File - Respiratory Therapy Files
advertisement
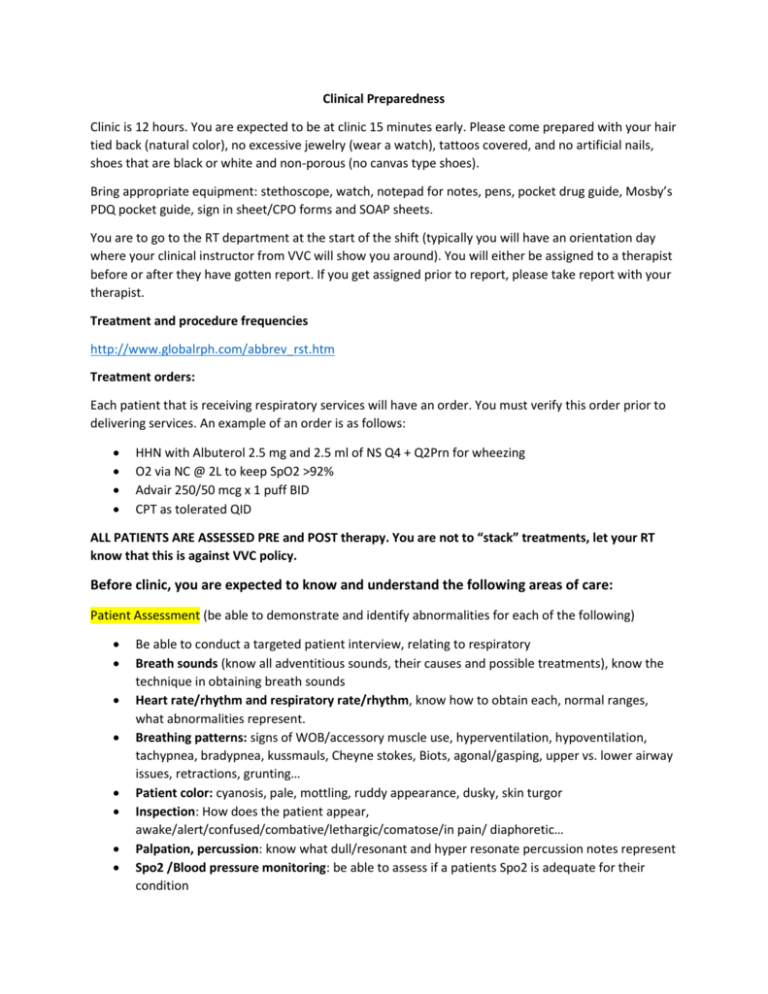
Clinical Preparedness Clinic is 12 hours. You are expected to be at clinic 15 minutes early. Please come prepared with your hair tied back (natural color), no excessive jewelry (wear a watch), tattoos covered, and no artificial nails, shoes that are black or white and non-porous (no canvas type shoes). Bring appropriate equipment: stethoscope, watch, notepad for notes, pens, pocket drug guide, Mosby’s PDQ pocket guide, sign in sheet/CPO forms and SOAP sheets. You are to go to the RT department at the start of the shift (typically you will have an orientation day where your clinical instructor from VVC will show you around). You will either be assigned to a therapist before or after they have gotten report. If you get assigned prior to report, please take report with your therapist. Treatment and procedure frequencies http://www.globalrph.com/abbrev_rst.htm Treatment orders: Each patient that is receiving respiratory services will have an order. You must verify this order prior to delivering services. An example of an order is as follows: HHN with Albuterol 2.5 mg and 2.5 ml of NS Q4 + Q2Prn for wheezing O2 via NC @ 2L to keep SpO2 >92% Advair 250/50 mcg x 1 puff BID CPT as tolerated QID ALL PATIENTS ARE ASSESSED PRE and POST therapy. You are not to “stack” treatments, let your RT know that this is against VVC policy. Before clinic, you are expected to know and understand the following areas of care: Patient Assessment (be able to demonstrate and identify abnormalities for each of the following) Be able to conduct a targeted patient interview, relating to respiratory Breath sounds (know all adventitious sounds, their causes and possible treatments), know the technique in obtaining breath sounds Heart rate/rhythm and respiratory rate/rhythm, know how to obtain each, normal ranges, what abnormalities represent. Breathing patterns: signs of WOB/accessory muscle use, hyperventilation, hypoventilation, tachypnea, bradypnea, kussmauls, Cheyne stokes, Biots, agonal/gasping, upper vs. lower airway issues, retractions, grunting… Patient color: cyanosis, pale, mottling, ruddy appearance, dusky, skin turgor Inspection: How does the patient appear, awake/alert/confused/combative/lethargic/comatose/in pain/ diaphoretic… Palpation, percussion: know what dull/resonant and hyper resonate percussion notes represent Spo2 /Blood pressure monitoring: be able to assess if a patients Spo2 is adequate for their condition Cough and sputum assessment: Be able to assess and discuss abnormalities in sputum color, consistency, smell. Have you patient demonstrate the ability or inability to cough Lung mechanics: Be able to demonstrate knowledge of a Vital Capacity Maneuver (VC), NIF/MIP ABG interpretation, and indications for puncture Basic EKG interpeations: know lead two rhythms (A-fib, Sinus tachycardia, bradycardia, SVT, Vtach, V-fib, Blocks: Types I-III…) ALL FORMULAS learned: Ve, VA, PAO2, CaO2, total flow, duration of flow… Be able to make recommendations based on your assessment. Chart Review (be able to review a chart and extract the below information) LABS: Be able to interpret and discuss abnormalities, associate them with the patients current