correlation of fat fraction, diffusivity, metabolic activity and
advertisement

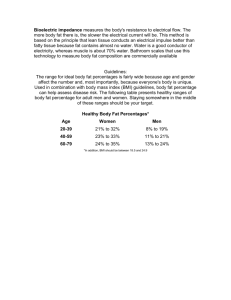
1 Multiparametric analysis of bone marrow in cancer patients using simultaneous PET/MR imaging: correlation of fat fraction, diffusivity, metabolic activity and anthropometric data 1 2 Abstract Purpose To analyze the regional composition of bone marrow (BM) in correlation with metabolic activity and diffusivity using simultaneous PET/MRI (positron emission tomography / magnetic resonance imaging). Materials and Methods Retrospective analysis of 18F-FDG-PET/MR scans of 110 patients was performed. A 3D gradient-echo sequence with Dixon-based fat-water-separation was used for fat quantification. Dixon images, diffusion-weighted images (DWI) and 18F-FDG-PET were co-registered. Mean values of fat fraction (FF), standardized uptake value (SUV) and apparent diffusion coefficient (ADC) of BM were measured in different anatomical regions. Correlation of FF, SUV and ADC and association of BM fat content and metabolic activity with anthropometric data was analyzed (Pearson). BM fat content and metabolic activity was compared in patients with and without chemotherapy (t-test). Results Regional differences in BM were found with highest fat content (93 ± 8 %) and lowest ADC (0.22 ± 0.18 x 10-3 mm²/s) in the peripheral skeleton and highest SUV in the spine (1.77 ± 0.6). There was a significant inverse correlation between FF and SUV (r = 0.73; p = 0.0001) and a significant correlation between FF and ADC (r = -0.62; p < 0.0001). In patients with chemotherapy, a tendency to higher fat content and lower metabolic activity was observed in the proximal skeleton, although no statistical significance was reached. Conclusions BM shows distinct regional variations in FF, SUV and ADC. The inverse correlation of FF and SUV in BM suggests that BM adipose tissue does not have a comparable high metabolic activity as brown adipose tissue. Key words: bone marrow, adipose tissue, fat quantification, PET/MRI, diffusionweighted imaging, 18F-FDG 2 3 Introduction Human bone marrow (BM) is a large complex and dynamic organ, which is involved in a number of physiological processes. Distribution, composition and metabolic activity of BM are mutable and can be influenced by various conditions such as age, body weight, endocrinologic factors, and drugs (1-4). BM may also be changed in oncological, degenerative and inflammatory diseases (5, 6). For a long time, the BM fat has been considered metabolically inactive (7, 8). Recent studies, however, have changed this perception: Bone marrow adipose tissue, hematopoietic marrow and trabecular bone mass have been shown to be interrelated through a pluripotent mesenchymal stem cell which is capable of differentiating into adipocytic, hematopoietic and osteocytic cell lines (7, 9, 10). Lately, it has even been reported that BM adipose tissue reveals characteristics of both white and brown adipose tissue (11). This could imply that the metabolic activity of BM adipose tissue might differ from white subcutaneous fat. Thus, investigating the metabolic activity of BM in correlation with its fat content is an essential step towards a deeper understanding of BM adipose tissue. Knowledge of the multiparametric characteristics of BM is useful to avoid misinterpretation of imaging studies. Today, invasive BM biopsy still represents the gold standard for the evaluation of BM. However, this method analyzes only a small sample volume and is therefore not a suitable tool for the evaluation of the entire BM in the skeleton. Cross-sectional imaging techniques such as computed tomography (CT) and magnetic resonance imaging (MRI) can provide whole-body evaluation of BM distribution. Metabolic activity of BM can be visualized using positron emission tomography (PET) with the glucose analog 2-[18F]fluoro-2-deoxy-d-glucose (18F-FDG) - as the tracer physiologically accumulates in BM (12). Sambuceti et al. have recently 3 4 given a first estimation of extension and metabolism of BM throughout the skeleton using 18F-FDG-PET/CT (5). In this study, the differentiation between red and yellow marrow was based on the metabolic activity using an arbitrary threshold of the mean standard uptake value (SUV) of 1.11. However, in MRI studies, accurate differentiation of fat and water can be performed using proton chemical shift imaging (13, 14). This MRI technique makes use of the different resonance frequencies of precessing spins of fat and water in order to obtain quantitative information about water and fat content of a given tissue (15). Thus, objective quantification of the regional fat content of BM can be performed throughout the whole skeleton. In addition, diffusion-weighted imaging (DWI) as a quantitative functional imaging technique is being applied increasingly for the assessment of BM because of its sensitivity to cell density, i.e., depicting a correlate of the relative content of fat and marrow cells, water