May Case Study - Charles Poole
advertisement

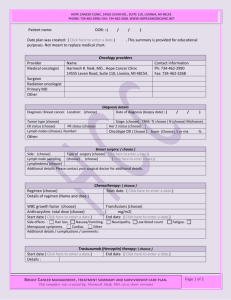
1 Charles Poole May Case Study May 31, 2012 Intensity Modulated Radiotherapy of Ductal Carcinoma in Situ (DCIS) of the Left Breast History of Present Illness: Patient JK is a 66 year old female who underwent a routine mammogram screening in mid-September 2009. The mammogram screening revealed a cluster of calcifications in the upper outer quadrant of the left breast. Subsequently, a stereotactic needle biopsy revealed a high grade, non-invasive, ductal carcinoma in situ (DCIS) that was estrogen receptor (ER) and progesterone receptor (PR) positive. For patients with positive receptors for the hormones estrogen and progesterone, approximately two out of three breast cancer growths may be facilitated by estrogen.1 Several anti-estrogen approaches to block the effects of estrogen such as Tamoxifen are being used to treat hormone receptor-positive breast cancers.1 Patients with receptor-positive tumors are more likely to respond to hormonal therapies and have better outcomes than receptor negative patients.2 In late September 2009, JK underwent a wirelocalized tumor lumpectomy of the left breast with the greatest dimension reported as 1.3 cm which demonstrated no invasive disease. The surgical margins were negative with the closest margin reported at 0.5 cm. No sentinel lymph node or axillary lymph nodes were reported. Postoperatively, the lumpectomy specimen confirmed the initial biopsy findings and JK was diagnosed with high grade, non-invasive DCIS involving the left breast which was ER and PR positive. Upon further evaluation from a multi-disciplinary tumor board, it was recommended to JK that radiation therapy be considered as the primary treatment for her diagnosis. The medical oncologist also discussed with JK the use of Tamoxifen due to the patients ER and PR positivity. The patient weighed the risks and benefits of this drug and ultimately decided against incorporating Tamoxifen into her treatment regimen. In mid-October 2009, the patient was referred to radiation oncology for consultation of post-operative irradiation to the left breast. The radiation oncologist discussed various treatment regimens with JK, such as partial breast irradiation and whole breast irradiation. The radiation oncologist recommended radiation treatment to the entire left breast with an additional radiation boost treatment to the tumor bed as the standard of care for this early diagnosis. The treatment 2 benefits and side effect complications were discussed and JK elected to proceed with radiation treatment. Past Medical History: JK has a past medical history of hypertension, migraine headaches, and urinary incontinence. The patient’s surgical history includes bi-lateral carpal tunnel surgery, cholecystectomy, an endoscopic retrograde cholangiopancreatography (ERCP) for retained gallstones following cholecystectomy, and an appendectomy. In addition, the patient reported undergoing open heart surgery for repair of an atrial septal defect. The patient also reported that at age 32 she underwent a total abdominal hysterectomy with bi-lateral salpino-oophorectomy and began using estrogen vaginal cream recommended by her physician at the time. JK states no allergies or reactions to medications, food, or latex. Social History: JK is a retired nurse from a regional medical center in the Midwest and lives in a small rural farming community. JK is married and a lifetime non-smoker and has never used tobacco. JK states she does not drink alcohol and denies any drug use. In addition, the patient reported a prevalent history of cancer in her extended family and stated her brother was diagnosed with metastatic breast cancer around 40 years of age. In addition, JK had one daughter that was diagnosed with an astrocytoma at age 21. Medications: JK uses the following medications: Colace, Citrucel, omeprazole, atenolol, Hyzaar, amitriptyline at night, amlodipine, Enablex, meclizine, folic acid, docusate sodium, multi-vitamin, calcium, vitamin D, and fish oil. Diagnostic Imaging: In September of 2009, JK underwent a routine mammogram screening which revealed a cluster of calcifications in the upper outer quadrant of the left breast. A stereotactic needle biopsy was performed in the suspected calcified region of tissue within the left breast. Pathology from this biopsy concluded the suspicious calcified tissue was a high grade, non-invasive, DCIS that was ER and PR positive. A lumpectomy was performed with the greatest dimension of the tumor reported as 1.3 cm with no positive margins reported. The sentinel and axillary lymph nodes were not reported or dissected. Pathology from the lumpectomy tissue in the left breast confirmed a diagnosis of