Scalp, Face, & Parotid Region
advertisement
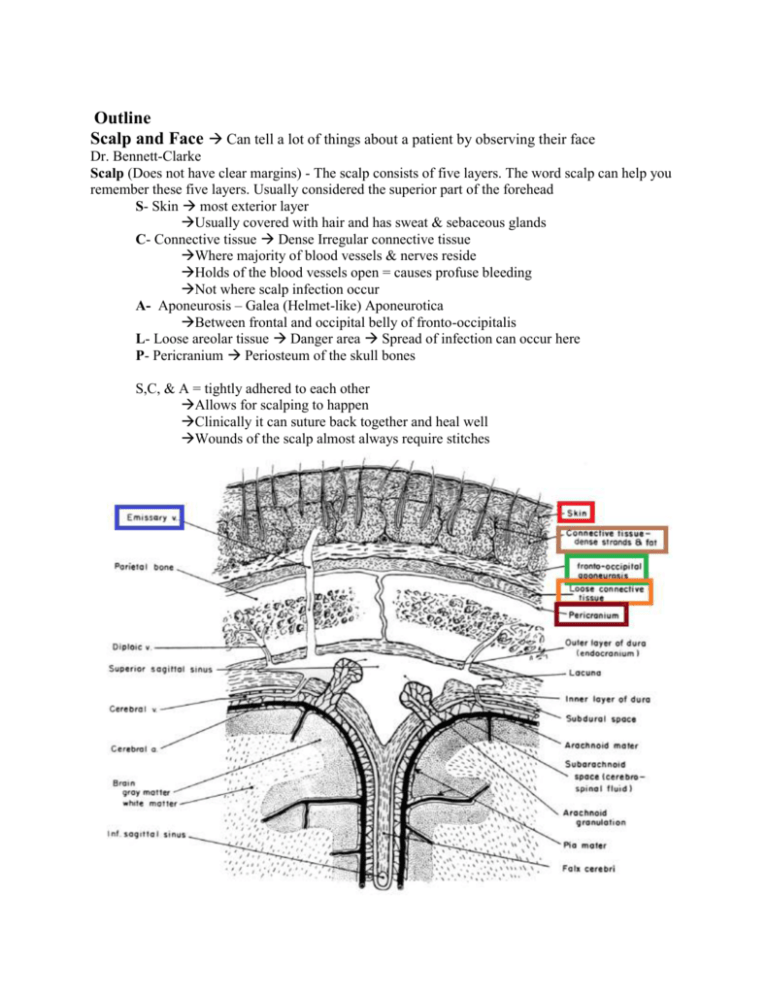
Outline Scalp and Face Can tell a lot of things about a patient by observing their face Dr. Bennett-Clarke Scalp (Does not have clear margins) - The scalp consists of five layers. The word scalp can help you remember these five layers. Usually considered the superior part of the forehead S- Skin most exterior layer Usually covered with hair and has sweat & sebaceous glands C- Connective tissue Dense Irregular connective tissue Where majority of blood vessels & nerves reside Holds of the blood vessels open = causes profuse bleeding Not where scalp infection occur A- Aponeurosis – Galea (Helmet-like) Aponeurotica Between frontal and occipital belly of fronto-occipitalis L- Loose areolar tissue Danger area Spread of infection can occur here P- Pericranium Periosteum of the skull bones S,C, & A = tightly adhered to each other Allows for scalping to happen Clinically it can suture back together and heal well Wounds of the scalp almost always require stitches 1. Innervation to the scalp Cranial nerves 1. Supratrochlear nerve (CN V1) 2. Supraorbital nerve (CN V1) = supplies scalp at vertex & slightly beyond 3. Zygomaticotemporal Nerve (CN V2) 4. Auriculotemporal Nerve (CN V3) Ventral primary ramus 1. Lesser Occipital Nerve (C2) – from cervical plexus Dorsal primary ramus 1. Greater Occipital Nerve (C2) 2. Third Occipital Nerve (C3) 2. Blood supply to the scalp Internal carotid 1. Supratrochlear & Supraorbital Artery From ophthalmic artery External carotid 1. Posterior Auricular Artery 2. Superficial Temporal Artery 3. Occipital Artery Venous Drainage = follows named arteries but drains in to External & Internal Jugulars Emissary Veins = run from scalp, through bone, & into dural sinuses (Not Primary Pathway) Conduit from scalp to meninges and vice versa = can aid spread of infection Face- The skin of the face contains numerous sweat and sebaceous glands. It is connect to the underlying bones by loose connective tissue. There is no deep fascia present in the face. 1. Bones of the face- These are the bones seen on the anterior view of the skull. A. Nasal Bones (2) B. Maxilla (2) C. Mandible (1) D. Zygomatic Bones (2) E. Lacrimal Bones (2 of them in orbit) F. Vomer (1 & part of nasal septum) G. Palatine (2) H. inferior Nasal Conchae (2) I. Ethmoid (1 & in nasal cavity & part of nasal septum) ** Make sure you review the bones of the face. Skin of the face Very vascular = heals well Very flexible/pliable – Diminishes with age Tightly fixed at chin & bridge of nose – everywhere else it can sag/droop No deep fascia on the face = nothing to limit/contain injury/infection to compartments No fascia connected to underlying bones Highly innervated 1. Sensory innervation of the skin of the face-The three braches of the trigeminal nerve provide the majority of the sensory innervation to the skin of the face. 1. Ophthalmic nerve 1. Supraorbital Nerve = uses Supraorbital foramen 2. Supratrochlear Nerve 3. Lacrimal nerve 4. Infratrochlear Nerve 5. External Nasal nerve 2. Maxillary nerve 1. Infraorbital Nerve = uses Infraorbital foramen 2. Zygomaticofacial nerve 3. Zygomaticotemporal Nerve 3. Mandibular nerve 1. Mental nerve = uses Mental foramen 2. Buccal nerve 3. Auriculotemporal Nerve 2. Blood supply to the face- The main artery to the face is the facial artery, a branch of the external carotid artery. There are other