some basic terms
advertisement
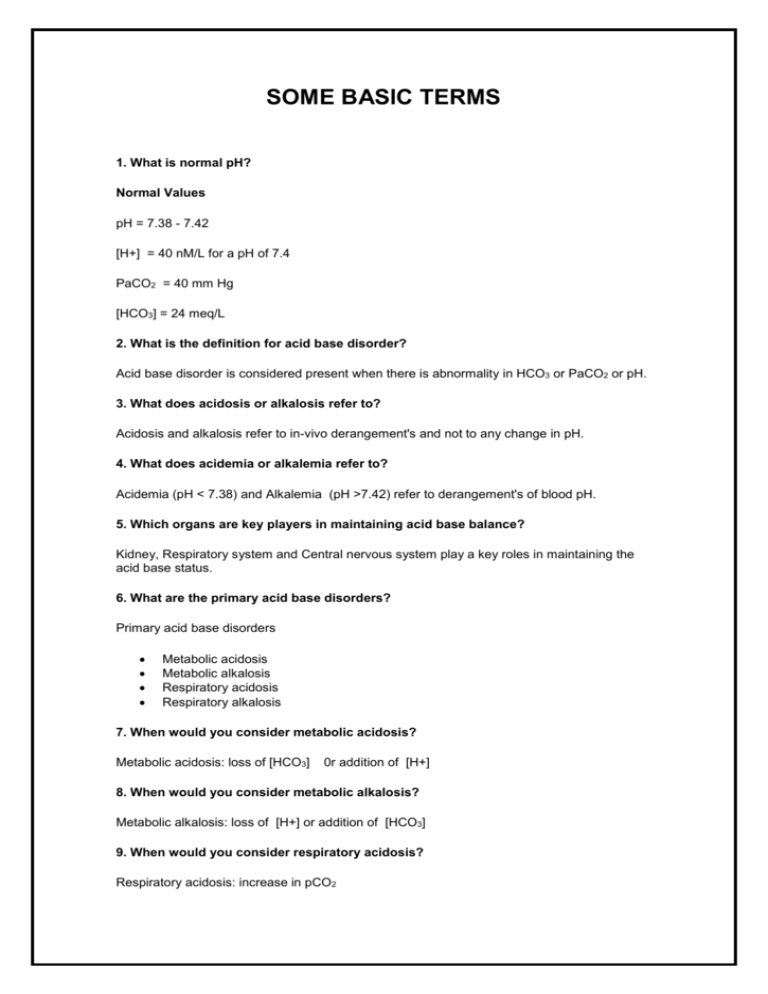
SOME BASIC TERMS 1. What is normal pH? Normal Values pH = 7.38 - 7.42 [H+] = 40 nM/L for a pH of 7.4 PaCO2 = 40 mm Hg [HCO3] = 24 meq/L 2. What is the definition for acid base disorder? Acid base disorder is considered present when there is abnormality in HCO3 or PaCO2 or pH. 3. What does acidosis or alkalosis refer to? Acidosis and alkalosis refer to in-vivo derangement's and not to any change in pH. 4. What does acidemia or alkalemia refer to? Acidemia (pH < 7.38) and Alkalemia (pH >7.42) refer to derangement's of blood pH. 5. Which organs are key players in maintaining acid base balance? Kidney, Respiratory system and Central nervous system play a key roles in maintaining the acid base status. 6. What are the primary acid base disorders? Primary acid base disorders Metabolic acidosis Metabolic alkalosis Respiratory acidosis Respiratory alkalosis 7. When would you consider metabolic acidosis? Metabolic acidosis: loss of [HCO3] 0r addition of [H+] 8. When would you consider metabolic alkalosis? Metabolic alkalosis: loss of [H+] or addition of [HCO3] 9. When would you consider respiratory acidosis? Respiratory acidosis: increase in pCO2 10. When would you consider respiratory alkalosis? Respiratory alkalosis : decrease in pCO2 11. What are the required lab values and historical information you need to assess acid base disorders? Recquired lab values/information Arterial blood gases: pH, PaCO2,calculated bicarb Electrolytes: Na, K, Cl, HCO3 BUN, Glucose, Creatinine Clinical history 12. What are anions? List the anions? Anions Chloride Bicarbonate(Total CO2) Proteins Organic acids Phosphates Sulfates 13. What are cations? List the cations? Cations Sodium Potassium Calcium Magnesium 14. What is anion gap? Anion gap (AG) Electrochemical balance: the total anions are the same as total Cations. An imbalance between Sodium, Chlorides and Total CO2.is measured as anion gap. Sum of Cations minus anions (Na+K)-(CL+HCO3) Use the measured total CO2 from venous blood as HCO3 anion gap is an artifact because some anions are not measured gap is mainly due to unmeasured proteins, phosphates and sulfates Normal anion gap is 8-12 meq/L (Varies from Lab to Lab) 15. How do you calculate anion gap? For practical purposes anion gap is calculated using only Sodium, Chlorides and Total CO2.((140-(104+24)) = 12. 16. What are the compensatory measures for acid base disorders? Compensatory measures Buffering---occurs immediately Respiratory regulation of pCO2 is intermediate (12-24 hours) Renal regulation of [H] and [HCO3] occurs more slowly (several days) 17. What is difference between bicarbonate value reported in arterial blood gases and bicarbonate reported in electrolytes? Calculated bicarbonate: calculated using the H-H equation From arterial blood Total CO2: measured from venous blood includes bicarbonate and dissolved carbon dioxide runs slightly higher than calculated value from nomogram 18. What is the metabolic compensation for acute respiratory acidosis? How do you assess whether it is appropriate? Hypoventilation: Respiratory acidosis Expected bicarbonate decrease No time for renal compensation. o for acute CO2 retention (Buffering) Expected decrease in pH = 0.08 x (measured PaCO2 - 40) 19. What is the metabolic compensation for chronic respiratory acidosis? How do you assess whether it is appropriate? Expected bicarbonate elevation for chronic CO2 retention (Renal compensation) is o 0.35 x (current PaCO2-normal PaCO2) For example: 0.35 x ( 60-40)=0.35x20=7 meq/l Chronic: Expected drop in pH = 0.03 x (measured PaCO2 - 40) 20. What is the metabolic compensation for acute respiratory alkalosis? How do you assess whether it is appropriate? Hyperventilation: The expected fall in bicarb for acute decrease in PaCO2 (Buffering) is 0.2 x (normal PaCO2-observed PaCO2) 21. What is the respiratory compensation for chronic respiratory alkalosis? How do you assess whether it is appropriate? The expected fall in bicarb for chronic hyperventilation: decrease in PaCO2 (Renal compensation) is : 0.5 x (normal PaCO2-observed (PaCO2) Expected pH: Compensation is almost complete 22. What is the respiratory compensation for acute metabolic acidosis? What are the sensors and effectors for this response? When it comes to metabolic acid base disorders we usually do not think in terms of acute and chronic. Most of them are chronic. Acidosis increases respiratory drive, alveolar ventilation and gets rid of Carbonic acid. Respiratory system can never completely compensate for a metabolic defect. Respiratory compensation attempts to maintain pH in a reasonable range. 