ORA Signal
advertisement

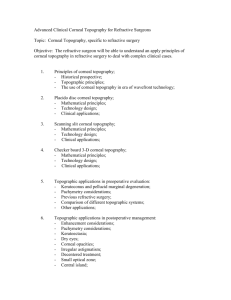
ESCRS 2012 - Course IC 71 - Treatment strategy for custom ablation of visually disturbing irregular astigmatism after refractive surgery and in keratoconus Tomography and Biomechanical Assessment for Enhanced Planning Therapeutic Corneal Procedures Renato Ambrósio Jr, MD, PhD Professor of Ophthalmology of Federal University of São Paulo and Pontific Catholic Federal University of Rio de Janeiro Scientific Coordinator of the Rio de Janeiro Corneal Tomography and Biomechanics Study Group Director of Cornea and Refractive Surgery of Instituto de Olhos Renato Ambrósio, Visare Personal Laser and Refracta-RIO Correspondence to: Renato Ambrósio Jr Rua Visconde de Pirajá 595/808 – Ipanema Rio de Janeiro, RJ – 22410-002 Dr.renatoambrosio@gmail.com I. Why it is critical to evolve on the diagnosis in Refractive Surgery? Refractive surgery determined the need for understanding corneal shape (geometry), optical (power and quality - aberrations) and biological (healing and biomechanical) properties. Parallel to progresses on corneal semiology, there has been an associated increase in understanding other issues, such as corneal wound healing and biomechanics. Also, sphere and cylinder refraction evolved to the measurement of wavefront optical aberrations of the whole eye. Integration of corneal and whole eye optics measurements enables calculations of internal optics. Understanding the clinical relevance of these new methodologies has been a critical part of the evolution in this field! Ectasia is a very severe complication after keratorefractive procedures. Risk factors have been described based on surgical parameters and preoperative screening tools: topography (axial anterior curvature map – typically from Placido´s reflection) and single point central pachymetry. However, there are many cases that had ectasia without risk factors. There are also cases with one or more risk factors with excellent and stable long-term outcomes. Thereby, new technologies have been needed to enhance sensitivity and specificity for screening refractive candidates, as well as to provide objective parameters to choose and plan the refractive procedure (increasing efficacy and safety) and to evaluate clinical results. However, we believe that corneal topography and central thickness measurements do NOT provide enough clinical data for decision making if we should ablate FFK cases. Interestingly, there are also many reports and there is a major concern regarding non-explained cases of ectasia after LASIK (and also surface ablation) with normal preoperative topography and low risk scores. This is why we considered, 5 years ago, the need for advanced technologies to screen refractive candidates and started working with new diagnostic tests such as the non contact air puff tonometer with corneal biomechanical measurements (Ocular Response Analyzer [Reichert], Corvis ST [Oculus]) and the rotating Scheimpflug Corneal Tomography (Pentacam [Oculus]). Other imaging technologies such as the OCT, very high frequency ultrasound tomography and also other biomechanical tests, such as the electronic speckle pattern interferometry, would definitively add to the exams that may be used for enhanced screening of refractive candidates. Other approaches for the evolution for the enhanced evaluation of ectasia would include keratocyte counts, in vivo molecular biology testing of the cornea and eventually genetic testing. II. Defining: Forme-fruste Keratoconus (FFK) Forme-fruste is an incomplete or abortive form of a disease or condition Forme-fruste keratoconus (FFK) is defined as an incomplete or abortive form of keratoconus. This condition was described by Amsler in 1937. Krachmer advocates that the term “mild” may be more appropriate (Cornea Day, Pre AAO 2008), based on the fact that mildly irregular mires with inferior steepening is keratoconus. “Early” is not appropriate as well since “early” implies progression, which cannot be anticipated. “Sub-clinical” keratoconus may be used to describe mild disease in asymptomatic patients with normal BSCVA. In this scenario (FFK), there is little to no slit lamp findings (Fleischer