File
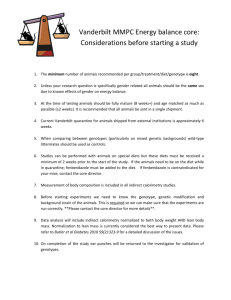
advertisement

Chapter 32 Diet Therapy and Special Diets Nutrition Nutrition is a vital component of therapy for many disorders. Some disorders necessitate a special diet, either during acute illness or throughout life. People who are ill may need help fulfilling their nutritional requirements. Mealtime is an excellent time to introduce or to reinforce diet teaching. Providing Nutritional Support to a Client Present food in an attractive and appetizing manner. Check the tray for the correct diet and check the client’s identification to ensure that the food is going to the right client. Monitor and teach good dietary habits. Make observations related to consumption of food and the client’s ability to prepare and eat food. Provide educational support about nutritional needs. Note clients who can have nothing by mouth (NPO). Meal Supplements Between-meal and bedtime supplements are often given to clients who have high nutritional needs or poor appetites. It may be ordered by physicians or initiated by dietitians. It must be served on time. If given too early, the client may still feel full from the previous meal. If given too late, it may ruin the client’s appetite for the next meal. Document nourishment intake or refusal by the client. Fluid Intake Fluid is required to maintain homeostasis; too much plain water can lead to electrolyte imbalance. Fluids include all foods and beverages that are in fluid form at room temperature. Force fluid Promote increased fluid intake Fluid restriction Polydipsia or end-stage renal disease Monitor client for intake and output (I&O). Assistance With Eating Very young, helpless, or confused individuals Visually impaired or temporarily blinded following surgery Individuals who have trouble chewing Clients with dysphagia or swallowing disorder Document Poor appetite, food refusal, swallowing difficulty, or complains of nausea Fluid intake, caloric intake, or the amount of tube feeding taken House Diets House diet Normal diet in acute or extended care facilities Regular diet, general diet, or full diet Served to clients who do not require a special diet Select diet or client’s select diet Diet as tolerated (DAT) Depends on client’s appetite and ability to eat and to tolerate food Modified Diets Modified diet Important part of therapy for many diseases. The physician and dietitian consider the disease process and the client’s general condition. Therapeutic diet Prescribed as part of the treatment of more than one disease or condition Question Is the following statement true or false? A diabetic client is more likely to comply with diet restrictions if it is referred to as “controlledcarbohydrate” diet rather than “diabetic diet.” Answer True Clients are more likely to comply with diet restrictions if they are not constantly reminded of their disease by having the diet classified according to a disease name. Referring to a diabetic diet as a “controlled-carbohydrate” diet de-emphasizes diabetes and focuses attention on nutritional habits the client should develop. Modified Diets The following classifications indicate how diets are modified in treatment: Consistency and texture (liquid, soft, mechanical, high-fiber, low-fiber) Energy value (high- or low-calorie) Nutrients (controlled carbohydrate, high- or low-fat or protein, sodium, calcium, phosphorus or potassium controlled) Amount (e.g., six small feedings) Specific allergens (e.g., eggs, dairy, nuts) Consistency Modifications Liquid diets Clear liquid diet Short-term, requires minimal digestion, leaves minimum residue, provides some electrolytes and carbohydrates Full liquid diet Suitable for long-term use, used to approximate the nutritional value of a diet, may be inadequate in folic acid, iron, vitamin B6, fiber Consistency Modifications (cont’d) Soft diet Digestive soft diet Nutritionally adequate diet; low in fiber, connective tissue, and fat; gas-forming foods are eliminated and mild seasonings are used Mechanical soft diet or dental soft diet Nutritionally adequate; meats, fruits, and vegetables may be chopped, ground, or pureed Consistency Modifications (cont’d) High-fiber diet Increased amount of insoluble fiber that helps increase stool bulk and stimulates peristalsis Increased amount of soluble fiber that helps lower the serum cholesterol level and improves glucose tolerance in diabetes Potential problems are cramping, diarrhea, and gas. Consistency Modifications (cont’d) Low-fiber or low-residue diet Foods that the body can absorb completely so that little residue is left for the formation of feces May be inadequate in iron, calcium, and some vitamins and minerals because of limited food choices and overprocessing of fruits and vegetables Bland diet Limit foods that stimulate the production of gastric acid Energy Value Modifications High-calorie diet Used in cases of weight loss, hyperthyroidism, undernutrition, general malnutrition, severe burns Clients with a