Module 6 - Arthroplasty
advertisement

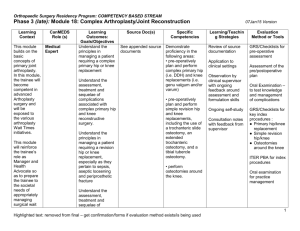
Orthopaedic Surgery Residency Program: COMPETENCY BASED STREAM MODULE 6: ARTHROPLASTY Dr. John Murnaghan Learning CanMEDs Learning Outcomes: Source Specific Context Role (s) Goals/Objectives Doc(s) Competencies Medical The goal of KNOW: Campbell’s DO: this module will Expert (Knee) Be able to advise Arthroplasty Perform an be for the patients regarding the Chp 6 appropriate trainee to non-operative work up diagnose and management of knee Source (including treat patients arthritis; including documents history, with hip or indications, on Portal physical knee arthritis complications and examination, and be able to effectiveness of such and diagnostic perform a total treatment imaging) for knee and total patients with hip knee arthritis arthroplasty and organize with guidance an appropriate and/or non-operative supervision. plan, when indicated Residents will spend approximately 4 weeks on a Medical Be able to explain the Campbell’s DO: Be able to block Expert (Knee) indications, results Arthroplasty explain the dedicated to and complications of Chp 6 indications, the knee at surgery for knee results and the Holland arthritis with respect Source complications Centre with to age, gender and documents of surgery for Dr. J. activity level. on Portal knee arthritis Murnaghan with respect to and age, gender approximately and activity 4 weeks on a level. block dedicated to the hip with Dr. O. Safir at Mount Sinai 20Jan15 Version Learning/Teaching Strategies Review of source documentation Resident observation of staff surgeon performing all of the specific competencies, with the opportunity for questions and discussion afterwards Resident opportunity to perform assessments under supervision of supervisor Review of source documentation Resident observation of staff surgeon performing all of the specific competencies, with the opportunity for questions and discussion afterwards Resident opportunity to perform assessments under supervision of supervisor Evaluation Method or Tools Assessment of performance on these competencies will be a continuous process over the course of the rotation with both summative and formative feedback coming from supervising surgeons and allied health professionals Observed clinical history and physical to give real-time assessment of clinical skills (one per month) with global ratings (last week of module) Mid-module assessment will occur where resident will be given an oral examination, short-answer questions, and a STACER on either a primary total hip or knee arthroplasty. A summative and formative evaluation will then follow Hx PE exam (oral) form End-of-module assessment will occur where resident will be given an oral examination, short-answer questions, and a STACER on either a primary total hip or knee arthroplasty. A summative and formative evaluation will then follow 1 Learning Context CanMEDs Role (s) Medical Expert (Knee) Learning Outcomes: Goals/Objectives Be able to explain the principles of knee reconstructive surgery for arthritis including osteotomy, arthrodesis and joint replacement Source Doc(s) Campbell’s Arthroplasty Chp 6 Source documents on Portal Specific Competencies Learning/Teaching Strategies DO: Be able to explain the principles of knee reconstructive surgery for arthritis including, osteotomy, arthrodesis and joint replacement One day surgical skills session on cadavers reviewing approaches, and techniques for total knee arthroplasty DO: Carry out the pre-operative planning for primary knee arthroplasty, with guidance DO: Perform arthrotomy and primary total joint replacement of the knee (and osteotomy and arthrodesis if opportunity arises) Medical Expert (Knee) Demonstrate an understanding of the recovery and rehabilitation following knee replacement Campbell’s Arthroplasty Chp 6 Source DO: Manage postoperative care and Evaluation Method or Tools Observed assessment throughout module on teaching rounds An ITER will be filled out at the end of the module at time of exit interview Review of source documentation Resident observation of staff surgeon performing all of the specific competencies, with the opportunity for questions and discussion afterwards Resident opportunity to perform assessments under supervision of supervisor Review of source documentation Resident observation of staff surgeon 2 Learning Context CanMEDs Role (s) Learning Outcomes: Goals/Objectives Source Doc(s) documents on Portal Specific Competencies common complications following knee arthroplasty Learning/Teaching Strategies performing all of the specific competencies, with the opportunity for questions and discussion afterwards Evaluation Method or Tools Resident opportunity to perform assessments under supervision of supervisor Medical Expert (Hip) Medical Expert (Hip) Be able to advise patients regarding the non-operative management of hip arthritis including indications, complications and effectiveness of such treatment Demonstrate an understanding of the indications, results and complications of surgery