BCS Accreditation Element List
advertisement

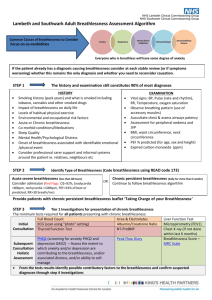
BCS Accreditation – Elements list 1. Service Planning Service requirement 1.1 Public Health. 1.2 Local delivery plans. 1.3 National policy (NSF etc). 1.4 Develop and review policies, strategies and plans for CHD services. 1.5 Review and enhance the strategic position of the PCT in relation to cardiovascular services. 1.6 Reduce the risk of people experiencing CHD. 1.7 Needs assessment. 1.8 Ensuring equity. Learning outcomes Understand how to assess the health needs of local populations and the interventions that could favourably impact on them. Be able to provide this data in a form that enables commissioners to determine the best use of resources. Know how to collate and present service plans to commissioners and national bodies in an effective way. Have an understanding of national targets, standards and audit points and how national policy can be translated into local action. Know how to ensure that local plans are consistent both with national policy and with local needs. Work with the PCT in delivering the joint vision for cardiovascular services. Understand the factors contributing to risk of CHD, and how to prevent it. Use this to develop local policy. Know how to assess the healthcare needs of the local population in order to develop appropriate cost-effective policies. Know how to assess equity and develop plans to improve the equitable provision of care. 2. Service development and delivery Service requirement 2.1. Financial planning. 2.2. Expert advice across PCT on developing cardiac services. 2.3. Service improvement and workforce development. 2.4. Act as an interface between primary, secondary and tertiary care. Learning outcomes Broadly estimate the cost of existing and planned services. Make the best use of available resources. Contribute clinical understanding to the development of cardiology services. Understand service improvement methodologies, and how to tailor the workforce to the tasks necessary to satisfy the service requirements. Understand the importance of designing services around the patient by working across traditional service boundaries. 3. Commissioning Service requirement 3.1. Work with commissioners, PCT leads and local secondary care representatives to develop local CHD services. 3.2. Links to PEC and cardiac network. Learning outcomes Work across organisations to develop seamless local services Work with the PEC and the cardiac network to ensure consistency of approach. 4. Education Service requirement 4.1. Educating GPs / PwSIs. 4.2. Mentor staff developing CHD skills. 4.3. Development of training programmes (in-house / external). Page 1 of 4 Learning outcomes Know how to assist in the educational development of local GP’s and other PwSI. Know how to assist and mentor GP’s and other PwSI towards their educational goals. Understand how to design and deliver local educational programmes. 5. Audit and clinical governance Service requirement 5.1. Lead the cardiovascular quality assurance programme in primary care including: Clinical governance process; Clinical standards. 5.2. Ensure the appropriateness of the various working environments and monitor and report on cleanliness. 5.3. Develop audit and IT processes to appraise services and inform service improvement. 5.4. Physical resources. Learning outcomes Understand how to assess the quality of cardiovascular services, and how to involve other staff in driving up standards. Understand the design and maintenance issues around the environments in which cardiovascular services are delivered. Understand clinical audit and the various audit systems in use for cardiovascular services. Know how to set up and evaluate an audit programme. Know the health and safety requirements relating to the environments in which cardiovascular services are delivered. 6. Presenting symptoms - breathlessness Service requirement 6.1. Assessment of the breathless patient. 6.2. Understanding relevant tests (ECG, echo, BNP, CxR). 6.3. Performing echo for heart failure. 6.4. Performing comprehensive echo. 6.5. Diagnosis. 6.6. Initiation and up-titration of medication. 6.7. Understanding of the role of device therapy. 6.8. Chronic disease management. 6.9. Lifestyle advice risk factor management and patient self management 6.10. Any clinician providing enhanced services to breathless patients. Learning outcomes Having a detailed understanding of the pathophysiology and investigation of conditions causing breathlessness, including non-cardiac causes. Knowing the strengths and weaknesses of investigations used to confirm or refute the diagnosis of heart failure. Certification from BSE accredited department for screening echo to exclude systolic LV dysfunction. BSE accreditation in community echo cardiography. Be able to assimilate the results of history, examination and investigations to be able to diagnose the cause of breathlessness, or to be able to diagnose or rule out heart failure or other cardiac causes of breathlessness. Knowledge of the recommended pharmacological agents for heart failure, their actions, indications, side-effects and use in combination. Knowledge of the contribution that device therapy and which patients might benefit. Ensuring that all relevant evidence based therapies are offered and used optimally. Carrying out regular reviews. Be able to give advice, about lifestyle issues relevant to the underlying condition, and support the patient in managing their own condition. A general understanding of the pathophysiology, symptomatology, investigation and treatment of heart failure. 7. Presenting symptoms - chest pain Service requirement 7.1. Assessment of the patient with chest pain. 7.2. Understanding relevant tests (stress ECG, stress echo, Myocardial Perfusion Imaging, Coronary angiography). 