Opportunistic Infections: Diagnosis & Management
advertisement
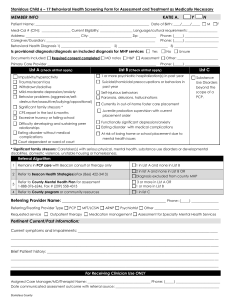
Introduction to the diagnosis and management of common opportunistic infections (Ols) Module 4 Sub module OIs Opportunistic Infections Pneumocystis carinii pneumonia (PCP) Penicilliosis Recurrent pneumonia Cryptococcus Toxoplasmosis Oesophageal candidasis Mycobacterium Avium Complex (MAC) Cytomegalovirus (CMV) Natural course & common clinical manifestations 1000 900 800 700 600 500 400 CD4 300 COUNT 200 100 50 <50 0 TB TB HZV OHL Oral candida PCP Cryptococcal meningitis PPE CMV MAC TB Cryptosporidial diarrhea 0369 1 Months 2 3 4 5 6 Years TB 7 8 9 10 Common opportunistic infections The most common opportunistic infections Tuberculosis PCP Cryptococcosis Candidiasis, oesophageal Pneumonia, recurrent 0 5000 10000 15000 20000 Division Epidemiology, Department of Communicable Diseases Control, MOPH, Thailand 25000 Pneumocystis Carinii Pneumonia (PCP) Organism Pneumocystis Carinii Very common CD4 count < 200 cells Absolute lymphocyte count <1200 Differentiation of bacterial pneumonia & PCP Bacterial pneumonia Pneumocystis pneumonia Onset: Acute: Hours to days Sub-acute: days to weeks Cough: Productive Non-productive Pleuritic chest pain: Common Un-common Shortness of breath: With chest pain Prominent on exertion Common Very uncommon Usual Very uncommon Often increased Normal or low Not helpful Usually <200/µl Pleural effusion: Focal chest Xray infiltrate: White blood cell count: CD4 count: PCP Bacterial pneumonia Pneumocystis carinii pneumonia PCP Diagnosis – Frequently clinical – Typical symptoms – Response to treatment – Microscopic demonstration of P. carinii in lung secretions/tissue – Culture unavailable PCP Diagnosis – special methods to obtain specimens are necessary • Induced sputum/B.A.L./Biopsy DDX: – MTB, bacterial pneumonia, fungal pneumonia, lymphoma, KS PCP Treatment – Trimethoprim-Sulfamethoxazole – drug of choice (iv 15 mg/kg/day or oral 2 DS tablets tid) – 3 weeks recommended – Allergy to TMP-SMX – Corticosteroids if severely hypoxic PCP Alternative treatment for allergic patients (all for 21 days) • pentamidine • dapsone + trimethoprim • clindamycin + primaquine • atovaquone – less effective PCP Prognosis: – 100% fatal untreated – Level of hypoxaemia best predicts outcome Secondary Prophylaxis – co-trimoxazole 1-2 tabs daily – Dapsone 100 mg daily – aerosilized pentamidine 300 mg monthly Penicilliosis Organism: Penicillium marneffei Endemic area: – SE Asia (Northern Thailand, Southern China, Vietnam, Indonesia, Hong Kong) – 3rd most common OI in Northern Thailand CD4 count < 100 cells Penicilliosis Clinical symptoms: – Fever (99%) – papulo-necrotic skin lesions (71%) – weight loss (76%) – anaemia (77%) – lymphadenopathy (58%) – hepatomegaly (51%) – productive cough – lung disease Penicilliosis Diagnosis – Presumptive:microscopy on smear – Definitive: culture – DDx: • other disseminated mycobacterial or fungal disease Penicilliosis Penicilliosis Penicilliosis Treatment: – amphotericin B IV for 6-8 weeks – amphotericin IV for 2 weeks + itraconazole 400 mg orally daily for 10 weeks In mild cases: – Itraconazole 400 mg orally daily for 8 weeks Penicilliosis Prognosis: – high mortality in patients with delayed diagnosis/treatment. Secondary prophylaxis – Itraconazole 200 mg orally daily for life – > 50% relapse at 1 year without secondary prophylaxis Primary prophylaxis - not routinely indicated Recurrent Pneumonia Definition > 1 episode of pneumonia in 12 months Epidemiology – common in HIV infected patients – S. pneumoniae and H. influenzae at least 20 times more common in HIV – Pneumococcal bacteraemia rate 100 times higher in AIDS v. non-AIDS Clinical – clinical presentation same as for non-HIV Recurrent Pneumonia Organism S. pneumoniae Stage of HIV Infection early and late late H. influenzae S. aureus enteric gram neg rods M.TB early and late Rhodococcus equi late Nocardia asteroides late Recurrent Pneumonia RUL infiltrate caused by Nocardia RUL infiltrate of TB TB with cavitation Disseminated candidiasis Recurrent Pneumonia Diagnosis – clinical evaluation, sputum smear/culture, CXR, blood culture Treatment – as per local guidelines for pneumonia in non HIV Prevention – Co-trimoxazole prophylaxis protects against recurrent pneumonia – Improve immune function with Cryptococcosis Clinical features – fever – headache – signs of meningism & photophobia – malaise, nausea and vomiting – alteration of mental status