for hip arthritis with respect to age, gender and activity level. Campbell’s Arthroplasty Chp 7 Source documents on Portal Campbell’s Arthroplasty Chp 7 Source documents on Portal DO: Perform appropriate work up (including history, physical examination, and diagnostic imaging) for patients with hip arthritis and organize an appropriate non-operative plan, when indicated Review of source documentation DO: Demonstrate an understanding of the indications, results and complications of surgery for Review of source documentation Resident observation of staff surgeon performing all of the specific competencies, with the opportunity for questions and discussion afterwards Resident opportunity to perform assessments under supervision of supervisor Resident observation of staff surgeon performing all of the specific competencies, with the opportunity for 3 Learning Context CanMEDs Role (s) Medical Expert (Hip) Learning Outcomes: Goals/Objectives Able to explain the principles of reconstructive hip surgery for arthritis including osteotomy, arthrodesis and joint replacement Source Doc(s) Campbell’s Arthroplasty Ch’s 7 Source documents on Portal Specific Competencies hip arthritis with respect to age, gender and activity level. Learning/Teaching Strategies questions and discussion afterwards DO: Able to explain the principles of hip reconstructive surgery for arthritis, including osteotomy, arthrodesis and joint replacement One day surgical skills session on cadavers reviewing approaches, and techniques for total hip arthroplasty DO: Carry out preoperative planning for primary hip arthroplasty, with guidance DO: Perform arthrotomy and primary total joint replacement of the hip (and osteotomy and arthrodesis if opportunity Evaluation Method or Tools Resident opportunity to perform assessments under supervision of supervisor Review of source documentation Resident observation of staff surgeon performing all of the specific competencies, with the opportunity for questions and discussion afterwards Resident opportunity to perform assessments under supervision of supervisor 4 Learning Context CanMEDs Role (s) Learning Outcomes: Goals/Objectives Medical Expert (Hip) Demonstrate an understanding of the recovery and rehabilitation following hip replacement Source Doc(s) Campbell’s Arthroplasty Ch’s 7 Source documents on Portal Specific Competencies arises) DO: Manage postoperative care and common complications following hip arthroplasty Learning/Teaching Strategies Evaluation Method or Tools Review of source documentation Resident observation of staff surgeon performing all of the specific competencies, with the opportunity for questions and discussion afterwards Resident opportunity to perform assessments under supervision of supervisor Medical Expert Communicator Demonstrate an understanding of the unique medical problems of the geriatric population KNOW: Provide appropriate information to others involved in the care of the patient Listen effectively and obtain an appropriate history from patients and their families and Campbell’s Arthroplasty Chp 6 + 7 Source documents on Portal Manage perioperative issues in the geriatric population, with regards to total joint arthroplasty Perform live surgical timeout effectively to display appropriate communication Regular observation time with supervising, with opportunity to discuss diagnosis and evidence-based treatments Review of source documentation Resident will do live time out with feedback from the surgical team in the OR Real-time assessments of ability to perform surgical time out to occur when resident in operating room Summative assessment at end of module – as reflected in ITER 5 Learning Context CanMEDs Role (s) Learning Outcomes: Goals/Objectives gather information not only about the specific problem but also about the patient’s beliefs, expectations and concerns about their illness. Source Doc(s) Specific Competencies Learning/Teaching Strategies Evaluation Method or Tools Provide information to the patient in a humane manner with language that they can understand so that they may be involved in the decision making process regarding their care. Manager Obtain an appropriate informed consent for patients undergoing interventions. KNOW: Demonstrate an understanding of the importance of the allocation of health care resources and how that effects wait list management Apply evidence and management processes for costappropriate care Triage of patients on elective surgical list requiring hip and knee arthroplasty (as per priority level) Direct feedback from supervisor on assessment of case booking Assessment of triaging cases (form) Resident to spend half days (2) in advanced practice physiotherapist clinic at Holland Centre to understand triage process of newlyreferred patients (for hip and knee arthritis). Manager encounter form OSCE or MCQ Direct feedback and opportunity for 6 Learning Context CanMEDs Role (s) Learning Outcomes: Goals/Objectives Source Doc(s) Specific Competencies Learning/Teaching Strategies questions and answers from supervising physio and clinic