DCIS. Recommendations: The radiation oncologist reviewed the patient’s surgical history and pathology reports and recommended JK undergo postoperative radiation therapy to the left breast using an intensity modulated radiation therapy (IMRT) plan. This would be followed by a boost 3 plan utilizing an enface electron beam targeting the tumor bed site within the left breast. The recommendation to use IMRT for the initial plan was to achieve a homogeneous dose distribution throughout the left breast volume while sparing normal structures such as the heart and left lung that are located in proximity to the left breast volume. IMRT may lessen the radiation toxicity effects to portions of the underlying lung and heart volumes by offering more degrees of freedom in the planning process.3 Dose homogeneity with conventional threedimensional conformal radiotherapy (3DCRT) may be worse in patients with large breast volumes and hotspots may increase within the target and surrounding normal tissues.3 IMRT offers the ability of improved dose homogeneity and decreased normal tissue irradiation.3 The Plan (prescription): The radiation oncologist’s recommendation for JK was to utilize IMRT for the left breast primary treatment. In addition, a boost region involving the tumor bed region within the left breast was recommended by the radiation oncologist to be treated after the left breast region was treated. The boost plan would utilize an enface electron beam targeting the tumor bed. The prescription dose for the initial left breast IMRT plan was 46.8Gy at 1.8Gy per fraction for 26 fractions. The dose for the left breast IMRT plan was prescribed to a left breast volume that the radiation oncologist contoured as a target volume. The boost prescription dose to the tumor bed region was 12.6Gy at 1.8Gy per fraction for seven fractions. The composite dose to the left breast tumor bed region was 61.2Gy. For the evaluation of this case study, only the primary left breast IMRT treatment technique will be discussed. Patient Setup / Immobilization: JK underwent a computed tomography (CT) simulation scan for radiation therapy treatment in October 2009. The patient was placed on the CT simulation couch in the supine position with her left arm raised and positioned above her head on a MedTec, Inc. breast board immobilization device (Figure 1). The breast board was inclined 15° and the patient’s head was turned to the right and supported with a breast board headrest (Figure 2). The patient had a sponge under her knees for support and her right arm was at her side for comfort. The radiation oncologist identified the superior, inferior, medial, and lateral regions of the left breast tissue on the skin surface with BB’s. Also, the lumpectomy scar was outlined on the patient’s skin surface by the physician with CT wire to identify the location of the scar on the CT simulation scan. 4 Anatomical Contouring: Once the CT simulation scan was complete, the CT dataset was transferred into the Philips Pinnacle3 8.0m radiation treatment planning system (TPS). The left breast volume was contoured on the TPS by the radiation oncologist and included the superior portion of breast tissue extending through to the inferior portion of breast tissue. The tumor bed was also contoured by the physician. The identification of the tumor bed proved challenging for the radiation oncologist. Postsurgical seroma changes within the breast tissue are difficult at times to identify. The radiation oncologist verified the location and size of the tumor bed from previous operative reports, the seroma from the lumpectomy procedure, and the location of the scar that was wired at the time of simulation. In addition, the left breast volume was adjusted 0.4 cm inside from the skin surface to avoid excessive dose to the patient’s left breast skin surface. The medical dosimetrist contoured organs at risk (OR) which included the left and right lungs, a total lung volume, the heart, carina, and normal tissue. The radiation oncologist reviewed the OR and final adjustments were made to proceed with radiation treatment planning. The medical dosimetrist was given a prescription objective sheet to begin treatment planning. Beam Isocenter / Arrangement: An isocenter was placed by the medical dosimetrist in the left chest wall adjacent to the left lung. The placement of the isocenter corresponded approximately to the mid-plane depth of the medial and lateral tangential beams and the center of the superior and inferior extents of the left breast volume (Figure 3). The left breast IMRT plan utilized four coplanar tangential photon fields arranged at gantry angles of 313°, 338°, 113°, and 138° (Figures 4-6). Each of the four fields utilized a 6 MV beam energy due to the location of the left