23. What is the respiratory compensation for chronic metabolic acidosis? How do you assess whether it is appropriate? Metabolic acidosis Expected PaCO2 decrease: (Normal bicarb-Observed bicarb) x 1.2 You can use the following crude formula 0.1 change in pH 10 mm change of PaCO2. If all else is well the PaCO2 should be the same as decimal values of pH i.e. for a pH of 7.28, the CO2 levels would be 28 mmHg. Estimation of expected PaCO2 for a given acidic pH also enables us to determine whether respiratory compensation is appropriate. Compensation is never complete. If the pH is normal there is probably a superimposed second acid base disturbance. 24. What is the respiratory compensation for acute metabolic alkalosis? How do you assess whether it is appropriate? When it comes to metabolic acid base disorders we usually think in terms of acute and chronic. Most of them are chronic. 25. What is the respiratory compensation for chronic metabolic alkalosis? How do you assess whether it is appropriate? Metabolic alkalosis Only when it is severe and protracted It is unusual to see CO2 retention (I don't agree with Books and others) Less predictable 26. What is bicarbonate gap? The bicarbonate gap useful in identifying mixed acidbase disorders in single acidbase disorder the difference between anion gap and the change in total CO2 should be negligible in other words change in total CO2 (Normal total CO2-observed total CO2) should be equal to anion gap. Excess bicarbonate gap suggests metabolic alkalosis Decrease in the gap suggests metabolic acidosis 27. Explain renal mechanism for regulation of acid base disorders? Major functions 1. 2. 3. Reclamation of filtered bicarbonate Generation of new bicarbonate in the distal tubule to replenish body buffer stores Excretion of Acid o titratable acidity o ammonium formation o free H+ excretion a dumb kidney is usually better than a smart Doctor Reclamation of filtered bicarbonate o 4000 meq / day in normal persons 28. What are the common causes for high anion gap metabolic acidosis? Increased anion gap Either due to addition or reduced excretion of acid reduced excretion of inorganic acids o renal failure retention of sulphates and phosphates impaired net acid excretion (ATN) impaired ammonia excretion (Chronic renal failure) accumulation of organic acids o ketoacidosis diabetic starvation alcoholic o lactic acidosis (impaired cellular respiration with anaerobic glycolysis) shock septicemia profound hypoxemia o ingestion salicilates methanol 29. What are the common causes for normal anion gap metabolic acidosis? Normal anion gap Either due to loss or failure to generate bicarbonate abnormally high bicarbonate loss o Kidney fails to reabsorb renal tubular acidosis o Kidney fails to regenerate Diuretics o extra renal loss of bicarbonate Diarrhea ileal drainage o acidifying salts have been added hyperalimentation ammonium chloride 30. What are the common causes for metabolic alkalosis? Metabolic alkalosis loss of hydrogen ions from the body o vomiting o gastric suction net rate of renal bicarbonate generation is greater than normal o volume contraction o potassium depletion o increased delivery of sodium to distal tubule (Loop diuretics) o minerelocorticoid excess Rapid correction of ventilation in a patient with chronic CO2 retention (posthypercapnic alkalosis) In severe alkalosis Cardiac arrhythmia Hypoventilation 31. What are the common causes for respiratory acidosis? Respiratory Acidosis Decreased alveolar ventilation acute respiratory acidosis (normal bicarbonate) o narcotic overdose o