ring [iron line], Vogt's striae), and typically the patient has normal BSCVA. Prominent corneal nerves are very common among such cases but this is a non specific finding. III. How is the Diagnosis of FFK made? Corneal Topography and Beyond… This is possible to detect “mild” keratoconus cases or (FFK) without corneal topography. (Note that Amsler was able to describe FFK in 1937, much before the advent of computerized topography). Scissoring of the retinoscopic reflex, careful slit lamp biomicroscopy, central and peripheral corneal thickness measurements, regional keratometry and keratoscopy are clinical tests that enable the identification of very subtle clinical signs of keratoconus, thereby identifying FFK. However, sensitivity and specificity is far from optimal and complementary tests are needed. The diagnosis of FFK is critical when screening refractive surgery candidates, because such conditions are the most important risk factors for progressive “iatrogenic” ectasia that may occur after LASIK and Surface Ablation. About 1% of refractive candidates have ectasia detected during screening (keratoconus and pellucid marginal degeneration). The majority of such cases may present with normal BSCVA and unremarkable slit lamp biomicroscopy (Examples 1 and 2). Example 1: Forme-Fruste or Early (or better “mild”) Pellucid Marginal Corneal Degeneration (PMCD) 57 years old male, presented as a candidate for LASIK Stable refraction for 8 years; no family history of keratoconus UCVA was 20/400 in OD and counting fingers in OS Manifest refraction in O: −8.50 +2.50 × 013, giving 20/20; and in OS: −9.00 +2.00 × 173, giving 20/20. Ultrasonic corneal pachymetry measurements: 550 and 541 micron in OD and OS respectively. Regional inferior peripheral thickness were 518 and 522 micron in OD and OS respectively. Cornea examination by slit lamp demonstrated superficial punctuate keratitis in both eyes but no evidence of corneal thinning, iron lines, or protrusion. The patient was advised not to undergo LASIK or PRK and to return for a new exam within 6 months. If stability is documented, Custom Surface Ablation may be advocated with a detailed informed consent. (Ambrósio R Jr, Wilson SE. Cornea. 2002 Jan;21(1):114-7.) Figure 1 – Example 1: Corneal topography revealed inferior steepening with the pattern of a “lazy C” or lobster claw shape and an area of central corneal flattening. Age presentation and localized inferior thinning are favorable for the diagnosis of early pellucid corneal marginal degeneration. It has been suggested the term forme-fruste pellucid for describing such cases. However, this may be debatable if this is a variant of keratoconus. We believe that the complete differentiation between keratoconus and PMCD may be done only with elevation 3D cornel tomography and a comprehensive pachymetric evaluation over the entire cornea. Computerized corneal topography provided more sensitivity to detect keratoconus patterns in asymptomatic patients. The advent of progressive “iatrogenic” ectasia after LASIK and Surface Ablation despite of normal topography and without other identifiable risk factors lead to the understanding of the need for more sensitive diagnosis. Example 2: Asymmetric Forme-fruste Keratoconus (not unilateral) with normal curvature maps in the contra-lateral eye 23 years old male, presented as a candidate for LASIK No contact lens history; no family history of keratoconus Mild allergy; Positive for eye rubbing UCVA was 20/200 in OD and 20/80 in OS and BSCVA to 20/20 in OD and 20/15 in OS MRx: -2.75 -1.25 x 27 – OD and -1.00 -0.50 x 126 – OS Corneal Hysteresis (CH) and Corneal Resistance Factor (CRF) were 8.4 and 9.1 mmHg and 6.1 and 7.2 mmHg in OD and OS respectively with a low amplitude ORA signal in OU. CCT (US): 519 and 531 micron in OD and OS Slit Lamp is Normal in OU Figure 2 – Example 1: Placido’s axial curvature map revealing keratoconus pattern in OD and a normal pattern OS. Considering the patient is asymptomatic unless for myopic astigmatism, but with normal BSCVA, the right eye would be considered as a forme-fruste or mild keratoconus. Interestingly, the left eye has a remarkably normal topography. Cases like