content and BM perfusion (16-19). By combining these MRI techniques, qualitative and quantitative characterization of BM in every location of the skeleton can be performed non-invasively. During the last years, the two modalities PET and MRI have been combined in simultaneous clinical hybrid PET/MR scanners. They offer the possibility to simultaneously assess structural and functional characteristics of BM by analyzing the spatial distribution and fat fraction (FF) of BM using MRI, in correlation with its metabolic activity as reflected by the 18F-FDG-uptake. Using this new hybrid technique it is possible to correlate human BM composition with metabolic activity and cell density. The aim of the present study was twofold: first, to analyze the composition of human BM in the skeleton of patients in correlation with metabolic activity and diffusion 4 5 properties using a simultaneous PET/MR scanner. Second, to investigate the influence of anthropometric factors on BM composition and metabolic activity. 5 6 Materials and Methods Patient population After institutional review board approval of the study, retrospective analysis of 110 whole-body 18F-FDG-PET/MR patient data sets acquired consecutively from 03/2011 to 01/2012 was performed. All patients had given written informed consent for the scientific evaluation of their data. Patients’ (58 female, 52 male) median age was 54 ± 19 years (range: 3 - 80 years; Figure 1). Median BMI of patients was 24.0 ± 4.9 kg/m² (range: 12.5 - 38.1 kg/m²). All patients underwent 18F-FDG-PET/MRI after a clinically indicated PET/CT. Clinical indication for PET/CT was staging or follow-up examination of the following primary diseases: anal cancer (n=9), appendix cancer (n=1), lung cancer (n=5), cholangiocellular cancer (n=1), colorectal cancer (n=16), cancer of unknown primary (n=8), small bowel cancer (n=1), endometrial cancer (n=2), aggressive fibromatosis (1), fever of unknown origin (n=3), oro- and hypopharyngeal cancer (n=2), lymphoma (n=13), gastric cancer (n=3), breast cancer (n=5), melanoma (n=7), mesothelioma (n=2), neurofibromatosis (n=1), neuroendocrine tumor (n=1), ovarian cancer (n=12), pancreatic cancer (n=1), parotideal cancer (n=1), PNET (n=2), sarcoma (n=3), thyroid cancer (n=6), seminoma (n=3), cervical cancer (n=1). 59 patients had chemotherapy in their medical history. Median time interval between PET/MRI and last chemotherapy was 8 ± 34 months (range: 0 - 228 months). 10 patients were undergoing chemotherapeutic treatment at the time of the PET/MR examination. PET/MR examination 6 7 All patients fasted overnight. Before tracer injection (median dose 18F-FDG 352 ± 56 MBq; range: 61 - 386 MBq), blood glucose levels were measured (median: 117 ± 21 mg/dl, range: 81 - 198 mg/dl). During the uptake phase, patients were instructed to lie still and avoid movement. PET/MRI was performed 120 ± 12 min (median: 120 min, range: 101 - 166 min) after radiotracer injection in a clinical simultaneous whole-body 3T PET/MR scanner (Biograph mMR, Siemens Healthcare). PET acquisition and reconstruction PET acquisition lasted 6 minutes per bed. Number of bed positions varied between 3 to 6 depending on the patient’s size. PET data were reconstructed using an iterative three-dimensional (3D) ordered-subset expectation maximization (OSEM) algorithm (20, 21) with three iterations, 21 subsets and a Gaussian filter of 3 mm. MR-based PET attenuation correction was performed using a segmentation-based approach after fat-water separation (22) provided by the vendor. Mean standardized uptake values (SUVmean) were used to evaluate 18F-FDG uptake of BM. MR sequence parameters FF quantification was performed using a coronal 3D T1-weighted spoiled gradientecho sequence with Dixon-based fat-water separation (23). The sequence is also used for the generation of segmentation-based PET attenuation correction maps. Sequence parameters were as follows: repetition time (TR) 3.6 ms, echo time (TE) TE1 1.23 ms, TE2 2.46 ms; excitation angle 10°; bandwidth 965 Hz/pixel; matrix size 79 x 192; pixel size 2.6 x 2.6 x 2.6 mm³; 128 slices per slab; parallel imaging acceleration factor 2; time of acquisition (TA) 19 s. Axial diffusion-weighted imaging was performed using a single shot echoplanar imaging (EPI) sequence under free breathing with TR/TE 13300 ms/76 ms; flip angle 7 8 90°; diffusion gradients in three orthogonal directions with two b-values (50 and 800 s/mm²); matrix size 104 x 138; resolution 2.8 x 2.8 x 6.0 mm³; parallel imaging acceleration factor 2; averages 3, spectral adiabatic inversion recovery (SPAIR) fat suppression; TA 3 min 20 s. Apparent diffusion coefficient (ADC) maps were calculated based on a mono-exponential fit using the built-in manufacturer’s software (SYNGO, Siemens Healthcare). Data evaluation All Dixon images were assessed visually to exclude potential phase artifacts resulting in fat-water swaps affecting accurate FF quantification. Dixon images, ADC maps and PET