7.3. Performing stress echo. 7.4. Diagnosis. 7.5. Initiation of medication. Page 2 of 4 Learning outcomes Knowledge of the pathophysiology, clinical characteristics and investigations for all common causes of chest pain, including non-cardiac. Knowing the strengths and weaknesses of tests used to evaluate the causes of chest pain. BSE adult certification and further training specifically in stress echocardiography. Assess the results of tests to produce a differential diagnosis, or to rule out myocardial ischaemia Understanding the indications for treatments for ischaemic heart disease, and the pharmacology and side-effects of the various medications. Service requirement 7.6. Chronic disease management. 7.7. Lifestyle advice, risk factor management. 7.8. Any clinician providing enhanced services to patients with chest pain. Learning outcomes Understanding the indications for invasive investigations for coronary disease, and the medical management, including all evidence-based treatments. Understanding of the value of risk factor management, including non-pharmacological interventions and rehabilitation. A general understanding of the pathophysiology, symptomatology, investigations and treatment of ischaemic heart disease. 8. Presenting symptoms - palpitation Service requirement 8.1. Assessment of the patient with palpitations. 8.2. Understanding relevant tests (ECG, Holter, Reveal, Echo). 8.3. Performing relevant tests. 8.4. Diagnosis. 8.5. Management, inc indications for anticoagulation and antiarrhythmic drugs and the role of ablation. 8.6. DC Cardioversion. 8.7. Any clinician providing enhanced services to patients with palpitations. Learning outcomes Understand the causes of palpitations and the value of the history and examination in assessment. Knowing the place for and value of the available tests for palpitations. Being able to carry out ECG, Holter, long-term ECG recording. Assimilate the results of tests together with clinical evaluation to produce a diagnosis. Know and institute the appropriate management for the diagnosed cause of palpitations. Be able to carry out DC cardioversion safely. A general understanding of the causes and mechanisms of palpitations as well as the investigations and treatments available. 9. Presenting symptoms - blackouts and dizzy spells Service requirement 9.1. Assessment of the patient with blackouts or dizzy spells. 9.2. Understanding and interpreting the relevant tests. 9.3. Diagnosis. 9.4. Understanding the indications for permanent pacemaker implantation. 9.5. Any clinician providing enhanced services to patients with blackouts and dizzy spells. Learning outcomes Understanding the causes of blackouts and dizzy spells including non-cardiac (eg neurological) causes. Initiating appropriate tests. Understanding the strengths and weaknesses of ECG, Holter, Reveal, Echo and Tilt testing. Assimilate the results of clinical features and investigations to arrive at a cause for blackouts, or to rule out a cardiac cause. Understanding which patients should be referred for permanent pacemaker implantation, ICD or other device. A general understanding of the causes and mechanisms of blackouts and dizzy spells, as well as the investigations and treatments available. 10. Hypertension Service requirement 10.1. Assessment of new cases. 10.2. Investigation of complex cases. 10.3. Treatment. 10.4. Any clinician providing enhanced services to patients with hypertension. Page 3 of 4 Learning outcomes Understanding of the definition of and means of diagnosing hypertension. Understanding when to institute investigations for secondary hypertension, the tests required and the importance of the results. Understanding of the pharmacological and nonpharmacological treatments for hypertension, and their roles in different situations. Side-effects of drugs. Titration of drugs to optimal effect. A general understanding of the definition of hypertension, its causes and treatment. 11. Palliation Service requirement 11.1. Delivery of a service to provide palliative or supportive care to cardiac patients with terminal conditions such as heart failure. Learning outcomes Understand the medical and psychosocial methods of palliation and preparation of the patient and carers for death. 12. Primary prevention Service requirement 12.1. Risk assessment. 12.2. Management of risk factors. Learning outcomes Know the contributions of risk factors and how to calculate risk of CHD. Be able to advise patients about lifestyle modification. Know when drug therapy is indicated, and the potential side-effects of medication. 13. Secondary prevention Service requirement 13.1. Chronic disease management. Learning outcomes Understand the potential for modification of risk factors both by lifestyle changes and medication. 14. Cardiac rehabilitation Service requirement 14.1. Run exercise classes. 14.2. Assess patients’ suitability for exercise. 14.3. Provide dietary advice. 14.4. Provide information about medication. Learning outcomes Phase 3 - physiotherapist or exercise specialist. Phase 4 BACR qualification recommended. Advise patients about appropriate safe exercise programmes for carrying out either in classes or at home. Provide patients and carers with broad dietary advice appropriate to their requirements. Assist patients with understanding their medication and encourage compliance. See: Secondary prevention. 15. Promotion of patient/carer self-management Service requirement 15.1. Chronic disease self-management. Learning outcomes Be able to educate patients about their condition and instruct them in making appropriate observations and management decisions. 16. Managing personal performance Service requirement 16.1 CPD. Page 4 of 4 Learning outcomes Know how to keep up to date in the chosen field, and requirements for revalidation.