Cryptococcosis Diagnosis – Lumbar puncture - India ink staining – Cryptococcal antigen, and culture – Cryptococcal Ag highly sensitive and specific (CSF and blood) Titre > 1:8 presumptive evidence of infection Differential Diagnosis – pyogenic meningitis, TB meningitis, toxoplasmosis, neurosyphillis Encapsulated yeast of Cryptococcus neoformans in CSF India ink preparation Cryptococcosis Cryptococcosis Cryptococcosis Treatment of Cryptococcal Meningitis – Induction phase • amphotericin B iv daily for 14 days • consider adding 5-flucytosine (5-FC) – Consolidation phase • fluconazole 400 mg po daily for 8 week Cryptococcosis Prognosis – mortality rates as high as 30% despite therapy Secondary Prophylaxis – fluconazole 200-400 mg daily – itraconazole 100-200 mg po bid (less effective than fluconazole) Toxoplasmosis Organism: Toxoplasma gondii Epidemiology: – Cats the definitive hosts – Ingestion of faecally contaminated material – Ingestion of undercooked meat CD4 count < 100 Toxoplasmosis Clinical Features: – encephalitis the most common manifestation (90%) • fever (70%), headaches (60%), focal neurological signs, reduced consciousness (40%), seizures (30%) • Constellation of fever, headache, and neurological deficit is classic – chorio-retinitis – pneumonitis – disseminated disease Toxoplasmosis Diagnosis – positive serology with typical syndrome – suggestive CT/MRI scan: • multiple, bilateral cerebral lesions; hypodense with ring enhancement – Differential diagnosis – CNS lymphoma, tuberculoma, fungal abscess, cryptococcosis, PML Toxoplasmosis Toxoplasmosis Toxoplasmosis- Response to therapy Toxoplasmosis Treatment – Empirical therapy reasonable as trial, at least for 2 weeks – Pyrimethamine plus folinic acid plus either sulfadiazine or clindamycin – 6 weeks therapy at least, or until 3 weeks after complete scan resolution – Corticosteroids for raised intracranial pressure Toxoplasmosis Secondary Prophylaxis – Essential because latent (cyst) phase cannot be erdicated – Pyrimethamine plus folinic acid plus sulfadiazine (or clindamycin) – relapse occurs in 20-30% of patients despite maintenance therapy – Improve immunity with HAART Oesophageal Candidiasis Organism: Candida yeast CD4 count < 200 Clinical symptoms – dysphagia, retrosternal pain – oral thrush in 50-90% – endoscopy • ulceration • plaques Oesophageal Candidiasis Oesophogeal Candidiasis Diagnosis – oral thrush and dysphagia sufficient – consider endoscopy if • symptoms without oral thrush • failure of empirical antifungal therapy – Treatment – Fluconazole 200-400 mg /day until resolved – Long term suppressive therapy if recurrent Mycobacterium Avium Complex (MAC) Organism: M.avium/M. intracellulare CD4 count: < 100 cells Clinical symptoms – fever & night sweats – anorexia & weight loss – Nausea & abdominal pain & diarrhoea – lymphadenopathy – hepatosplenomegaly – anaemia MAC Diagnosis; – Blood cultures – 2 blood cultures will detect 95% of cases – microscopy and culture of bone marrow, lymph nodes DDx: – MTB, disseminated fungal disease, malignancy MAC Treatment Option 1 clarithromycin + ethambutol Option 2 clarithromycin + ethambutol + rifabutin Option 3 HAART MAC Prognosis (pre HAART): – Untreated: 4 months – Treated: 8 months Secondary Prophylaxis – lifelong maintenance required CMV Disease Epidemiology: – a worldwide human herpes virus – 3 periods of transmission • perinatal, chidhood, reproductive years – in LDC’s, > 90% of children infected by 2 yo CD4 < 50 emerging pathogen in SE Asia? CMV Retinitis Clinical: – field defects – floaters – blurred vision – rapid deterioration in vision Diagnosis: – typical fundoscopic appearance in a seropositive patient CMV Retinitis Toxoplasma Retinitis Managing CMV retinitis Treatment – expensive and toxic – maintenance therapy essential – ganciclovir/foscarnet – IVI or intra-vitreal – HAART CMV Disease Other clinical manifestations of CMV – oesophagitis – colitis – sclerosing cholangitis – encephalitis – polyradiculomyelopathy – adrenalitis – pneumonitis Opportunistic infection prophylaxis in the era of HAART Stopping rules – Fluconazole after CD4 > 100 for 3 months – Azithromycin after CD4 > 100 for 3 months – Cotrimoxazole after CD4 > 200 for 3 months Cessation of secondary prophylaxis more controversial Stopping prophylaxis should always be Opportunistic Infections Key Points Very uncommon in those on successful ARV Predictable according to CD4 count Prevention better than cure Secondary ‘maintenance’ therapy required Educate patients