Clinical Case
advertisement
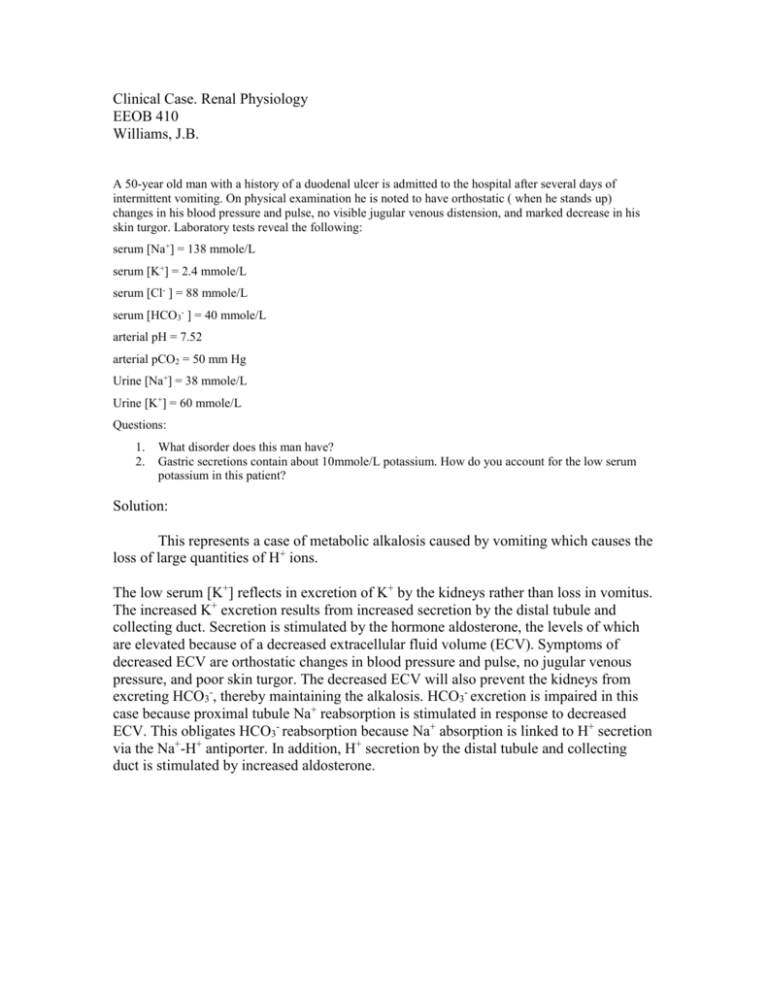
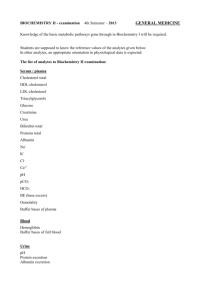
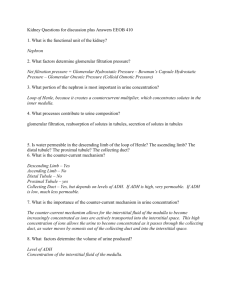
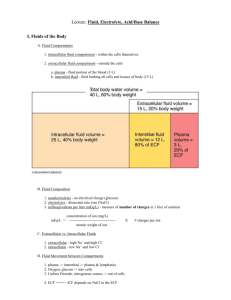
Clinical Case. Renal Physiology EEOB 410 Williams, J.B. A 50-year old man with a history of a duodenal ulcer is admitted to the hospital after several days of intermittent vomiting. On physical examination he is noted to have orthostatic ( when he stands up) changes in his blood pressure and pulse, no visible jugular venous distension, and marked decrease in his skin turgor. Laboratory tests reveal the following: serum [Na+] = 138 mmole/L serum [K+] = 2.4 mmole/L serum [Cl- ] = 88 mmole/L serum [HCO3- ] = 40 mmole/L arterial pH = 7.52 arterial pCO2 = 50 mm Hg Urine [Na+] = 38 mmole/L Urine [K+] = 60 mmole/L Questions: 1. 2. What disorder does this man have? Gastric secretions contain about 10mmole/L potassium. How do you account for the low serum potassium in this patient? Solution: This represents a case of metabolic alkalosis caused by vomiting which causes the loss of large quantities of H+ ions. The low serum [K+] reflects in excretion of K+ by the kidneys rather than loss in vomitus. The increased K+ excretion results from increased secretion by the distal tubule and collecting duct. Secretion is stimulated by the hormone aldosterone, the levels of which are elevated because of a decreased extracellular fluid volume (ECV). Symptoms of decreased ECV are orthostatic changes in blood pressure and pulse, no jugular venous pressure, and poor skin turgor. The decreased ECV will also prevent the kidneys from excreting HCO3-, thereby maintaining the alkalosis. HCO3- excretion is impaired in this case because proximal tubule Na+ reabsorption is stimulated in response to decreased ECV. This obligates HCO3- reabsorption because Na+ absorption is linked to H+ secretion via the Na+-H+ antiporter. In addition, H+ secretion by the distal tubule and collecting duct is stimulated by increased aldosterone.