DOCX ENG

H- 14 : infectious complications
J- 05 : other recommendations
Post-transplant Pneumocystis jirovecii pneumonia —a re-emerged public health problem?
Jeremy R Chapman 1 , 2 , Deborrah J Marriott 3 , Sharon C-A Chen 2 and Peter S MacDonald 3 on behalf of TSANZ and the consensus meeting attendees
Kidney International (2013) 84, 240 –243
1. 1 Centre for Transplant and Renal Research, Westmead Hospital, Westmead, New
South Wales, Australia
2. 2 Department of Infectious Diseases, Westmead Hospital, Westmead, New South
Wales, Australia
3. 3 Departments of Cardiology and Infectious Diseases, St Vincent’s Hospital,
Darlinghurst, New South Wales, Australia
Correspondence: Jeremy R. Chapman, Centre for Transplant and Renal Research,
Westmead Hospital, Westmead, New South Wales 2145, Australia. E-mail:
Jeremy.chapman@swahs.health.nsw.gov.au
ABSTRACT
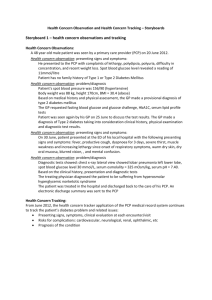
Pneumocystis jirovecii is a unicellular organism that in individuals with impaired immunity may cause pneumonia that can progress from minor illness to severe inflammatory pneumonia (PCP) with respiratory failure and death. Despite antimicrobial prophylaxis, which has reduced the incidence of PCP, clusters of late infections have been reported among kidney transplant recipients worldwide. A nosocomial PCP cluster was first recognized in
2010 at a Sydney hospital, but PCP clusters have since occurred in almost half of the renal transplant units on the eastern Australian seaboard, refocussing attention on optimal prophylaxis regimens and the likelihood of patient-to-patient transmission. A consensus meeting was conducted to derive the lessons from this experience for responding to PCP outbreaks. These included: (1) acting quickly —clusters of PCP in kidney transplant recipients with patient-to-patient transmission required transplant programs to act quickly to institute prophylactic and treatment measures; (2) instituting universal prophylaxis for all patients seen in the affected unit; (3) reducing patient-to-patient transmission via airborne droplets in the outpatient waiting areas; (4) examining the P. jirovecii genotypes. The meeting also considered recommendations for the duration of prophylaxis following de novo transplant and, for the individuals in whom long term prophylaxis is required, separating units with and without clusters of PCP.
Keywords:
consensus; epidemic; nosocomial; risk factors
COMMENTS
Pneumocystis infection is a life threatening pulmonary complication in transplant patients.
Pneumocystis jirovecii is a unicellular organism that may be found in the human respiratory tract. It is now classified as a fungus but cannot be cultured in the routine microbiology laboratory. Infection is worldwide, and ~80% of children have antibodies by the age of 4 years, whereas up to 20 –50% of healthy adults are colonized. Most immunocompetent individuals clear the infection without any symptoms; however, with impaired immunity as a result of human immunodeficiency virus (HIV)/AIDS, cancer, or organ transplantation, P. jirovecii pneumonia (PCP) can progress from minor illness to severe inflammatory pneumonia with respiratory failure and death.
Reduce patient-to-patient transmission : Transmission occurs via airborne droplets, and in some clusters it could be traced to patient-to-patient contact in outpatient waiting areas.
The approach to prophylaxis has varied with patient risk factor profile, organ transplanted, and local policy. Alt hough low CD4 counts (<200 × 10 9 ) are strongly predictive of risk among people with HIV, they are not a biomarker in organ transplantation.
Prophylactic antimicrobial agents
PCP prophylaxis among solid-organ recipients has been guided by the experience in preventing PCP in individuals with HIV/AIDS using cotrimoxazole (trimethoprimsulfamethoxazole). Second-line treatments have included dapsone alone or dapsone/pyrimethamine combination, inhaled pentamidine, and atovaquone.
An important unanswered question that recent case clusters have highlighted is the optimal duration of post-transplant prophylaxis. There is no standardized approach to prophylaxis within specific organ transplant groups.
Pr. Jacques CHANARD
Professor of Nephrology