depressed appetite may need smaller and more frequent meals. Low-calorie diet Promotes weight loss in those with, or at risk for, complications related to obesity Nutrient Modifications Carbohydrate-controlled diets Diabetic diet Eat foods in their natural form to increase fiber intake. Lactose-restricted diet People with lactose intolerance lack sufficient amounts of the enzyme lactase, which is needed to digest the sugar (lactose) in dairy products. Nutrient Modifications (cont’d) Fat-controlled diets First step in treating individuals with hyperlipidemia Low-fat diet Prescribed for clients with malabsorption syndromes, pancreatic, and gallbladder diseases High-fat diet Prescribed for children with seizure disorders. This ketogenic diet is extremely low in carbohydrates and is sometimes as high as 80% to 90% fat. High-protein diet Encompasses a range of protein intakes depending on the severity of depletion and causative factors Protein-restricted diet The amount of protein is based on the client’s weight or may be ordered as a total amount per day. Nonprotein calorie intake should be high. Gluten-restricted diet Prescribed for clients with celiac disease Nutrient Modifications (cont’d) Diets with controlled minerals and electrolytes Sodium-controlled diets Depends on the client’s disease and the amount of edema present Mild sodium restriction Moderate sodium restriction Strict and severe sodium restriction Nutrient Modifications (cont’d) Diets with controlled minerals and electrolytes Calcium- or phosphorus-modified diets High calcium intake is indicated for both the prevention and treatment of osteoporosis. Low phosphorus diet may be indicated for the person with kidney failure. Potassium-modified diet For clients who are taking diuretics Question Is the following statement true or false? The progression of a client’s diet should always start with a clear liquid diet, then full liquid diet, followed by a soft diet, and finally, a regular diet. Answer True The progression of diets should be: clear liquid, full liquid, soft, and regular. A client’s diet should progress as soon as possible to ensure an adequate nutritional intake and to increase the client’s sense of well-being. Diets Modified for Allergens An allergic reaction is caused by an autoimmune response to specific proteins called allergens in certain foods. Depending on the number of allergens and how widespread they are in the diet, vitamin and mineral supplements may be necessary to ensure a nutritionally adequate intake. Tube Feedings A tube feeding or enteral feeding Provides liquid nourishment through a tube into the gastrointestinal (GI) tract Liquid formulas Routine formulas Specialized formulas Ready-mixed formulas Powdered formulas Tube Feedings (cont’d) Placement sites Nasogastric tube (NG tube) Passed through the nose and into the stomach Gastrostomy tube (G tube) Placed directly into the stomach through the abdominal wall A jejunal tube (J tube) Inserted into the jejunum of the small intestine Question Is the following statement true or false? The bed should be put flat when the client is receiving a tube feeding. Answer False The head of the bed must be elevated about 30 degrees whenever a client is receiving a tube feeding. If the bed is put flat, even for a short period of time, such as for changing bed linens, the client has a chance of aspirating stomach contents. Serious complications, such as aspiration pneumonia, may lead to client morbidity or mortality. Types of Tubes Nasogastric: Through the nose into the stomach Percutaneous: Percutaneous endoscopic gastrostomy (PEG) placed through the skin Endoscopic: Placed with an instrument called an endoscope Gastrostomy: Inserted into the stomach Button feeding device: A small silicone device used in place of a gastrostomy tube Nursing Considerations The nurse is responsible for washing or replacing the feeding bag, as per hospital policy, and documenting care. The client may need an extra water (“free water”) allowance. Document findings and alert the physician if untoward signs develop: Dry mouth, poor skin turgor (tone), complaints of thirst, illness, fever or physical complaints. Question Is the following statement true or false? The nurse should inform the team leader or physician if a client is NPO for more than 3 days. Answer True The prolonged use of nothing by mouth (NPO) is a serious problem. A client may be NPO for tests, after surgery, or because of vomiting. A client who has been NPO for 3 or more days and is not receiving nutritional support is at serious nutritional risk. Intravenous Therapy Intravenous (IV) therapy or parenteral therapy Involves injecting into a vein sterile solutions, drugs, and electrolytes that the body needs Total parenteral nutrition (TPN) Infused directly into the blood circulation and bypasses the digestive tract Peripheral parenteral nutrition (PPN) Contains lesser concentrations of TPN, administered into a peripheral vein End of Presentation