data were re-sampled to the same spatial resolution, co-registered and depicted in three planes for the volumetric evaluation of the defined BM regions, using an institutional Matlab program (Imagine 1.2, Matlab Central File Exchange, MathWorks Inc., Matwick, USA). . Volumetric analysis of predefined regions (humerus, thoracic spine, lumbar spine, pelvis, and femur) was performed in a 3D analysis. ROIs were drawn manually by two readers in consensus (M.S.; 1 year of experience and C.S.; 10 years of experience) in subsequent Dixon images and automatically transferred to the co-registered ADC map and PET. ROIs were combined to a VOI and the mean value of each VOI was calculated and used for statistical analysis. In the humerus, the femur, and the pelvis, bilateral VOIs were outlined and their mean value was used for data evaluation. For the two spine regions, two vertebrae were outlined for each the thoracic and the lumbar spine and the mean values were used for data evaluation, respectively. An example for the image data used for evaluation is shown in Figure 2. Care was taken not to include cortical bone. The skull was not evaluated, as the spillover of brain PET activity would have prevented accurate measurement of the SUV in this region. Regions with 8 9 obvious osseous lesions or osseous metastases or in field of a prior radiation therapy were excluded by C.S. based on clinical history and by visual analysis of all available image data. Fat quantification of BM was calculated using the coronal 3D T1weighted spoiled gradient-echo sequence with Dixon-based fat-water separation. FF was calculated from the relative signal intensity of the fat images divided by the signal intensity of the in-phase images. FFmean (in %), mean SUV (SUVmean) and mean apparent diffusion coefficient (ADCmean) of each VOI were assessed. Mean VOI volume was 23 cm³ in the humerus, 6 cm³ in the thoracic spine, 13 cm³ in the lumbar spine, 15 cm³ in the pelvis and 27 cm³ in the femur. Statistical analysis All statistical analyses were performed using statistical software (JMP 11.0; SAS Institute, Cary, NC). Normal distribution was verified using the Shapiro Wilk test. The Pearson test was used to measure the significance of the association of FF mean with SUVeman and ADCmean, respectively. The association of age, body mass index (BMI) and fasting blood glucose level with BM fat content and metabolic activity was analyzed using Pearson correlation coefficient. Fat content and metabolic activity of BM in male and female patients were compared for each anatomical region using Student’s t-test. Accordingly, fat content and metabolic activity in patients with and without chemotherapy were compared for each anatomical region using Student’s t-test. Bonferroni correction for multiple testing was performed. P values < 0.01 were considered to be statistically significant. 9 10 Results In five patients, the Dixon images showed water fat flip artifacts that did not allow for reliable fat quantification (Figure 3). Therefore, these data sets were excluded for further evaluation. Two patient data sets with adequate imaging quality for further evaluation are exemplarily shown in Figure 4 and 5. Box plot diagrams summarizing FFmean, SUVmean as well as ADCmean obtained in the different skeletal regions are shown in Figure 6 a-c. Fat content was highest in the extremities as assessed in humerus (mean ± standard deviation: 93 ± 8 %, median 95 %, range: 55 - 99 %) and femur (89 ± 7 %; median 90 %, range: 60 - 98 %) and lowest in the thoracic vertebrae (52 ± 15 %; median 55 %, range: 3 - 83 %). FFmean was 62 ± 16 % (median 66 %, range: 4 - 95 %) in the lumbar spine and 74 ± 13 % (median: 76 %, range: 23 - 96 %) in the pelvis (Figure 6a). SUVmean was highest in the thoracic spine (mean ± standard deviation: 1.77 ± 0.6; median 1.75, range: 0.19 - 4.08) and lumbar spine (mean ± standard deviation: 1.50 ± 0.50, median: 1.46, range: 0.20 - 3.77) and lowest in the extremities with a mean value of 0.50 ± 0.28 in the humerus (median 0.44, range: 0.23 - 1.90) and mean value of 0.56 ± 0.23 in the femur (median: 0.59, range: 0.02 - 1.65) (Figure 6b). ADCmean was lowest in the extremities with a mean value in the humerus of 0.218 ± 0.178 x 10-3 mm²/s (median: 0.174 x 10-3 mm²/s, range: 0.03 - 0.863 x 10-3 mm²/s) and in the femur of 0.207 ± 0.123 x 10 -3 mm²/s (median: 0.191 x 10-3 mm²/s, range: 0.20 - 0.840 x 10-3 mm²/s). ADCmean was highest in the thoracic spine with 0.464 ± 0.380 x 10-3 mm²/s (median: 0.369 x 10-3 mm²/s, range: 0.091 - 2.942 x 10-3 mm²/s) and intermediate in the lumbar spine (0.305 ± 0.169 x 10 -3 mm²/s, median: 0.280 x 10 11 10-3 mm²/s, range: 0.034 - 1.229 x 10-3 mm²/s) and in the pelvis 0.351 ± 0.161 x 10 -3 mm²/s, median: 0.326 x 10-3 mm²/s, range: 0.086 - 1.145 x 10-3 mm²/s) (Figure 6c). There was a significant strong to moderate inverse correlation of fat content with 18FFDG uptake in all regions, and there was a significant moderate inverse