respiratory muscle paralysis o acute airway obstruction Chronic respiratory acidosis (increased bicarbonate) o COPD o kyphoscoliosis o Obesity hypoventilation syndromes End stage restrictive pulmonary disease 32. What are the common causes for respiratory alkalosis? Respiratory alkalosis Acute hyperventilation (Light headedness, paresthesias, circumvoral numbness, tingling of extremities and tetany.) o pain o acute salicylism o fever o sepsis o CHF o PE o Mechanical ventilation o anxiety (breath with a paper bag) Chronic hyperventilation o high altitude o hepatic insufficiency o pregnancy o Diffuse interstitial fibrosis 33. What are the factors that stimulate kidney to excrete acid? Excretion of acid stimulated by Acidemia Hypercapnea Volume depletion Chloride depletion ? Hypokalemia Aldosterone 34. What are the factors that inhibit kidney to excrete acid? Excretion of acid inhibited by Alkalemia Elevated [HCO3] Hypocapnea ? Hyperkalemia 35. How do you determine whether an acid base disorder is simple or mixed? Single acid base disturbance: the change in concentration of one anion is balanced by a reciprocal change in one other anion. Mixed acid base disturbance: the anion patterns are more complex Bicarbonate gap is not equal to anion gap o Excess bicarbonate gap suggests metabolic alkalosis o Decrease in the gap suggests metabolic acidosis CO2 levels not in keeping with estimates Bicarbonate levels as estimated by nomogram from arterial blood gas significantly varies from venous total CO2 (bicarbonate) 36. Explain CSF barrier for acid base disorders. How does it come into play clinically? Blood brain barrier Freely permeable to CO2 o responses occur instantaneously lag in equilibrating with bicarbonate o early stages of metabolic acidosis 2-3 hour lag in respiratory response o hyperventilation may persist even after correction of metabolic acidosis 37. Give me your step by step approach to interpreting acid base disorders. Approach to interpreting Acid-base disturbance 1. 2. Is the patient Acidemic or Alkalemic Identify the primary Acidbase disorder by evaluating HCO 3 and PaCO2 What is the [HCO3] o o Elevated------Metabolic alkalosis if alkalotic Decreased ---- Metabolic acidosis if acidotic What is the PaCO2 o o Elevated ---Respiratory acidosis if acidotic Decreased --- Respiratory alkalosis if alkalotic 3. 4. 5. 6. What is the anion gap (to determine etiology of Metabolic acidosis) What is the bicarbonate gap (to evaluate mixed disorders) Is the degree of compensation what you expect (appropriate)? Identify and understand the pathophysiology for the disorder 38. Describe the buffer system. Buffering-Bicarbonate is in both ICF and ECF and participates in buffering capacity Extracellular almost entirely through bicarbonate whose concentration highest of all buffers small contribution from phosphate Intracellular Buffer systems Hemoglobin can directly buffer protons o H+ entry into RBC matched by exit of Na and K+ 39. Describe how kidney excretes acid. Excretion of Acid Titratable acidity o mainly with phosphate o 10-30 meq / day Ammonia formation o H+ combines with N3HO from NH4+ which is trapped in tubule o baseline 30-60 meq / day, but may rise to as much as 250-400 meq / day Excretion of free [H] maximally acidified urine -- pH = 4.5 -- will account for only 0.04 meq +H / L urinary acidification is important in order to titrate protons into phosphate and ammonium 40. What is the relationship between Ventilation and pCO2 PaCO2 is inversely proportional to ventilation Ventilation increases in response to a drop in pH o respiratory center in medulla o responds to pH "intermediate" between that of CSF and plasma o response is rapid o response is more predictable for falls in pH o for increase in pH ventilation decreases only when it is severe and protracted Interrelationship between acute changes in CO2 and pH pCO2 pH 70 7.10 60 7.20 50 7.30 40 7.40 30 7.50 20 7.60 This formula is usable because in the range of pH values we usually deal with, there is nearly linear relationship between pH and pCO2. DONE BY : FATIMAH ALSHEHRI ,PHARM.D FACULTY OF PHARMACY, KAU 2014