STANDARD 6: COMPETENCIES, CURRICULAR OBJECTIVES
advertisement

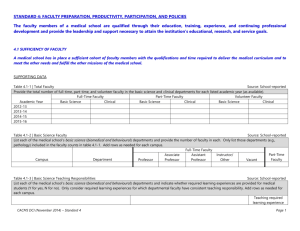
STANDARD 6: COMPETENCIES, CURRICULAR OBJECTIVES, AND CURRICULAR DESIGN The faculty of a medical school define the competencies to be achieved by its medical students through medical education program objectives and is responsible for the detailed design and implementation of the components of a medical curriculum that enables its medical students to achieve those competencies and objectives. The medical education program objectives are statements of the knowledge, skills, behaviors, and attitudes that medical students are expected to exhibit as evidence of their achievement by completion of the program. OVERVIEW DATA Table 6.0-1 | Academic Year 1 - Instructional Formats Source: School-reported Using the most recently-completed academic year, list each required learning experience from year one of the curriculum and provide the total number of instructional hours for each listed instructional format. Note that “small group” includes case-based and problem-solving sessions. Provide the total number of hours per required learning experience and instructional format. Provide a definition of “other” if selected. Add rows as needed for each campus. Number of Formal Instructional Hours per Required Learning Experience Required learning experience Lecture Lab Small Group Patient Other Total Campus Weeks Contact (Describe) TOTAL Table 6.0-2 | Academic Year 2 - Instructional Formats Source: School-reported Using the most recently-completed academic year, list each required learning experience from year two of the curriculum and provide the total number of instructional hours for each listed instructional format. Note that “small group” includes case-based or problem-solving sessions. Provide the total number of hours per required learning experience and instructional format. Provide a definition of “other” if selected. Add rows as needed for each campus. Number of Formal Instructional Hours per Required Learning Experience Lecture Lab Small Group Patient Other Total Campus Required learning experience Weeks Contact (Describe) TOTAL Table 6.0-3 | Academic Years 3 and 4 - Weeks/Formal Instructional Hours Source: School-reported Provide data from the most recently-completed academic year on the total number of weeks and formal instructional hours per week (includes lectures, conferences, teaching rounds, clinical and procedural skills teaching/workshops) for each required learning experience in years three-four of the curriculum. Provide a range of hours if there is significant variation across weeks. Note that hours devoted to patient care activities should NOT be included. Add rows as needed for each instructional site if there are differences between sites. Instructional Site Required learning experience Total Weeks Typical Hours per Week of Formal Instruction CACMS DCI (November 2014) – Standard 6 Page 1 NARRATIVE RESPONSE a. Provide a brief description of the structure of the medical curriculum including the relationships between required learning experiences and the rationale for their placement in the curriculum. b. Provide a separate, brief description of each parallel curriculum (e.g., longitudinal integrated clerkship). Include the following information in each description, and highlight the difference(s) from the curriculum of the medical education program taken by the majority of medical students. Name of parallel curriculum: 1. The placement of the parallel curriculum in the medical education program (e.g., year 3 only, all years) 2. The location of the parallel curriculum (main campus, geographically distributed campus and/or community sites) 3. The year the parallel curriculum was first offered 4. The focus of the parallel curriculum, including the additional objectives that students must achieve 5. The general structure of the parallel curriculum (including the sequence of required learning experiences in each curriculum year/phase) 6. The number of students participating in the parallel curriculum for the last three academic years by year of the medical education program in which the parallel curriculum is implemented (e.g., if the parallel curriculum is implemented only in year 3, provide the number of third-year medical students who have participated each year for the last three academic years). CACMS DCI (November 2014) – Standard 6 Page 2 SUPPORTING DOCUMENTATION a. A schematic or diagram that illustrates the structure of the curriculum. The schematic or diagram should show the approximate sequencing of, and relationships among, required learning experiences in each academic year. (Appendix DD) b. If the structure of the curriculum has changed significantly since the DCI and self-study were completed (i.e., a new curriculum or curriculum year has been implemented), include a schematic of the new curriculum, labeled with the year it was first introduced. (Appendix EE) c. A schematic of any parallel curriculum. (Appendix FF) CACMS DCI (November 2014) – Standard 6 Page 3 6.1 FORMAT / DISSEMINATION OF MEDICAL EDUCATION PROGRAM OBJECTIVES AND LEARNING OBJECTIVES The faculty of a medical school define its medical education program objectives in competency-based terms that reflect and support the continuum of medical education in Canada and allow the assessment of medical students’ progress in developing the competencies for entry into residency and expected by the profession and the public of a physician. The medical school makes these medical education program objectives known to all medical students and faculty members with leadership roles in the medical education program, and others with substantial responsibility for medical student education and assessment. In addition, the medical school ensures that the learning objectives for each required learning experience are made known to all medical students and those faculty, residents, and others with teaching and assessment responsibilities in those required experiences. SUPPORTING DATA Table 6.1-1 | Competencies, Medical Education Program Objectives, and Outcome Measures Source: School-reported List each general competency and demonstrate the relationship between each general competency expected of graduates, the medical education program objectives, and the