correlation of fat content and ADC in all regions except for the thoracic spine (Table 1). Analysis of fat fraction and metabolic activity with respect to anthropometric data (sex, age, BMI, blood glucose level) 10 patients were less than 20 years of age (three less than 10 years) (Figure 1). Lower fat content was observed in all skeletal regions in these patients, whereas in the SUVmean measurements no trend was observable. Due to the very limited number of young patients, no separate statistical comparison was performed. Significant positive correlation was observed between age and BM fat content for all regions except for the humerus (thoracic spine: r = +0.38; lumbar spine: +0.55; pelvis: +0.58; femur: +0.53; all p < 0.0001). In all predefined regions, no significant difference between male and female patients was observed regarding the fat content and the 18F-FDG uptake (detailed evaluation see Table 2a+b). BMI was not significantly associated with FFmean of BM in all evaluated skeletal regions. In contrast, there was a positive correlation of BMI and SUVmean in all regions, reaching statistical significance in the humerus (r = 0.56; p = 0.0252), thoracic spine (r = 0.36; p = 0.0002) and the pelvis (r = 0.44; p = 0.0213). 11 12 In our study, no significant correlation between BM fat content and blood glucose was found in all evaluated skeletal regions. Chemotherapy Patients during chemotherapy: Patients undergoing chemotherapy at the time of the PET/MR examination (n = 10) showed a tendency to lower FF mean and a higher mean SUVmean and ADCmean of BM in all regions. However, this trend did not reach statistical significance. Patients with prior chemotherapy: Patients who had previous chemotherapy in the medical history (n = 59) presented with a tendency to higher fat content in BM of the proximal skeleton (thoracic spine, lumbar spine, pelvis). However, with Bonferroni correction, no statistical significance was reached (details see Table 3a). This tendency was observed irrespective of the time period between the last chemotherapy application and the PET/MR examination. In contrast, no relevant difference in FFmean was observed in the peripheral skeleton as represented by the humerus and femur. Correspondingly, a tendency to lower SUVmean was found in patients with previous chemotherapy in the proximal skeleton (Table 3b), although no statistical significance was reached. 12 13 Discussion Modern hybrid imaging modalities such as PET/MRI have great potential for the investigation of BM. In the present study, the BM fat content as calculated by the Dixon method could be quantitatively assessed and directly correlated with the metabolic activity. This could not have been performed as accurate when using PET/CT due to the limited possibility for accurate BM fat quantification by CT methods. However, dual-energy techniques might be useful to overcome this limitation in the future (24). Our study results reveal differences between the peripheral and proximal skeleton regarding BM fat content and metabolic activity with highest fat content in the extremities and lowest in the spine and correspondingly inverse results regarding the 18F-FDG uptake. These findings reflect the known centripetal conversion pattern of BM with age that shows a replacement of red marrow by fatty marrow beginning in the distal parts of the extremities, subsequently processing to the more proximal parts of the skeleton (25). Conversely, the metabolic activity as reflected by the glucose uptake measured with the SUVmean was highest in the proximal skeleton and lowest in the extremities. In the present study, the SUVmean of BM measured in the different predefined skeletal regions were in good accordance with data published in the literature (26, 27). The significant strong inverse correlation of 18F-FDG uptake and fat content in BM suggests that the metabolic activity of BM is mainly represented by the red marrow. This, in turn, ascribes only minor metabolic activity to BM adipose tissue. Therefore, results of the present study do not support the hypothesis that BM adipose tissue 13 14 could have a comparably high metabolic activity as observed for brown adipose tissue (11). The ADC values of BM measured in our study lie within the range of the values reported in the literature (18, 28, 29). Moreover, inverse correlation of ADC and fat content of BM was observed in the present study. As an explanation for this finding various factors can be discussed. First, there is a restricted mobility of lipid-bound water molecules in contrast to non-lipid bound protons (30). Second, the overall water content is higher in red BM because hematopoietically active marrow (cellular marrow) has more intracellular water and also more adjacent free water than does the metabolically less active yellow marrow. This seems to enable more molecular diffusion in cellular marrow (29). Another influencing factor for the observed higher BM diffusivity in red