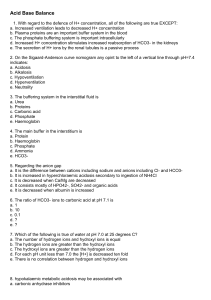
Acid Base Balance
advertisement
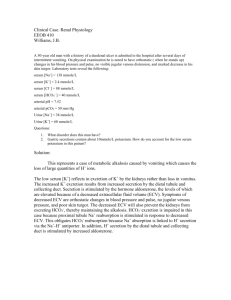
Acid Base Balance Learning Objectives: 1) Describe the components of normal daily acid-base balance (routes of H+ intake or production, and H+ utilization or excretion) a. Normal pH range of plasma is 7.38-7.42 i. Extremes compatible with life are pH 6.8-7.8 ii. The pH of body fluids is regulated by: 1. Buffering, changes in ventilation, and changes in renal handling of HCO3b. Buffer – solution containing a weak acid and it’s conjugate base i. The buffer pair present in highest concentration in the ECF is H2CO3 & HCO31. The lungs regulate PCO2 by changing ventilation 2. The kidneys regulate serum [HCO3-] c. H+ production & H+ utilization in normal metabolism i. Metabolic production of H+ 1. Methionine-SH + O2 2H+ + CO2 + SO4- + urea 2. Glucose lactic acid H+ + lactate (lactate is excreted in stool) ii. Metabolic utilization of H+ 1. Citrate + H+ citric acid + O2 CO2 +H2O iii. On a diet including red meat, H+ production exceeds utilization by 50 to 100 mEq/day 1. The kidney generates sufficient HCO3- to neutralize the H+ produced from metabolism d. Sites of HCO3- catabolism & generation i. H+ from metabolism (50-100 mE/day) reacts with HCO3- in ECF decreases ECF [HCO3-] CO2 is exhaled ii. Plasma HCO3- is freely filtered, but 99% is reabsorbed iii. The kidneys generate 50-100 mEq/day of new HCO3- to replace the HCO3- lost by reacting with H+ 2) Make a diagram showing the mechanism of HCO3- reabsorption in the renal proximal tubule a. H+ from inside the cell is transported into the urine by an H+, Na+ ANTIPORT (secondary active secretion) b. In the urine, H+ reacts with HCO3- to form H2CO3 c. H2CO3 is acted upon by CARBONIC ANHYDRASE to become water and CO2 d. CO2 passively diffuses back into the cell where it combines with water to become H2CO3 i. Reaction again catalyzed by carbonic anhydrase 3) List the fraction of the filtered load of HCO3- reabsorbed in different nephron segments a. Proximal tubule & thick ascending limb of loop = 95% i. Carbonic anhydrase in both luminal membrane and cytoplasm b. Collecting duct = 4-5% i. Carbonic anhydrase only in cytoplasm 4) Explain the role of carbonic anhydrase in renal HCO3- reabsorption and describe the effect on urine flow and Na+, K+, and HCO3- excretion of a drug that inhibits carbonic anhydrase a. Carbonic anhydrase catalyzes the reaction of H2CO3 H2O + CO2 b. Drugs that inhibit CA cause an osmotic diuresis i. These carbonic anhydrase inhibitors decrease the rate of reabsorption of HCO3- and Na+ which holds water in the urine causing the diuresis ii. This can induce metabolic acidosis by preventing CO2 reabsorption 5) Make a diagram showing the mechanism of renal HCO3- generation in relation to NH4+ secretion and titratable acid formation a. During acidosis, more glutamine is metabolized to buffer the blood with HCO3i. The main reaction for generating bicarbonate is the metabolism of glutamine which forms NH4+ which is excreted an α-KG-2 which reacts with 2H+ to yield glucose and CO2 1. This 2nd equation leads to the degeneration of H+ inside the cell which tells CA to breakdown more H2CO3 H+ + HCO32. This HCO3- created to buffer the blood is a ratio of 1:1 with the NH4 excreted in urine b. In titratable Acid Excretion, filtered HPO4-- reacts with secreted H+ H2PO4i. This H2PO4- is excreted (the kidney has secreted an acid to react with a phosphate) ii. At serum pH = 