of instruments 0 1 2 3 4 5 17.5 Aseptic technique 0 1 2 3 4 5 17.6 Stance and posture 0 1 2 3 4 5 17.7 Management of stress/unpredicted events/presence of visitor 0 1 2 3 4 5 17.8 Use of antibiotic or anticoagulant prophylaxis 0 1 2 3 4 5 17.9 Discussion with anaesthetist as to post-op meds 0 1 2 3 4 5 25 © Copyright RANZCOG (0=unsatisfactory; 1=poor; 2=Satisfactory.; 3=good; 4=v.good; 5=Excellent) Post-operative care plan 18.1 Proposed frequency of visits 0 1 2 3 4 5 18.2 Availability in emergencies 0 1 2 3 4 5 18.3 Proposed rate of discharge 0 1 2 3 4 5 18.4 Recommended return to work 0 1 2 3 4 5 18.5 Recommended time for post-op visit 0 1 2 3 4 5 18.6 Relative notified 0 1 2 3 4 5 Comments: 26 © Copyright RANZCOG