marrow could be a higher perfusion fraction in red bone marrow. However, this effect should be less important when using higher b values as chosen in present study. In the present study, significant positive correlation was observed between BM fat content and age in all predefined regions except for the humerus. A possible explanation for this finding might be that the fat conversion of BM in the humerus starts at a younger age so that the linearity of the correlation is no longer as evident in an older patient population such as in our patient collective with a median age of 54 years. In the literature, age-dependent sex differences in BM composition have been reported with higher fat content in younger males and in elder females (7, 31). Sex hormones and menstrual blood loss are discussed as potential causes (32). In contrast, we did not observe significant gender differences regarding fat content or 18F-FDG uptake in BM. The discrepancy may be explained by the different study 14 15 populations (healthy volunteers versus patients). Moreover, we did not perform agematched comparisons due to the limited number of patient data per age group. Besides, as we were consecutively including the patients for the analysis, we were unable to perform gender comparison in matched age groups. We did not observe a significant correlation between BMI and BM fat content in the evaluated regions of the skeleton. This is in accordance with data reported in the literature. Bredella and colleagues (33) investigated the association of BMI and BM fat in the L4 vertebra in 106 patients using MR spectroscopy. They found a positive correlation between BM fat with weight but not with BMI. In contrast to our study setup, their study was performed in a younger obese patient population. Although we analyzed different skeletal regions in an elder – mostly oncologic – patient cohort we obtained comparable results. In our study, no significant correlation between BM fat content and blood glucose was found in all skeletal regions (33, 34). This is in accordance with published studies using MR proton spectroscopy for fat quantification. (34). In the Baum study, the authors quantified BM fat in the vertebral bodies (L1-3)in diabetic and nondiabetic postmenopausal women. In the Bredella study, BM fat was assessed in the L4 vertebra in 106 healthy young men and women. In both studies, no correlation between fasting blood glucose level and vertebral BM fat content was found. In contrast to ours, the aforesaid studies were performed in non-cancer populations. .It It is known that chemotherapy has a myelosuppressive effect on BM and decreased marrow functioning has been reported for up to several years after chemotherapy (35). The degree and the time course of BM suppression (nadir, time to marrow recovery) vary among the different chemotherapeutic drugs (35). In our study, higher fat content of the proximal skeleton (spine and pelvis) was found by trend in patients 15 16 who had chemotherapy in their medical history, irrespective of the time interval between chemotherapy and examination. Correspondingly, lower SUVmean were observed by trend in the proximal skeleton regions (such as spine and pelvis). These findings underline the assumption that chemotherapy might have long-term effects on the composition and metabolic activity of BM. It is also plausible that the influence of chemotherapy is more distinct in bone regions that have a physiologically higher persistent red marrow fraction such as the proximal skeleton where up to 60 % of the entire red marrow are located in adults (35, 36). The present study has limitations. The population evaluated in this single institution study was a cohort of convenience with broad heterogeneity regarding primary tumor and prior therapy. Due to the retrospective study design, the data originate from PET/MR patients who were consecutively included in the evaluation. .As a consequence there is a certain bias regarding the age distribution with only a small number of younger subjects. Second, bone is not represented as a separate tissue class in the MR-based method for attenuation correction (MRAC) provided by the manufacturer. This may lead to errors in the SUV quantification in bone regions because bone is ignored in the MRAC. In previous studies investigating the effect on SUV quantification in bone an underestimation of up to 14 % has been reported (37). This underestimation, however, is comparable for all bone regions so that the correlation analysis results should not be influenced. Further improvements in the MRAC technique such as the approach of separating bone and air using ultrashortecho-time sequences might contribute to overcome this shortcoming in the future and might even allow for compensation of different thicknesses of cortical bone at different anatomical positions (38). Finally, in the present study setup, VOI positioning and alignment quality of the registration is an important issue because