the left eye represent the best model to test if the enhanced screening tests are sensitive to detect any abnormality (see enhanced test results). There are also cases with topographic signs of keratoconus, such as inferior steepening which are stable with no progression over time. This may represent 0.5% of normal population (Example 3). Example 3: Asymmetric bow tie, stable for over 10 years 33 years old male; UCVA 20/15 OU MRx: +0.25 = -0.25 x 21 - OD and plano OS Corneal Hysteresis (CH) and Corneal Resistance Factor (CRF) were 11.8 and 10.6 mmHg and 11.2 and 10.1 mmHg in OD and OS respectively with a normal ORA signal in OU. CCT (US) is 502 and 505 micron in OD and OS Slit Lamp is Normal in OU Placido’s Topography is remarkably similar to the Pentacam’s Sagittal Anterior Map in OU with inferior steepening and asymmetric bow tie. Conclusion: Normal thin cornea (this case illustrates enhanced specificity). Figure 3: Axial curvature maps with IS /ABT, a keratoconic suspect pattern OD. USVA is 20/15 and there is also documented topographic stability over 10 years. Conreal surface disorders may also lead to an abnormal corneal topography similar to keratoconus. Example 4: False Positive Topography for Keratoconus due to irregular surface Figure 4: Placido’s Reflection and Corneal Topography Maps from a case with Anterior Basal Membrane Dystrophy. Figure 5: Biomicroscopy from a case with ABMD demonstrationg marked surface irregularity which leads to a keratoconic pattern on surface topogrpahy. This patient had custom surface ablation for treating hyperopic astigmatismo with excellent visual results and resolution of recurrent erosion. Other case of a false positive for FFK in corneal topography is contact lens corneal warpage, which is reversible, weeks to months after discontinuation of the contact lens. Some of these cases have documented successful LASIK with stable results. For example, Jampaulo and Maloney (J Refract Surg. 2008 Sep;24(7):707-9.) reported a patient with clinically evident topographic keratoconus with a preoperative spherical equivalent refraction of more than -10.00 diopters (D) who underwent successful LASIK with no evidence of progression of ectasia 7 years after surgery. We have done LASIK and now preferably Surface Ablation in similar cases based on the enhanced screening findings from Corneal Tomography (CTm) and biomechanical measurements (Example 5). Example 5: False Positive Topography for Keratoconus Suspect based on Corneal Tomography and Biomechanics. Patient had LASIK with stable results in both eyes for over 3 years. (This case would be considered as very high risk for ectasia based on corneal topography, age, thickness and high correction). 23 yo LASIK candidate, mild asymmetry on the axial topo MRx: - 9.50 -1.75 x 3º OD, giving 20/60 - 7.25 -1.25 x 179º OS, giving 20/20 No contact lens use US-CCT: 565 / 545 µm (OD / OS) Corneal Hysteresis (CH) and CRF were 12.1 and 12.0 mmHg and 13.1 and 12.2 mmHg in OD and OS respectively with a normal ORA signal in OU. Corneal Tomography revealed normal posterior elevation float and a normal thickness profile in OU. Patient had uneventful LASIK (Hansatome with intended flap thickness of 160 and VISX S4). 1 year Post Op UVCA: 20/50 (gain of 1 line from pre op BSCVA) in OD and 20/20 in OS. Results remain stable for over 3 years. Figure 6: Placido’s derived (Vista, iTrace) Curvature topography with ABT and IS in both eyes, which is a false postive for FFK based on enhanced screening methodology used. Highest K was 46.3 and 47.2 in OD and OS respectively; I/S difference at 6mm in diameter was 1.1 in OD and 1.5 in OS. Figure 7: Recent exam from OS by Scheimpflug Tomography by Oculyzer, demonstrating oblate cornea with stable architecture over 3 years after LASIK; UCVA: 20/20. Other alternative approaches have been described to provide more specificity to detect “real” ectasia, such as the evaluation of the epithelial profile using the very high frequency ultrasound tomography (Reinstein, Refractive Surgery SubDay 2007 and 2008). This is based on the previous study of the epithelial profile among normal corneas and on the observation that the epithelium thins over the