manager Evaluation Method or Tools Reference textbooks: Campbells Operative Orthopaedics, 10th edition, chapter 6 Surgery of the Knee, 4th Edition, Norman Scott Editor. AAOS Orthopaedic Basic Science Text book Optional Readings and/or Required – Resident to be notified: Wear and Osteolysis Around Total Knee Arthroplasty. J. Am. Acad. Ortho. Surg., January 2007; 15: 53 - 64. Hannah Morgan, Vincent Battista, and Seth S. Leopold. Constraint in Primary Total Knee Arthroplasty. J. Am. Acad. Ortho. Surg., December 2005; 13: 515 – 524 Paul J. Favorito, William M. Mihalko, and Kenneth A. Krackow. Total Knee Arthroplasty in the Valgus Knee. J. Am. Acad. Ortho. Surg., January/February 2002; 10: 16 - 24. Matthew R. Bong and Paul E. Di Cesare. Stiffness After Total Knee Arthroplasty J. Am. Acad. Ortho. Surg., May/June 2004; 12: 164 - 171. Christopher J. Vertullo, Mark E. Easley, W. Norman Scott, and John N. Insall Mobile Bearings in Primary Knee Arthroplasty. J. Am. Acad. Ortho. Surg., November/December 2001; 9: 355 – 364 Robert L. Barrack and Michael W. Wolfe. Patellar Resurfacing in Total Knee Arthroplasty. J. Am. Acad. Ortho. Surg., March/April 2000; 8: 75 - 82. Michel Malo and Kelly G. Vince. The Unstable Patella After Total Knee Arthroplasty: Etiology, Prevention, and Management. J. Am. Acad. Ortho. Surg., September/October 2003; 11: 364 - 371. David A. Parker, Michael J. Dunbar, and Cecil H. Rorabeck. Extensor Mechanism Failure Associated With Total Knee Arthroplasty: Prevention and Management. J. Am. Acad. Ortho. Surg., July/August 2003; 11: 238 – 247 Donna E. Smith, Robert W. McGraw, David C. Taylor, and Bassam A. Masri. Arterial Complications and Total Knee Arthroplasty. J. Am. Acad. Ortho. Surg., July/August 2001; 9: 253 – 257 John R. Watterson and John M. Esdaile. Viscosupplementation: Therapeutic Mechanisms and Clinical Potential in Osteoarthritis of the Knee. J. Am. Acad. Ortho. Surg., September/October 2000; 8: 277 - 284. 7 JH Lonner and PA Lotke. Aseptic complications after total knee arthroplasty J. Am. Acad. Ortho. Surg., Sep 1999; 7: 311 - 324. Vince KG, Abdeen A. Wound problems in total knee arthroplasty. Clin Orthop Relat Res. 2006 Nov;452:88-90. Cui Q, Mihalko WM, Shields JS, Ries M, Saleh KJ. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J Bone Joint Surg Am. 2007 Apr;89(4):871-82. Sheth NP, Pedowitz DI, Lonner JH. Periprosthetic patellar fractures. J Bone Joint Surg Am. 2007 Oct;89(10):2285-96. Hip Reference textbooks Campbells Operative Orthopaedics, 10th edition, chapter 7 AAOS Orthopaedic Basic Science Text book Journal articles Michael A. Mont, Phillip S. Ragland, Gracia Etienne, Thorsten M. Seyler, and Thomas P. Schmalzried, Hip Resurfacing Arthroplasty. J. Am. Acad. Ortho. Surg., August 2006; 14: 454 - 463. Maximillian Soong, Harry E. Rubash, and William Macaulay. Dislocation After Total Hip Arthroplasty. J. Am. Acad. Ortho. Surg., September/October 2004; 12: 314 – 321 Richard Iorio and William L. Healy Heterotopic Ossification After Hip and Knee Arthroplasty: Risk Factors, Prevention, and Treatment. J. Am. Acad. Ortho. Surg., November/December 2002; 10: 409 – 416 MM DeHart and LH Riley, Jr. Nerve injuries in total hip arthroplasty. J. Am. Acad. Ortho. Surg., Mar 1999; 7: 101 – 111 Charles R. Clark, Herbert D. Huddleston, Eugene P. Schoch, III, and Bert J. Thomas Leg-Length Discrepancy After Total Hip Arthroplasty. J. Am. Acad. Ortho. Surg., January 2006; 14: 38 - 45. Alejandro González Della Valle, Douglas E. Padgett, and Eduardo A. Salvati Preoperative Planning for Primary Total Hip Arthroplasty. J. Am. Acad. Ortho. Surg., November 2005; 13: 455 – 462 Richard J. Friedman. Optimal Duration of Prophylaxis for Venous Thromboembolism Following Total Hip Arthroplasty and Total Knee Arthroplasty. J. Am. Acad. Ortho. Surg., March 2007; 15: 148 – 155 Della Valle CJ, Zuckerman JD, Di Cesare PE. Periprosthetic sepsis. Clin Orthop Relat Res. 2004 Mar;(420):26-31 Hanssen AD, Spangehl MJ. Treatment of the infected hip replacement. Clin Orthop Relat Res. 2004 Mar;(420):63-71. Babis GC, Soucacos PN. Effectiveness of total hip arthroplasty in the management of hip osteonecrosis. Orthop Clin North Am. 2004 Jul;35(3):359-64 Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B.Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005 Jun;87(6):762-9. Lieberman JR, Hsu WK. Prevention of venous thromboembolic disease after total hip and knee arthroplasty. J Bone Joint Surg Am. 2005 Sep;87(9):2097-112. Beksaç B, González Della Valle A, Salvati EA. Thromboembolic disease after total hip arthroplasty: who is at risk? Clin Orthop Relat Res. 2006 Dec;453:211-24. Parvizi J, Campfield A, Clohisy JC, Rothman RH, Mont MA. Management of arthritis of the hip in the young adult. J Bone Joint Surg Br. 2006 Oct;88(10):1279-85. Board TN, Karva A, Board RE, Gambhir AK, Porter ML. The prophylaxis and treatment of heterotopic ossification following lower limb arthroplasty. J Bone Joint Surg Br. 2007 Apr;89(4):434-40. Dezateux C, Rosendahl K. Developmental dysplasia of the hip. Lancet. 2007 May 5;369(9572):1541-52. 8