VOI 16 17 positioning can markedly influence FF, SUV and ADC measurements for the final evaluation. In order to reduce partial volume effects, all VOIs were visually checked to assure correct positioning within normal BM and to avoid cortical bone or lesions within the bone. To increase representativeness of mean values manually positioned VOIs were drawn as large as possible. In the present study, BM fat content was assessed non-invasively in different regions of the human skeleton in correlation with its metabolic activity and diffusion properties in a representative number of PET/MR patients. BM shows distinct regional differences in fat content, 18F-FDG uptake and ADC. The significant strong inverse correlation of fat content and 18F-FDG uptake in BM suggests that the metabolic activity of BM can mainly be attributed to red marrow and that BM adipose tissue does not have a comparable high metabolic activity as reported from brown adipose tissue. Chemotherapy seems to have long-term effects on composition and metabolic activity of BM in the proximal skeleton. The presented study results broaden the knowledge about BM characteristics in oncologic patients, which is an important prerequisite for the accurate interpretation 17 of clinical PET/MR images. 18 References 1. Vande Berg BC, Lecouvet FE, Galant C, Simoni P, Malghem J. Normal variants of the bone marrow at MR imaging of the spine. Seminars in musculoskeletal radiology. 2009;13(2):87-96. 2. Blebea JS, Houseni M, Torigian DA, et al. Structural and functional imaging of normal bone marrow and evaluation of its age-related changes. Seminars in nuclear medicine. 2007;37(3):185-94. 3. Fan C, Hernandez-Pampaloni M, Houseni M, et al. Age-related changes in the metabolic activity and distribution of the red marrow as demonstrated by 2-deoxy-2[F-18]fluoro-D-glucose-positron emission tomography. Molecular imaging and biology : MIB : the official publication of the Academy of Molecular Imaging. 2007;9(5):300-7. 4. Goethals I, Hoste P, De Vriendt C, Smeets P, Verlooy J, Ham H. Time- dependent changes in 18F-FDG activity in the thymus and bone marrow following combination chemotherapy in paediatric patients with lymphoma. Eur J Nucl Med Mol Imaging. 2010;37(3):462-7. 5. Sambuceti G, Brignone M, Marini C, et al. Estimating the whole bone-marrow asset in humans by a computational approach to integrated PET/CT imaging. Eur J Nucl Med Mol Imaging. 2012;39(8):1326-38. 6. Meyer MA, Nathan CO. Reduced F-18 fluorodeoxyglucose uptake within marrow after external beam radiation. Clinical nuclear medicine. 2000;25(4):279-80. 7. Griffith JF, Yeung DK, Ma HT, Leung JC, Kwok TC, Leung PC. Bone marrow fat content in the elderly: a reversal of sex difference seen in younger subjects. Journal of magnetic resonance imaging : JMRI. 2012;36(1):225-30. 18 19 8. Gimble JM, Robinson CE, Wu X, Kelly KA. The function of adipocytes in the bone marrow stroma: an update. Bone. 1996;19(5):421-8. 9. Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult human mesenchymal stem cells. Science (New York, NY). 1999;284(5411):143-7. 10. Rosen CJ, Ackert-Bicknell C, Rodriguez JP, Pino AM. Marrow fat and the bone microenvironment: developmental, functional, and pathological implications. Critical reviews in eukaryotic gene expression. 2009;19(2):109-24. 11. Krings A, Rahman S, Huang S, Lu Y, Czernik PJ, Lecka-Czernik B. Bone marrow fat has brown adipose tissue characteristics, which are attenuated with aging and diabetes. Bone. 2012;50(2):546-52. 12. Murata Y, Kubota K, Yukihiro M, Ito K, Watanabe H, Shibuya H. Correlations between 18F-FDG uptake by bone marrow and hematological parameters: measurements by PET/CT. Nucl Med Biol. 2006;33(8):999-1004. 13. Buxton RB, Wismer GL, Brady TJ, Rosen BR. Quantitative proton chemical- shift imaging. Magn Reson Med. 1986;3(6):881-900. 14. Dixon WT. Simple proton spectroscopic imaging. Radiology. 1984;153(1):189- 94. 15. Hood MN, Ho VB, Smirniotopoulos JG, Szumowski J. Chemical shift: the artifact and clinical tool revisited. Radiographics. 1999;19(2):357-71. 16. Biffar A, Dietrich O, Sourbron S, Duerr HR, Reiser MF, Baur-Melnyk A. Diffusion and perfusion imaging of bone marrow. European journal of radiology. 2010;76(3):323-8. 19 20 17. Messiou C, deSouza NM. Diffusion Weighted Magnetic Resonance Imaging of metastatic bone disease: A biomarker for treatment response monitoring. Cancer biomarkers : section A of Disease markers. 2010;6(1):21-32. 18. Padhani AR, van Ree K, Collins DJ, D'Sa S, Makris A. Assessing the relation between bone marrow signal intensity and apparent diffusion coefficient in diffusionweighted MRI. AJR American journal of roentgenology. 2013;200(1):163-70. 19. Hillengass J, Stieltjes B, Bauerle T, et al. Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) and diffusion-weighted imaging of bone marrow in healthy individuals. Acta radiologica (Stockholm, Sweden : 1987). 2011;52(3):324-30. 