outcome measure(s) specifically used to assess students’ attainment of each related objective and competency. Add rows as needed. General Competency Medical Education Program Objective(s) Outcome Measure(s) NARRATIVE RESPONSE a. Provide the year in which the current medical education program objectives were last reviewed and approved. b. Describe how and by whom the medical education objectives were developed, reviewed and approved to ensure that they: 1. Reflect and support the continuum of medical education in Canada 2. Link to the relevant competencies 3. Allow the assessment of medical students’ progress in developing the competencies for entry into residency and expected by the profession and the public of a physician CACMS DCI (November 2014) – Standard 6 Page 4 c. Describe how the medical school selected the outcome measures for the assessment of its medical education program objectives. How does the medical school ensure that the outcome measures selected are sufficiently specific to allow a judgment that each of the medical education program objectives has been met? d. Describe how medical education program objectives are made known to each of the following groups: e. 1. Medical students 2. Faculty members with leadership roles in the medical education program 3. Other individuals with substantial responsibility for medical student education and assessment Describe how learning objectives for each required learning experience are made known to each of the following groups: 1. Medical students 2. Faculty with responsibility for teaching, supervising or assessing medical students in a specific required learning experience 3. Residents and non-faculty instructors with responsibility for teaching, supervising or assessing medical students in a specific required learning experience CACMS DCI (November 2014) – Standard 6 Page 5 6.2 REQUIRED CLINICAL LEARNING EXPERIENCES The faculty of a medical school define the types of patients and clinical conditions that medical students are required to encounter, the skills and procedures to be performed by medical students, the appropriate clinical settings for these experiences, and the expected levels of medical student responsibility. SUPPORTING DATA Table 6.2-1 | Required Clinical Learning Experiences (Required Patient Encounters and Procedural Skills) Source: School-reported For each required clinical learning experience, list and describe each patient type, clinical condition, required procedure and skill, and clinical setting in which they take place, along with the required level(s) of student responsibility. Patient Type Clinical Condition Procedures/Skills Clinical Setting(s) Level of Student Responsibility NARRATIVE RESPONSE a. Define the levels of student responsibility provided in table 6.2-1. b. Describe how the list of required patient encounters and procedural skills was developed. c. Describe how and by which individuals and groups the list of required patient encounters and procedural skills was reviewed and approved. Note if the curriculum committee or other central oversight body played a role in reviewing and approving the list of required patient encounters and procedural skills across required learning experiences. d. Describe which individuals and/or groups developed the list of alternatives designed to remedy gaps when students are unable to access a required patient encounter or perform a required procedural skill. How was the list of alternative experiences developed? Which individuals and groups approved the list of alternative experiences? CACMS DCI (November 2014) – Standard 6 Page 6 e. Describe how medical students, faculty, and residents are informed of the required patient encounters and procedural skills in each required clinical learning experience. CACMS DCI (November 2014) – Standard 6 Page 7 6.3 SELF-DIRECTED AND LIFE-LONG LEARNING The faculty of a medical school ensure that the medical curriculum includes self-directed learning experiences and time for independent study to allow medical students to develop the skills of lifelong learning. Self-directed learning involves medical students’ self-assessment of learning needs; independent identification, analysis, and synthesis of relevant information; and appraisal of the credibility of information sources. NARRATIVE RESPONSE a. Describe the learning sessions, and the required learning experiences in which these learning sessions occur during the first two years of the curriculum, where in the context of a clinical case, students engage in all of the following components of self-directed learning as a unified sequence (use the names of relevant required learning experiences from the Overview tables 6.0-1 and 6.0-2 when answering): 1. 2. 3. 4. 5. Identify, analyze, and synthesize information relevant to their learning needs Assess the credibility of information sources Share the information with their peers and tutor/facilitator Apply their knowledge to the resolution of the clinical case Receive feedback and are assessed on their skills in self-directed learning b. Referring to the sample schedules requested below, describe for the first two years of the program, the amount of scheduled time for self-directed learning sessions. SUPPORTING DOCUMENTATION a. Schedules that illustrate the amount of time in the first and second years of the curriculum that medical students spend in self-directed learning sessions. (Appendix GG) CACMS DCI (November 2014) – Standard 6 Page 8 6.4 INPATIENT / OUTPATIENT EXPERIENCES The faculty of a medical school ensure that the medical curriculum includes clinical experiences in both outpatient and inpatient settings. SUPPORTING DATA Table 6.4-1 | Percentage Total Required Clinical Learning Experience Time Source: School-reported Provide the percentage of time that medical students spend in inpatient and ambulatory settings in each required clinical learning experience. If the names differ from those in the table, substitute the name used by the medical school. If the amount of time spent in each setting varies across instructional sites (e.g., hospitals), provide a range. Add rows as needed for each campus. % of Total Required Clinical Learning Experience Time Campus Ambulatory Inpatient Emergency Medicine Family medicine Internal medicine Obstetrics Gynecology