Endo 21 Pancreas and Adrenal Morphology Pancreas has head
advertisement
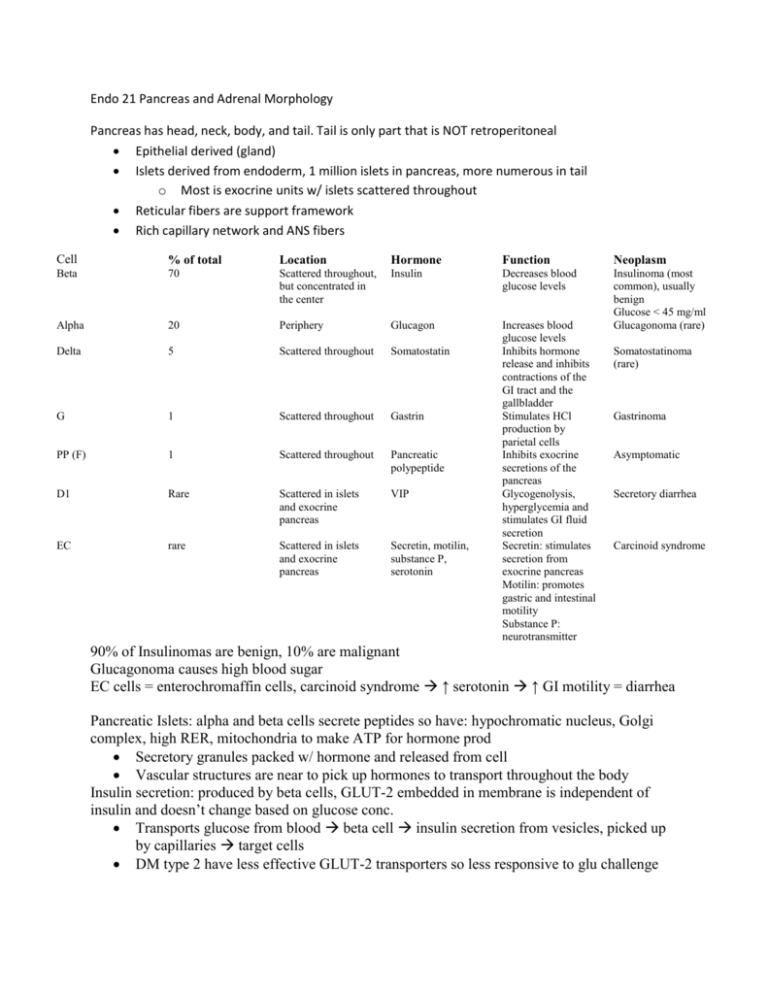
Endo 21 Pancreas and Adrenal Morphology Pancreas has head, neck, body, and tail. Tail is only part that is NOT retroperitoneal Epithelial derived (gland) Islets derived from endoderm, 1 million islets in pancreas, more numerous in tail o Most is exocrine units w/ islets scattered throughout Reticular fibers are support framework Rich capillary network and ANS fibers Cell % of total Location Hormone Function Neoplasm Beta 70 Scattered throughout, but concentrated in the center Insulin Decreases blood glucose levels Alpha 20 Periphery Glucagon Delta 5 Scattered throughout Somatostatin G 1 Scattered throughout Gastrin PP (F) 1 Scattered throughout Pancreatic polypeptide D1 Rare Scattered in islets and exocrine pancreas VIP EC rare Scattered in islets and exocrine pancreas Secretin, motilin, substance P, serotonin Increases blood glucose levels Inhibits hormone release and inhibits contractions of the GI tract and the gallbladder Stimulates HCl production by parietal cells Inhibits exocrine secretions of the pancreas Glycogenolysis, hyperglycemia and stimulates GI fluid secretion Secretin: stimulates secretion from exocrine pancreas Motilin: promotes gastric and intestinal motility Substance P: neurotransmitter Insulinoma (most common), usually benign Glucose < 45 mg/ml Glucagonoma (rare) Somatostatinoma (rare) Gastrinoma Asymptomatic Secretory diarrhea Carcinoid syndrome 90% of Insulinomas are benign, 10% are malignant Glucagonoma causes high blood sugar EC cells = enterochromaffin cells, carcinoid syndrome ↑ serotonin ↑ GI motility = diarrhea Pancreatic Islets: alpha and beta cells secrete peptides so have: hypochromatic nucleus, Golgi complex, high RER, mitochondria to make ATP for hormone prod Secretory granules packed w/ hormone and released from cell Vascular structures are near to pick up hormones to transport throughout the body Insulin secretion: produced by beta cells, GLUT-2 embedded in membrane is independent of insulin and doesn’t change based on glucose conc. Transports glucose from blood beta cell insulin secretion from vesicles, picked up by capillaries target cells DM type 2 have less effective GLUT-2 transporters so less responsive to glu challenge Target cell response to insulin: must have a receptor, GLUT-4 transporters are dependent on insulin, in presence of insulin GLUT-4 upregulated on plasma membrane to ↑ glucose uptake, when insulin levels drop some GLUT-4 receptors internalized DM pts have defective signaling, GLUT-4 doesn’t get incorporated into membrane Could be defect in insulin receptor Counter insulin hormones: glucagon, cortisol, growth hormone, and epinephrine Complications of DM: pt compliance is #1 factor neuropathy, loss of autonomic control (bowel and bladder), eye problems (retinopathies, glaucoma), kidney failure, gangrene/infection, lower limb amputation is common, atherosclerosis common @ early age, MI @ early age Suprarenal arteries: IPAR: IP = Inferior Phrenic, parent for superior suprarenal arteries A = aorta, parent vessels for middle suprarenal arteries R = renal, parent vessels for inferior suprarenal arteries Veins: left suprarenal vein empties into left renal vein (longer than right) Only 1 vein drains each adrenal gland o Right suprarenal vein inf vena cava, much shorter, more easily torn In adrenal gland, delicate arteries penetrate capsule (subcapsular arterial plexus) One set will form cortical sinusoidal capillaries – bathe cortical cells Medullary arteries travels thru cortex