20. Hudson HM, Larkin RS. Accelerated image reconstruction using ordered subsets of projection data. IEEE transactions on medical imaging. 1994;13(4):601-9. 21. Shepp LA, Vardi Y. Maximum likelihood reconstruction for emission tomography. IEEE transactions on medical imaging. 1982;1(2):113-22. 22. Martinez-Moller A, Souvatzoglou M, Delso G, et al. Tissue classification as a potential approach for attenuation correction in whole-body PET/MRI: evaluation with PET/CT data. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2009;50(4):520-6. 23. Coombs BD, Szumowski J, Coshow W. Two-point Dixon technique for water- fat signal decomposition with B0 inhomogeneity correction. Magn Reson Med. 1997;38(6):884-9. 20 21 24. Goodsitt MM, Shenoy A, Shen J, et al. Evaluation of dual energy quantitative CT for determining the spatial distributions of red marrow and bone for dosimetry in internal emitter radiation therapy. Med Phys. 2014;41(5):051901. 25. Ricci C, Cova M, Kang YS, et al. Normal age-related patterns of cellular and fatty bone marrow distribution in the axial skeleton: MR imaging study. Radiology. 1990;177(1):83-8. 26. Basu S, Houseni M, Bural G, et al. Magnetic resonance imaging based bone marrow segmentation for quantitative calculation of pure red marrow metabolism using 2-deoxy-2-[F-18]fluoro-D-glucose-positron emission tomography: a novel application with significant implications for combined structure-function approach. Molecular imaging and biology : MIB : the official publication of the Academy of Molecular Imaging. 2007;9(6):361-5. 27. Drzezga A, Souvatzoglou M, Eiber M, et al. First clinical experience with integrated whole-body PET/MR: comparison to PET/CT in patients with oncologic diagnoses. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2012;53(6):845-55. 28. Li Q, Pan SN, Yin YM, et al. Normal cranial bone marrow MR imaging pattern with age-related ADC value distribution. European journal of radiology. 2011;80(2):471-7. 29. Nonomura Y, Yasumoto M, Yoshimura R, et al. Relationship between bone marrow cellularity and apparent diffusion coefficient. Journal of magnetic resonance imaging : JMRI. 2001;13(5):757-60. 30. Herneth AM, Friedrich K, Weidekamm C, et al. Diffusion weighted imaging of bone marrow pathologies. European journal of radiology. 2005;55(1):74-83. 21 22 31. Ishijima H, Ishizaka H, Horikoshi H, Sakurai M. Water fraction of lumbar vertebral bone marrow estimated from chemical shift misregistration on MR imaging: normal variations with age and sex. AJR American journal of roentgenology. 1996;167(2):355-8. 32. Roldan-Valadez E, Pina-Jimenez C, Favila R, Rios C. Gender and age groups interactions in the quantification of bone marrow fat content in lumbar spine using 3T MR spectroscopy: a multivariate analysis of covariance (Mancova). European journal of radiology. 2013;82(11):e697-702. 33. Bredella MA, Gill CM, Gerweck AV, et al. Ectopic and serum lipid levels are positively associated with bone marrow fat in obesity. Radiology. 2013;269(2):53441. 34. Baum T, Yap SP, Karampinos DC, et al. Does vertebral bone marrow fat content correlate with abdominal adipose tissue, lumbar spine bone mineral density, and blood biomarkers in women with type 2 diabetes mellitus? Journal of magnetic resonance imaging : JMRI. 2012;35(1):117-24. 35. Mauch P, Constine L, Greenberger J, et al. Hematopoietic stem cell compartment: acute and late effects of radiation therapy and chemotherapy. Int J Radiat Oncol Biol Phys. 1995;31(5):1319-39. 36. Rose BS, Liang Y, Lau SK, et al. Correlation between radiation dose to (1)(8)F-FDG-PET defined active bone marrow subregions and acute hematologic toxicity in cervical cancer patients treated with chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012;83(4):1185-91. 37. Hofmann M, Bezrukov I, Mantlik F, et al. MRI-based attenuation correction for whole-body PET/MRI: quantitative evaluation of segmentation- and atlas-based 22 23 methods. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2011;52(9):1392-9. 38. Berker Y, Franke J, Salomon A, et al. MRI-based attenuation correction for hybrid PET/MRI systems: a 4-class tissue segmentation technique using a combined ultrashort-echo-time/Dixon MRI sequence. Journal of nuclear medicine : official publication, Society of Nuclear Medicine. 2012;53(5):796-804. 