protruded cone area as an attempt to mask the irregularities. Thereby a case with ABT and IS with a THICK epithelium over the cone would be considered as a FALSE POSITIVE on corneal topography, thereby a candidate for corneal refractive ablation. IV - The Concept of Ectasia Susceptibility Corneal thinning is a hallmark of these ectatic diseases. The area of maximal thinning, relative to the location of maximal corneal protrusion differentiates keratoconus, pellucid marginal degeneration, and keratoconus. Ectasia is a process of biomechanical failure, which is the biological equivalent of a well-known composite science process described in biomechanical engineering by Puk and Knops: interfiber fracture. Significant evidence supports that thinning does occur prior to steepening. A genetic predisposition, combined with behavioral (eye rubbing) and environmental stress factors influence the biomechanical susceptibility to develop ectasia. Thereby, a concept of a balance between corneal resistance (individual genetic-driven corneal biomechanical and biochemical properties) and stress factors (individual phenotype) would lead to a net result which we refer as ECTASIA SUSCEPTIBILITY. More sensitive analyses reveal a continuum of findings from normal cornea towards ectatic disease, even in its earliest presentations. For example, this is well documented that some family members of keratoconus patients have mild topography abnormalities. Studies from asymmetric keratoconus and examples indicate that novel tests based on corneal tomography and biomechanical measurements are sensitive to detect abnormalities in the contralateral eyes with normal topography (Salomão, ASCRS 2008). We believe that any cornea may undergo ectasia IF enough stress is applied to overpass its resistance limit, leading to biomechanical failure. For example, some corneas may undergo spontaneous ectasia (keratoconus) even without eye rubbing history. Others cases may undergo ectasia IF there is enough stress, such as eye rubbing and corneal surgery to overcome corneal resistance limit. V - Enhanced Screening Corneal Tomography Along with anterior curvature data, CTm provides detailed architecture information so that elevation maps from the front and back surfaces are calculated, along with the paquimetric map. Much attention has been devoted to the posterior corneal elevation map. The BFS (best fit sphere) for the 9mm corneal area is one of the most accepted parameters for referencing the elevation map. The thickness map provide detailed information regarding the thinnest point (value and location in relation to the apex [0;0]) nad pachymetric distribution. Corneal Thickness Spatial Profile (CTSP): average of the thickness values along twenty-two imaginary circles centered on the thinnest point (TP). Percentage Thickness Increase (PTI): percentage of increase of each of these circles from the TP. CTSP and PRI Graphs displays 95%CI limits of normals. Thinned corneas (likely ectatic) have profiles out of the 95% CI more abrupt (going down) increase. Normal Thin Cornea CCT = 493 µm Figure 8: CTSP and PTI Graphs for the thickness profiles. Example from a normal thin cornea. Anterior and Posterior Enhanced Elevation: standard BFS “subtracted” from the enhanced BFS (best fits to peripheral cornea excluding 4mm in diameter centered on the thinnest). Figure 9: Belin’s Concept for Enhanced Elevation. Peripheral fit highlights the cone area. Figure 10: Normal Enhanced Elevation in a thin cornea. Enhanced Elevation Map (Three colors Format): Anterior: Green < 6, Yellow: 6 – 12, Red > 12 µm Posterior: Green < 8, Yellow: 8 – 20, Red > 20 µm Corneas with higher elevation around the TP (likely ectatic) have pronounced differences between the standard and enhanced BFS (YELLOW and RED). The Pentacam Belin-Ambrósio Enhanced Ectasia Display (BAD) combines thickness profile with enhanced elevation from front and back. VI - Enhanced Screening and Corneal Biomechanics: ORA (Ocular Response Analyzer) A ORA Signal 2 1 B 4 3 Figure 11: A - ORA Measurement and B – ORA Normal Signal Corneal response to a collimetric air pulse is monitored by the infrared light reflection (applanation => peak) Detects