breast volume in relation to the skin surface. There was no collimator or couch rotation associated with any of the four IMRT fields. The medical dosimetrist assigned the prescription to the four fields and entered the left breast IMRT objectives in the IMRT module of the TPS. The TPS determined and automatically adjusted the field sizes of each beam in relation to the treatment objectives in order to accomplish the desired dose distribution around the target volume (Figure 7). Treatment Planning: The radiation oncologist outlined dose objectives to the left breast target volume and OR dose constraints for this plan. The objectives of the IMRT plan were to reduce the radiation toxicity to the heart and left lung while maintaining a homogeneous dose distribution throughout the left breast and limiting radiation dose to the OR (Figures 8-14). For the left breast volume, a uniform, minimum, and maximum dose objective corresponding with 5 the prescribed dose were entered into the IMRT module of the TPS. In addition, the OR dose constraints were entered into the IMRT module of the TPS for plan optimization. The OR constraints of the plan included: the heart maximum dose was to be less than 50Gy and the volume at 30Gy (V30) was to be less than 10%, the left lung volume at 20Gy (V20) was to be less than 17% or as low as possible. A normal tissue objective was used to control peripheral dose outside of the left breast target volume. The TPS utilized the direct machine parameter optimization (DMPO) feature with 50 segments to accomplish the IMRT objectives and parameters. Once adequate prescription dose coverage was achieved to the left breast volume, the medical dosimetrist reviewed the OR doses, the isodose lines, and the dose volume histogram (DVH) (Figure 15). The radiation oncologist also reviewed this plan and assigned a normalization of 97% for the treatment plan. The monitor units were reviewed and a second check was completed with a quality assurance (QA) computer program. The monitor units were within tolerance for this IMRT plan. Conclusion: This plan presented the medical dosimetrist with some challenges utilizing IMRT for left breast treatment. One challenge was maintaining a daily reproducible setup of the patient. In the patient setup, the left arm was raised above the head and the patient was on an inclined breast board. This proved very challenging for the radiation therapists and the medical dosimetrist to reproduce this setup consistently day to day. With IMRT, treatment plans are very conformal and a homogeneous dose distribution can be achieved throughout the target volume. However, if the patient position is slightly off-set everyday due to setup variations a geometric miss may occur in target area. Other challenges this plan presented were related to target volume movement from patient respiration and possible swelling of breast tissue during treatment. The field aperture for each IMRT beam was opened 3.0 cm in order to account for breathing motion, swelling, and setup variation. This margin adequately accounts for all these variables without compromising the treatment plan. With some minor adjustments, the IMRT technique for the treatment of breast cancer yields a plan whose dosimetric conformity and reduction of hot spots is exceptional without compromising the practicality of a clinically reproducible setup. 6 Figure 1: Patient position on a Med-Tec, Inc. breast board at CT simulation. 7 Figure 2: Patient position from CT simulation. Figure 3: Isocenter placement. 8 Figure 4: Isocenter placement in the axial view. 9 Figure 5: Isocenter placement in the sagittal view. 10 Figure 6: Isocenter placement in the coronal view. 11 Figure 7: Field sizes determined automatically by the TPS. 12 Figure 8: IMRT dose distribution of the left breast. 13 Figure 9: IMRT dose distribution of the left breast. 14 Figure 10: IMRT dose distribution of the left breast. 15 Figure 11: IMRT dose distribution of the left breast. 16 Figure 12: IMRT dose distribution of the left breast. 17 Figure 13: IMRT dose distribution of the left breast. 18 Figure 14: IMRT dose distribution of the left breast. 19 Figure 15: Dose Volume Histogram (DVH). 20 References 1. Breast cancer hormone therapy. American Cancer Society. http://www.cancer.org/Cancer/BreastCancer/DetailedGuide/breast-cancer-treating-hormonetherapy. 2012. 2. Uschold GM, Zhang H. Breast Cancer. In: Washington CM, Leaver D, eds. Principles and Practice of Radiation Therapy. 3rd ed. St. Louis, MO: Mosby-Elsevier; 2010: 866-894. 3. Schubert L, Gondi V, Cannon G, et al. Dosimetric comparison of left-sided whole breast irradiation with 3DCRT, forward-planned IMRT, inverse-planned IMRT, helical tomotherapy, and topotherapy. Radiother Oncol. 2011;100(2):241-246.