23 24 Figure captions Figure 1 Age distribution Scatterplots showing the age distribution of the PET/MR patients evaluated in the study is shown separately for men and women. The majority of patients were over 30 years of age. Figure 2 Image series Typical image series used for data evaluation is shown. The data sat consists of fat and water MR images, ADC map and 18F-FDG-PET. The data series was obtained in a 17-year old male patient with germ cell tumor. Differences in FF and SUV can be observed between the proximal and the peripheral skeleton with a lower FF in the lumbar spine and the pelvis with correspondingly higher SUV and ADC as compared to the peripheral skeleton. Figure 3 Fat-water-flip Fat and water MR images obtained in a 45-year old female patient referred to imaging for cancer of unknown primary. The fat-water-flip which occurred in the upper thorax in this patient is marked by white arrows. To prevent errors in FF quantification of bone marrow, all Dixon images were visually checked for the presence of this artifact. Data sets with fat water flip (5 of 110) were excluded for evaluation. Figure 4 Bone marrow in proximal and peripheral skeleton Image series consisting of fat and water MR images, ADC map and 18F-FDG-PET obtained in a 64-year old female patient with breast cancer. In the peripheral skeleton (see humerus and femur), high FF with low 18F-FDG-uptake and low ADC of bone marrow is observed. In the proximal skeleton as represented by the visible portion of 24 25 the lumbar spine, the FF of bone marrow is lower with correspondingly higher ADC and 18F-FDG-uptake. Figure 5 Bone marrow activation Image series (fat and water MR images, ADC map and 18F-FDG-PET) obtained in a 54-year old female patient with malignant melanoma who had been referred to imaging for investigation of anemia. Intestinal metastasis was found in the small bowel with intermittent bleeding as explanation for the anemia. BM was highly activated as indicated by the high 18F-FDG uptake as visible in the lumbar spine and the right humerus (arrows). Fat content in the corresponding regions was reduced and ADC was elevated. Figure 6 Fat fraction, 18F-FDG uptake and ADC Box-plots for fat fraction (FFmean) (a), 18F-FDG uptake given by the SUVmean (b) and ADCmean (c) as assessed in the VOI analysis in the different regions are summarized. The boundaries of the boxplots indicate the 25th and 75th percentiles; the whiskers indicate the 90th and 10th percentiles. The line within each box indicates the median. The points represent outliers. The black points represent data from pediatric patients (< 15 years of age). 25 26 Tables Table 1 ADC Correlation of bone marrow fat fraction with 18F-FDG uptake and Skeletal region Correlation of FFmean and SUVmean r p value Correlation of FFmean and ADCmean r p value Humerus -0.61 < 0.0001* -0.62 < 0.0001* Thoracic spine -0.53 < 0.0001* -0.09 0.37 Lumbar spine -0.54 < 0.0001* -0.36 0.0005* Pelvis -0.73 < 0.0001* -0.34 0.0017* Femur -0.49 < 0.0001* -0.38 0.0006* Pearson correlation coefficients are given together with the p value. * significant; n.s.: not significant Summary of the region-based correlation of mean bone marrow (BM) fat fraction (FFmean) with metabolic activity as expressed by the mean standard uptake value (SUVmean) in 18F-FDG-PET and with the apparent diffusion coefficient (ADCmean). 26 27 Table 2a Comparison of regional mean fat fraction (FFmean) between male and female patients FFmean Humerus male female p value 95 [94-96] 90 [83-96] 0.098 Thoracic Spine 50 [46-55] 54 [50-57] 0.268 Lumbar Spine 60 [54-66] 64 [61-68] 0.245 Pelvis Femur 72 [68-77] 75 [71-78] 0.469 90 [87-93] 88 [86-90] 0.151 Fat fraction values are given in %. Values are given as mean values and 95 % confidence interval in brackets. Table 2b Comparison of regional SUVmean between male and female patients SUVmean male female p value Humerus Thoracic Spine 0.45 [0.38- 1.82 [1.660.51] 1.98] 0.58 [0.37- 1.73 [1.570.79] 1.88] 0.212 0.386 Lumbar Spine 1.52 [1.341.70] 1.49 [1.361.61] 0.767 Pelvis Femur 1.03 [0.90- 0.54 [0.461.17] 0.62] 0.96 [0.87- 0.58 [0.511.05] 0.64] 0.397 0.476 SUV are given as mean values and 95 % confidence interval in brackets. Fat fraction (FFmean) and metabolic activity (as represented by the SUVmean) of bone marrow in male and female patients were compared for each anatomical region using Student’s t-test. Bonferroni correction for multiple testing was performed. p values < 0.01 were considered statistically significant. 27 28 Table 3a Comparison of regional mean fat fraction (FFmean) between patients with and without chemotherapy (CTX) Humerus CTX 90 [83-98] Thoracic Spine 54 [50-59] no CTX p value 94 [92-96] 0.317 50 [46-54] 0.157 Lumbar Spine 66 [61-70] Pelvis Femur 76 [72-80] 89 [87-91] 59 [54-64] 0.039 72 [69-75] 0.106 89 [87-91] 0.674 Fat fraction values are given in %. Values are given as mean values with 95 % confidence interval in brackets. Table 3b Comparison of regional SUVmean between patients with and without chemotherapy (CTX) Humerus CTX no CTX p value Thoracic Spine 0.54 [0.44- 1.65 [1.490.64] 1.80] 0.49 [0.37- 1.88 [1.730.60] 2.04] 0.466 0.034 Lumbar Spine 1.42 [1.251.59] 1.59 [1.461.72] 0.118 Pelvis Femur 0.90 [0.79- 0.57 [0.491.01] 0.64] 1.09 [0.99- 0.57 [0.511.20] 0.63] 0.012 0.990 SUV are given as mean values with 95 % confidence interval in brackets. Fat fraction (FFmean) and metabolic activity (as represented by the SUVmean) of BM in patients with and without previous chemotherapy (CTX) were compared for each anatomical region using Student’s t-test. Bonferroni correction for multiple testing was performed. p values < 0.01 were considered statistically significant. 28