two applanation events correlated with the air pulse pressure (INWARD - p1 and OUTWARD - p2) The delay of p2 caused by corneal viscous damping [CH = p1 – p2] and [CRF = p1 - (K * p2)] Normal Values: CH: 10.17 ± 1.82 mmHg (3.23 to 14.58) CRF: 10.14 ± 1.8 mmHg (range 5.45 to 15.1) Ectasia leads to lower CH and CRF and altered signals CH or CRF < 8.8mmHg is considered a relative contra indication for LASIK based on normal population values Advanced Bio-corneagram Analysis provides 38 waveform morphology parameter. Combination these new parameters can provide new information regarding corneal behavior, allowing a better biomechanical study. VII - Corneal Biomechanics with the Corvis ST (Oculus, Germany) Ultra High-Speed (UHS ST) Scheimpflug Technology: 4,330 frames/sec that monitors 8mm horizontal Scheimpflug image in response to a symmetrically metered air pulse with fixed peak pressure. The metered collimated air pulse or puff has a symmetrical configuration and fixed maximal internal pump pressure of 25 kPa. The bidirectional movement of the cornea in response to the air puff is monitored. Measurement time is 30ms, with 140 frames acquired. Advanced algorithms for edge detection of the front and back corneal contours are applied for every frame. IOP is calculated based on the first applanation momentum. Deformation amplitude is determined as the highest displacement of the apex in the highest concavity momentum. Applanation length and corneal velocity are recorded during ingoing and outgoing phases. Such parameters provide clinical in vivo characterization of corneal biomechanical properties, which are relevant for different applications in Ophthalmology. Figure 12: Corvis ST and corneal Scheimpflug imaging in response to a symmetrically metered air pulse with fixed peak pressure VIII - Integration of tomographic and biomechanical evaluation in clinical practice Enhanced Screening Findings from Asymmetric Forme-fruste Keratoconus (not unilateral) with normal curvature maps in the contra-lateral eye Sagittal Anterior Curvature Map from Pentacam Scheimplfug CTm with similar findings as in Placido’s Topography Abnormal profile in both eyes. Note the escape from the superior limit (lower dot line) in the PTI in both eyes. ORA Signal with relatively low amplitudes and waveform scores in both eyes. The findings in OS are abnormal and, despite the normal anterior curvature map, this case is considered as a high risk for ectasia (Ectasia Susceptible). Conclusions A. Curvature -based Corneal Topography is a more traditional and intuitive language for Ophthalmologists and will always be critical since it reflects refractive power of the cornea and optical regularity. It is (and will always be) a critical step for the evaluation of refractive properties of the cornea and quality of the ocular surface tear film. B. However, curvature maps does not represent all the picture for screening candidates for Refractive Surgery. C. Central Corneal Thickness (CCT) of Pachymetry does not represent the thinnest value. D. Corneal Tomography is defined as a 3D representation of the corneal architecture, with detailed and reliable data from the front and back surface of the cornea and a pachymetric map. E. Elevation subtraction maps is the preferred method for describing the front and back surfaces of the cornea. However, this is a more complex way and less intuitive for the general Ophthalmologist. In addition, there are many possible options to calculate the reference surface for the subtraction with the corneal surface (front or back). F. Corneal Thickness Distribution enables the identification of ectasia and the differentiation of a normal thin cornea from ectasia. G. The Belin-Ambrósio Enhaced Ectasia Display (BAD) combines tomographic elevation from anterior and posterior corneal data, along with a more comprehensive thickness evaluation, which provide complementary critical additional information for screening refractive candidates. H. Corneal Biomechanical measurements represent a complementary method for the enhanced screening for ectasia References: 1. Binder PS, Lindstrom RL, Stulting RD et al. Keratoconus and corneal ectasia after LASIK. J Refract Surg 2005; 21: 749–52. 