7.4, 80%of filtered phosphate is in the HPO4—form iii. For each H+ excreted with HPO4--, one HCO3- is added to renal venous blood iv. “Titratable acid” refers to the amount of H+ buffered by phosphate and other buffers in the urine 6) Describe the changes in tubular fluid Cl- and HCO3- concentrations as the urine flows along the proximal tubule a. Both are reabsorbed following Na+ reuptake and water osmosis 7) Compare the cellular mechanism of H+ secretion in the proximal tubule with the mechanism in the collecting duct a. H+ secretion in the proximal tubule is done using an H+, Na+ antiport b. H+ secretion in the collecting duct is done using an H+ ATPase & a H+, K+, ATPase i. Occurs in the intercalated cells in the collecting duct 8) Describe how acidosis or alkalosis affects renal tubular H+ secretion HEALTHY DIABETIC ACIDOSIS CHRONIC RENAL DISEASE NH4+ 30-50 300-500 0.5-15 Titratable acid 10-30 75-250 2-20 a. Chronic renal disease will thus create a metabolic acidosis because not enough HCO3- is being returned or generated to buffer the blood 9) Give the formula for calculating net acid excretion, and explain its significance with respect to HCO3- generation a. N.A.E. = rate of NH4+ excretion + rate of titratable acid (T.A.) excretion – rate of HCO3- excretion i. N.A.E. = (Urine NH4+)(V) + (T.A.)(V) – (Urine HCO3-)(V) b. The physiological significance of NAE is that it equals the net amount of new HCO3- generated by the kidney: i. For each NH4+ excreted, 1 new HCO3- is added to renal venous supply ii. For each H+ excreted combined with HPO4-- (this is T.A.), 1 HCO3- is added to renal venous supply iii. Subtracting the amount of HCO3- excreted gives the NET amount of new HCO3- added to the renal venous blood c. NEED TO KNOW EQUATION AND USE TO SOLVE PROBLEMS!!! d. Renal HCO3- generation maintains normal ECF [HCO3-] when HCO3- is lost from: i. Reaction with H+ produced from metabolism ii. The stool iii. The urine (at urine pH <6 there is very little HCO3- in the urine) 10) Describe the effect of a change in PCO2, or a decrease in blood volume, on renal HCO3- reabsorption a. Increasing H+ secretion increases HCO3- reabsorption i. H+ secretion is stimulated by: 1. Aldosterone, increased cell [H+], increased cell PCO2 ii. Increasing the [H+] gradient from cell to lumen increases H+ secretion 1. This effect occurs in all nephron segments that secrete H+ 2. Respiratory Acidosis increased PCO2 which increases cell PCO2 increased cellular [H+] a. Also, increased PaCO2 stimulates HCO3- reabsorption since CO2 participates in the mechanism of reabsorption b. Hypovolemia stimulates HCO3- reabsorption by increasing reabsorption of Na+ and HCO3- to help maintain ECF volume regardless of ECF pH 11) Describe the effect of increasing filtered load of HCO3- on HCO3- reabsorption and excretion a. Plasma [HCO3-] above normal leads to bicarbonaturia b. Normal plasma [HCO3-] is 24-26 c. Increasing the FF leads to an increase in Na+, HCO3-, and H20 reabsorption into peritubular capillaries Summary: 1) The kidneys generate 50-100 mEq/day of new HCO3- to replace the HCO3- lost by reaction with metabolic H+ 2) Plasma HCO3- is freely filtered; 99% is reabsorbed 3) HCO3- reabsorption is: a. Coupled to H+ secretion in proximal tubule, thick ascending loop of Henle, and the collecting duct b. Stimulated by increased PCO2 c. Increased in hypovolemia 4) HCO3- generation: a. DERVIES FROM GLUATMINE CATABOLISM b. Is stimulated by a high protein diet and acidosis