Pediatrics Psychiatry Surgery Other (list) Source: AAMC CGQ and AFMC GQ Table 6.4-2 | Inpatient and ambulatory patient experience Provide data from the AAMC Canadian Graduation Questionnaire (CGQ) and the AFMC Graduation Questionnaire (AFMC GQ) on the percentage of respondents that agree/strongly agree (aggregated) that when they are presented with a variety of patients that they have the knowledge and skills to perform the tasks listed in the table. Add rows as needed for each campus. School % Campus 2013 2014 2015 Care for patients in a hospital setting Care for patients in an ambulatory setting NARRATIVE RESPONSE a. Describe how the curriculum committee or subcommittee ensures that medical students spend sufficient time in ambulatory and inpatient settings to meet the learning objectives for each required clinical learning experience. CACMS DCI (November 2014) – Standard 6 Page 9 6.5 ELECTIVE OPPORTUNITIES The faculty of a medical school ensure that the medical curriculum includes elective opportunities that supplement required learning experiences and that permit medical students to gain exposure to and deepen their understanding of medical specialties reflecting their career interests and to pursue their individual academic interests. SUPPORTING DATA Table 6.5-1 | Required Elective Weeks Provide the number of required weeks of elective time in each year of the curriculum. Total Required Elective Weeks Year 1 Year 2 Source: School-reported Year 3 Year 4 NARRATIVE RESPONSE a. Indicate whether the medical school has a policy (e.g., the AFMC UGME/PGME Policy on Diversification of Electives), that requires diversification of electives. How and by whom is students’ adherence to this policy monitored? b. Describe the policies or practices that require or encourage medical students to use electives to pursue a broad range of interests in addition to their chosen specialty. SUPPORTING DOCUMENTATION a. Policy on the diversification of electives. (Appendix HH) CACMS DCI (November 2014) – Standard 6 Page 10 6.6 SERVICE-LEARNING The faculty of a medical school ensure that the medical education program provides sufficient opportunities for, encourages, and supports medical student participation in service-learning and community service activities. SUPPORTING DATA Table 6.6-1 | Service learning Source: ISA Provide data from the independent student analysis (ISA), by curriculum year, on the percentage of respondents that were satisfied/very satisfied (aggregated) with their access to opportunities to participate in service learning experience. If available, provide medical school administrative data in an additional table. School % Campus Year 1 Year 2 Year 3 Year 4 NARRATIVE RESPONSE a. Summarize the opportunities for medical students to participate in required and voluntary service-learning and community service activities, including the general types of activities that are available. b. Describe how medical student participation in service-learning and community service activities is encouraged. How are students informed about the availability of these activities? c. Describe how the medical school supports service-learning and community service activities. CACMS DCI (November 2014) – Standard 6 Page 11 6.7 ACADEMIC ENVIRONMENTS The faculty of a medical school ensure that medical students have opportunities to learn in academic environments that permit interaction with students enrolled in other health professions, graduate, and professional degree programs, and opportunities to interact with residents in clinical environments and with physicians in continuing medical education activities. SUPPORTING DATA Table 6.7-1 | Health Professions Degree Programs Taught by Medical School Faculty Source: School-reported List the health professions degree programs taught by the medical school faculty where medical students have the opportunity to interact with these programs’ students in academic environments. Add rows as needed for each campus. Campus Health Professions Program Table 6.7-2 | Master’s and Doctoral Degree Programs Taught by Medical School Faculty Source: School-reported List the biomedical or biological sciences master’s and doctoral degree programs taught by the medical school faculty where medical students have the opportunity to interact with graduate students in the academic environment. Add rows as needed for each campus. Campus Department or Program Table 6.7-3 | Residency and Fellowship Programs Source: School-reported List the CFPC and Royal College accredited residency or fellowship programs where medical students have the opportunity to interact with residents in clinical environments. Indicate the number of residents and fellows in the table. Add rows as needed for each campus. Name of the residency or fellowship program Number of Residents Accreditation status of the program Campus (add rows) and Fellows NARRATIVE RESPONSE a. Describe opportunities available for medical students to interact with students in graduate programs and how the medical school encourages such interactions. b. Provide examples of opportunities for medical students to interact with students in other health profession education programs in the first two years of the program and how the medical school encourages such interaction. CACMS DCI (November 2014) – Standard 6 Page 12 c. Provide examples of opportunities for medical students to interact with residents in clinical learning environments and how the medical school encourages such interaction. d. Describe how medical students are exposed to continuing medical education activities for physicians and note if student participation in any continuing medical education activities is permitted or required. CACMS DCI (November 2014) – Standard 6 Page 13 6.8 EDUCATION PROGRAM DURATION A medical education program includes at least 130 weeks of instruction. SUPPORTING DATA Table 6.8-1 | Number of Scheduled Weeks per Year Source: School-reported Use the table below to report the number of scheduled weeks of instruction in each academic year of the medical curriculum (do not include vacation time). Refer to the overview section if the medical school offers one or more parallel curricula. Number of Scheduled Weeks Year 1 Year 2 Year 3 Year 4 TOTAL: CACMS DCI (November 2014) – Standard 6 Page 14