Haemopoiesis & Anaemia - Weebly - Wk 1-2
advertisement

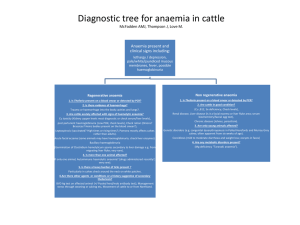
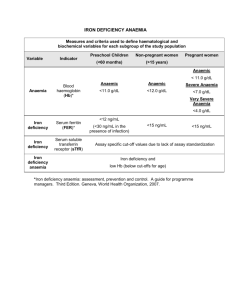
Haemopoiesis & Anaemia 1. Outline the process of haemopoiesis identifying the major cell types Haemopoiesis is a continuous, regulated process of blood cell production that includes cell renewal, proliferation, differentiation, and maturation. These processes result in the formation, development and specialisation of all the functional blood cells that are released from the bone marrow to the circulation. Process of haemopoiesis in Bone Marrow: Red haemopoiesis-active marrow (vs yellow haemopoiesis-inactive marrow) is present in adults in the sternum, skull, scapula, vertebrae, ribs, pelvic bones and the proximal ends of long bones. Fibroblasts extend along the perivascular space, creating a network for developing haemopoietic cells, macrophages, and mast cells. This network is composed into extravascular ‘cords’, with haemopoeitic cells developing in particular niches within the cords. The mature blood cells of the bone marrow eventually enter the peripheral circulation. This semifluid network is responsible for maintaining differentiation and proliferation, as well as being a supporting tissue for haemopoiesis. It is controlled by several cell types: 1. Endothelial cells: regulate the flow of particles across haemopoeitic spaces 2. Adipoctyes: secrete various steroids that influence erythropoiesis 3. Macrophages: function in phagocytosis/secretion of cytokines that regulate haemopoiesis 4. Osteoblasts: bone-forming cells 5. Osteoclasts: bone reabsorbing cells 6. Fibroblasts: formation of reticular fibres that form a lattice Process of haemopoiesis in Liver & Spleen: The liver is often involved in blood-related diseases (eg haemolytic anaemia), and is capable of extramedullary haematopoietic production in case of bone marrow shutdown. The spleen directs blood through a slow transit route through macrophage-lined cords before reaching the sinuses. The RBC’s have difficulty passing the tiny openings created by the endothelial junctions, and along with the acidic, hypoglycemic and hypoxis conditions, are subject to sufficient stress to lyse, allowing their contents to be provided for subsequent haemopoiesis. Major Cell Types Produced: The earliest recognisable bone marrow pluripotent stem cells are haemocytoblasts (blood+cell+precursor), which produce two populations of stem cells: 1. myeloid stem cells: create progenitor cells, which give rise to all blood cells except lymphocytes - see attached figure. 2. lymphoid stem cells: producing various classes of lymphocytes haemopoiesis is regulated by growth factors which act in synergy to determine cell function. RBCs: Erythropoiesis (formation of RBCs) requires adequate amino acids, iron and vitamins. Red cells conatin haemoglobin (Hb) which allows then to carry oxygen & carbon dioxide. The hormone erythropoietin (EPO) is a glycoprotein that stimulates erythropoiesis. It increases cell division in erythroblast stem cells & speeds up RBC maturation. It itself is stimulated by decreased oxygen supply to the kidneys. In the process of red blood cell maturation, a cell undergoes a series of eight differentiations. The first seven stages of development all occur within the bone marrow, and then the cell is released after stage 7 as a reticulocyte. Of circulating red blood cells there are ~1% reticulocytes. After 1-2 days these ultimately become "erythrocytes" or mature red blood cells. Platelets: The second type of progenitor cell, involved in blood clotting. WBCs: The third type of progenitor cell, producing neutrophils, eosinophils, basophils, and monocytes. All WBCs complete development in bone marrow, except monocytes which differentiate into free macrophages in peripheral tissue. Lymphopoiesis (formation of lymphocytes) can occur in the marrow & lymph tissues (lymph nodes, spleen, thymus) as lymphoid stem cells migrate to peripheral tissues. Their production as B, T or Natural Killer (NK) cells is regulated primarily by exposure to antigens. Nb during foetal development, haemopoiesis occurs in different places (& is different to adult haemopoiesis), and can be divided into the mesoblastic, hepatic and medullary phases. 2. List the major causes and types of anaemia and describe the roles of haematinic agents, decreased erythrocyte production and haemolysis in its classification Anaemia is defined as a qualitative or quantitative deficiency of hemoglobin, a protein found inside red blood cells (RBCs). Normal ranges are 130-170g/L (males) & 120-150g/L (females). Since hemoglobin normally carries oxygen from the lungs to the tissues, anaemia leads to hypoxia (lack of oxygen) in organs, and subsequent adaptive changes: - fluid shift from interstitiual to blood - increased cardiac output - increase rate & depth of breathing - redirection of blood from the peripheries - increased erythropoiesis Anaemia is a manifestation of disease, not a final diagnosis. The symptoms found in anaemic patient may be caused by the underlying disease or by the anaemia itself. The three main classes of anemia include: Reduced Haemoglobin levels: excessive blood loss – acute hemorrhage, or chronic: Referred to as Microcytic and Hypochromic anaemia, can be a result of: - Disorders of iron metabolism – gastric/duodenal ulcers, eating disorders, increased iron demand (pregnancy, infancy, menstruating women) - Disorders of Haeme sunthesis – sideroblastic anaemia, where iron accumulates in insoluble deposits - Disorders of globin synthesis: Thalassaemia (= inherited impared rate of synthesis of either alpha or beta globin chains) or Sickle Cell (= inherited defect of beta-globin chain replication). Commonly causes of chronic anaemia are linked to inflammation disease or malignancy, where dietary or age-related factors impact on RBC lifespan. Megaloblastic: impared red blood cell production (ineffective haemopoiesis) When RBC DNA synthesis and subsequent cell division is impaired by lack of folate or vitamin B12, megaloblastic anaemia develops. These deficiencies result in ineffective erythropoiesis where blood cells die in the marrow. Deficiencies may be dietary, or due to malabsorption in conditions such as gastritis. Pernicious anaemia results, and patients present with fatigue, weakness, shortness of breath. Reduced RBC levels: excessive blood cell destruction – haemolysis Haemolysis, increased or premature destruction of RBCs (referred to as haemolytic anaemia), is another form of erythropoiesis. It may result from congenital defects, or immune-mediated disease, membrane defects, enzyme deficiencies, infections, transfusion reactions, and hemorrhage. In this case RBC morphology is usually normal, but the cell count is low (normocytic-normochromic anaemia). A haematinic agent is one which increases the haemoglobin level & the number of RBCs in the blood. Examples include iron, B-vitamins. 3. Relate standard haematology reports to types of anaemia Full blood count parameters include: Packed Cell Volume (PCV): the proportion of the total blood volume taken by RBC: 0.4-0.5 Mean Cell Volume (MCV): the average volume of each REC: 80-100 femolitres (fL) Mean Cell Haemoglobin (MCH): av haemoglobin content of a RBC : 27-34 picograms (pg) Mean Cell Haemoglobin Concentration (MCHC): average haemoglobin concentration in a volume of packed RBC: 310-360 g/L. Hence anaemia can be classified as: Conditions for Microcytic / hypochromic MCV < 80 fL MCH < 27 pg Anameia types: Iron deficiency, Thalassemia Conditions for Normocytic / normochromic MCV: normal MCH: normal Anaemia types: Haemolytic anaemia Conditions for Macrocytic MCV > 100 fL Anaemia types: megaloblastic anaemia