medullary area o Also supplied by sinusoidal capillaries after passing thru cortex Functional cells are chromaffin cells Nerves of Suprarenal glands: segmental levels are variable Medulla w/ modified postganglionic nerve cells Need to be supplied by preganglionic nerve cells T8-T12 and L1 are common segments supplying these cells On MRI left adrenal gland looks like “Y” and right looks like Mercedes Benz sign Adrenal gland is 5 grams, same as nickel 90% cortex 10% medulla Cortex from mesoderm, medulla from neuroectoderm Chromaffin cells (in medulla) have neuroectoderm source and neural crest cells move from sympathetic ganglia to become chromaffin cells Move from ganglia adrenal glands 2 signaling molecules for development of chromaffin cells – cortisol and NGF Extra adrenal tissue occurs when cells travel to other parts of body, possible areas of ectopic medullary tissue along path of aorta Btw bifurcation of aorta and inferior mesenteric artery is Organ of Zuckerkandl – no cortical tissue, medullary only Tumor of ectopic tissue is pheochromocytoma Cortical tissue or medullary tissue can develop by ovaries or male genitalia Adrenal Cortex: 3 zones: Superficial to deep: Glomerulosa, fasiculata, and reticularis Fasiculata is thickest, 78% of cortex, glomerulosa 15%, reticularis 7% Glomerulosa = aldosterone, Fasciculata = glucoocorticoids and small amts androgens, Reticularis = androgens and small amts glucocorticoids Medulla produces and secretes NE and epi Steroid-secreting cells of zona fasciculate has lots of smooth ER, mitochondria has tubular cristae, nucleus has euchromatin, lipid droplets contain precursor for steroid synth o Steroid hormones diffuse across membrane, not stored, body systems signal steroid production Factors affecting cortex: Angiotensin and K ions have greatest influence on aldosterone secretion o ACTH influences the production of aldosterone but NOT the release o Fasciculata and reticularis, ACTH influences synthesis of cortisol and androgens o Too much ACTH most effect on inner 2 zones hypertrophy and thicken o Glomerulosa is basically unaffected o ACTH is low, fasciculata and reticularis will shrink Feedback control of ACTH and cortisol secretion: too much cortisol inhibits ant pit and hypothalamus ↓ amts of ACTH and CRH released Aldosterone regulates extracellular fluid volume, fluid ↓ aldosterone release ↑ Effect of cortisol of metabolic fuel flow: shift metabolic to use free fatty acids to conserve carbs Uses fat and protein as fuel Liver mainly unaffected by cortisol to maintain gluconeogenesis Excessive amts fat deposition, can dvlp striae ↑ appetite ↑ caloric intake ↑ blood volume red face Synthetic pathway for DA, NE, and Epi; Cortisol required by enzyme to convert NE epi Tyrosine DA NE and Epi in cytosol concentrated & stored in secretory granule Blood carries cortisol from adrenal cortex to medulla to act on enzyme Tumor of Organ of Zuckerkandl expected to ↑ NE release bc low levels of cortisol d/t no cortical tissue in tumor, therefore epi prod will not ↑ Catecholamines are released bound to chromogranin A Pheochromocytoma (tumor of chromaffin cells) will ↑ synthesis and release of catecholamines and ↑ prod of catecholamine binding proteins Congenital Adrenal Hyperplasia: occurs during development affecting fetus Precursor steroids cortisol or androgens W/ disease can’t make cortisol so get ↑ androgens o Body senses lack of cortisol and ↑ ACTH release from adenohypophysis hypertrophy and hyperplasia of androgen-producing areas too much androgens o Too much androgens ambiguous genitalia, male if testes in scrotum