smaller arteries which also help to provide blood to the face. 1. Facial artery A. Submandibular Artery B. Inferior Labial Artery C. Superior Labial Artery D. Angular Artery (Medial corner of eye) 2. Superficial temporal artery 3. Transverse facial artery (Runs with Parotid Duct) 4. Supraorbital 5. Supratrochlear arteries 6. Angular Vein 7. Facial Vein (Not torturous like the artery & Gets its tributaries) 1. At medial corner of eye it is continuous with Inferior Ophthalmic Vein Continuous with Cavernous Sinus (Dural Sinus) 2. Drains into Deep Facial vein to Pterygoid Plexus Continuous with Cavernous Sinus ***No valves in this area & is an abnormal pathway for venous drainage Muscles of the face- The Muscles of facial expression are embedded in the superficial fascia of the face insert on the skin. They are all innervated by the facial nerve (CN VII). Refer to the attached diagram for the specific location of several of these muscles. ***Origin & Insertion = not important BUT Actions = IMPORTANT Most Origen = Subcutaneous fascia & Some = Facial Bones Attached to skin of face ( Act as Dilators of Sphincters All innervated by CN VII All developed from pharyngeal arch II 1. Frontal belly of Fronto-occipital muscle 3. Orbicularis Oculi close eye tightly 10. Orbicularis Oris Close Lips – Fish Lips 13. Depressor Anguli Oris Depresses corner of mouth 14. Depressor Labii InferiorisDepress Lower lip = shower lower teeth 7. Zygomaticus major Draw up corners of mouth = smile 11. Levator Labii Superioris Elevate upper lip = show upper teeth 12. Levator Anguli Oris Help draw up corner of mouth = show upper teeth & smile 9. Levator Labii Superioris Alaque Nasi Works with upper lip to flair the nostrals Platysma Tighten skin of neck Some depression of jaw Innervation = cervical branch of facial nerve Fronto-occiptal Muscle Frontal & Occipital Bellies Raise Eyebrows = Frontal bellies Facial nerve (CN VII)- This nerve supplies all of the muscles of facial expression but does not supply the skin overlying them. The facial nerve exits the skull via the stylomastoid foramen to supply the muscles of facial expression. Innervation for Muscles of Facial Expression (Skeletal Muscles) = CN VII = Facial Nerve Multipolar motor neurons = originate in brainstem It courses through the substance of the parotid gland to be distributed in 5 main branches on the face. Temporal branch Two Zygomatic Branch Zebras Buccal Branch Bit Marginal Branch My Cervical branch Cookie Any trauma, inflammation, damage of the facial nerve results in loss of function to the muscles of facial expression (Bell’s palsy). Loss of facial competence, drooling, etc Patient CANNOT close eye (get dry eyes and can get corneal ulceration from chronic dryness) Usually not permanent Usually from inflammation of the nerve (more frequently from middle ear infection) Frequent with Lyme’s disease 7 higher incidences with pregnancy Most likely treatment = steroids The Parotid Gland/ Parotid Bed - These are the largest salivary glands in the body. The parotid duct passes over the surface of the masseter muscle, pierces the buccinator muscle and opens on the mouth adjacent to the second upper molar. Structures which traverse or lie deep to the parotid gland include: 1. Facial nerve (CN VII) & Branches 2. Superficial temporal artery 3. Retromandibular vein 4. Auriculotemporal nerve ***Anything that can impart/injure the parotid can impact these structures