condition o CBC: WBC (the differential), Hb, RBC, HCT, Platlets o Electrolytes: K, Na, Ca, Mg, Cl, Phosphorous o BUN, Creatine o Liver enzymes: ALT o Cardiac enzymes: CPK, troponine, BNP o Sputum, blood and urine analysis/microbiology o Essentially you are to review all abnormal labs and relate them to the patients current condition CXR/CT scan: Review for abnormalities, interpret consolidation, pneumothorax, pleural effusion, pulmonary edema, atelectasis… All structures, ribs/trachea/stomach... History and Physical and consultations: all disease you encounter in the chart, please review them, common issues among patients will include: Diabetes II, CHF, CAD, CRF, ESRD, COPD, Obesity, OSA, ETOH abuse, Liver cirrhosis, STEMI, CVA, Cancer… Pulmonary Function tests: Review if the patient has undergone one, and what the results mean Respiratory and nursing notes MAR: all medications Code status, isolation status, known allergens Bronchial Hygiene (be able to demonstrate knowledge in each of the below topics) Know indications for bronchial hygiene, including patients who have ineffective coughs, no cough, congestion or who are predisposed to congestion Know the following equipment: o EZPAP o Acupella o Flutter devices o Cough Assist o Aerobika o Thera-PEP Be able to demonstrate proper patient positioning and CPT using hand technique, percussive device and the vest Understand the indication and techniques used during bronchoscopy, know the different types Nasotracheal suctioning vs. Tracheal suctioning, technique and indications, sputum collection Basic airway management: o Trachestomy care, intubation, nasal and oral airway placement and indications Humidity and aerosol therapy: Know when aerosol and humidity is indicated and how to setup: o Bubble humidifier o Large Volume nebulizer o Small volume nebulizer o Heated humidifier (Passover and wick) o HME Positive Pressure/Hyperinflation Know the indications and basic function of non-invasive positive pressure (BiPAP) o Be able to describe CPAP vs BiPAP IPPB: all settings, indications, contraindications and hazards IPV: all settings, indications, contraindications and hazards Using a positive pressure mask during CPR Indications for mechanical ventilation Indications and use of an Incentive Spirometer Other Equipment ALL Oxygen devices, low flow, high flow and enclosure systems Peak flow meters Holding chambers DPI, MDI Pulse oximeters Capnography SVN, BAN (know how to cough and instruct the patient to take a treatment) Spirometry Oxygen analyzers Regulators and cylinders EKG machines Hyperbaric Oxygen systems Pharmacology Gas therapy: Know indications, hazards/side effects for Oxygen, Heliox, Nitric Oxide Know indications, hazards/side effects, doses, frequency, and onset/duration, drug classification, Receptor site mechanisms and mode of action for the following respiratory therapy drugs: o Albuterol o Atrovent o Duoneb o Xopenex o Spiriva o Combivent o Serevent o Dulera o Foradil o Racemic o Advair o Brovana Epinephrine o Symbicort o Mucomyst o o o o o o Dornase Alfa Sodium Bicarbonate Nebupent Flovent Qvar Asmanex o o o o o o o Breo Elliepta Tudorza Curosurf Pulmicort Tobi Predinsone Solumederol o o o o o o o Lasix Decadron Singulair Aerospan Xolair Accolate Flolan