2. Wing M, ed. Corneal Topography in the Wavefront Era: A Guide for Clinical Application. New Jersey: Slack Publishing, 2006. 3. Littoff D, Belin MW, Winn SS, Smith RS: PAR Technology Corneal Topography System. Inv Ophthalmol. Vis Sci 1991;32: 992. 4. Ciolino J, Belin MW: Changes to the Posterior Cornea after LASIK and PRK. J Cataract & Refract Surg 2006; 32: 1426-31. 5. Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28: 293–322. 6. Moshirfar M, Marx DP. Incidence of Post-LASIK Ectasia in Patients with Unidentified Preoperative Risk actors. Presented World Cornea Congress, Washington, DC, 2005. 7. Klein SR, Epstein RJ, Randleman JB, Stulting RD. Corneal ectasia after laser in situ keratomileusis in patients without apparent preoperative risk factors. Cornea 2006; 25: 388–403. 8. Belin MW, Khachikian SS: New Devices & Clinical Implications for Measuring Corneal Thickness. Clin & Exp Ophthalmol 2006; 34: 729-731. 9. Klyce SD, Karon MD, Smolek MK. Screening patients with the corneal navigator. J Refract Surg. 2005;21:S617-22. 10. Ambrósio Jr R, Klyce SD, Smolek MK, Wilson SE. Pellucid marginal corneal degeneration. J Refract Surg. 2002;18:86-8. 11. Amoils SP, Deist MB, Gous P, Amoils PM. Iatrogenic keratectasia after laser in situ keratomileusis for less than -4.0 to -7.0 diopters of myopia. J Cataract Refract Surg. 2000;26:967-77 12. Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110:267-75. 13. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008 Jan;115(1):37-50. Epub 2007 Jul 12. 14. Condon PI. 2005 ESCRS Ridley Medal Lecture: will keratectasia be a major complication for LASIK in the long term? J Cataract Refract Surg. 2006 Dec;32(12):2124-32. 15. Binder PS. Ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2003;29:2419-29. 16. Jonsson M, Behndig A. Pachymetric evaluation prior to laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:701-6. 17. Mandell RB, Polse KA. Keratoconus: spatial variation of corneal thickness as a diagnostic test. Arch Ophthalmol. 1969;82:182-188. 18. Luz A, Ursulino M, Ambrósio Jr R. Corneal Thickness Variation from the Thinnest Point to the limbus: Study based in a normal and keratoconus population for creating reference values. Arch Bras Oftalmol. In Press 2006. 19. Ambrósio Jr R, Jardim D. Corneal Biomechanics, Pachymetry Progression, and Volume: Novel Indices for Detecting Ectasia and Screening Refractive Patients. ASCRS 2006 Online Poster - awarded as Best Poster Category: Cornea. http://ascrs2006.abstractsnet.com/acover.wcs?entryid=076028 (accessed on april2008) 20. Ambrósio Jr R. Corneal Biomechanics, Pachymetric Progression Profile, and Corneal Volume: Indices for Detecting Ectasia and Screening Refractive Candidates . ASCRS 2007 Online Poster - Honorable Mention Category: Refractive. http://ascrs2007.abstractsnet.com/acover.wcs?entryid=000242 (accessed on april-2008) 21. Huang D. A reliable corneal tomography system is still needed. Ophthalmology. 2003 Mar;110(3):455-6. 22. Wickham L, Edmunds B, Murdoch IE. Central corneal thickness: will one measurement suffice? Ophthalmology. 2005 Feb;112(2):225-8 23. Ambrósio R Jr, Alonso RS, Luz A, Coca Velarde LG. Corneal-thickness spatial profile and corneal-volume distribution: tomographic indices to detect keratoconus. J Cataract Refract Surg. 2006 Nov;32(11):1851-9. 24. Auffarth GU, Wang L, Volcker HE. Keratoconus evaluation using the Orbscan Topography System. J Cataract Refract Surg. 2000;26:222-8. 25. Rao SN, Raviv T, Majmudar PA, Epstein RJ. Role of Orbscan II in screening keratoconus suspects before refractive corneal surgery. Ophthalmology. 2002;109:1642-6. 26. Cairns G, McGhee CN. Orbscan computerized topography: attributes, applications, and limitations. J Cataract Refract Surg. 2005;31:205-20. 27. Ambrósio Jr R. Enhanced Screening for Refractive Candidates Based on Corneal Tomography and Biomechanics. ASCRS 2008 Online Poster - awarded as Best Poster Category: Cornea. http://ascrs2008.abstractsnet.com/acover.wcs?entryid=000116 (accessed on april2008) 28. Li X, Rabinowitz YS, Rasheed K, Yang H. Longitudinal study of the normal eyes in unilateral keratoconus patients. Ophthalmology. 2004 Mar;111(3):440-6.