Provider Manual Attachment 10.1.3, Prior Authorization Criteria for
advertisement
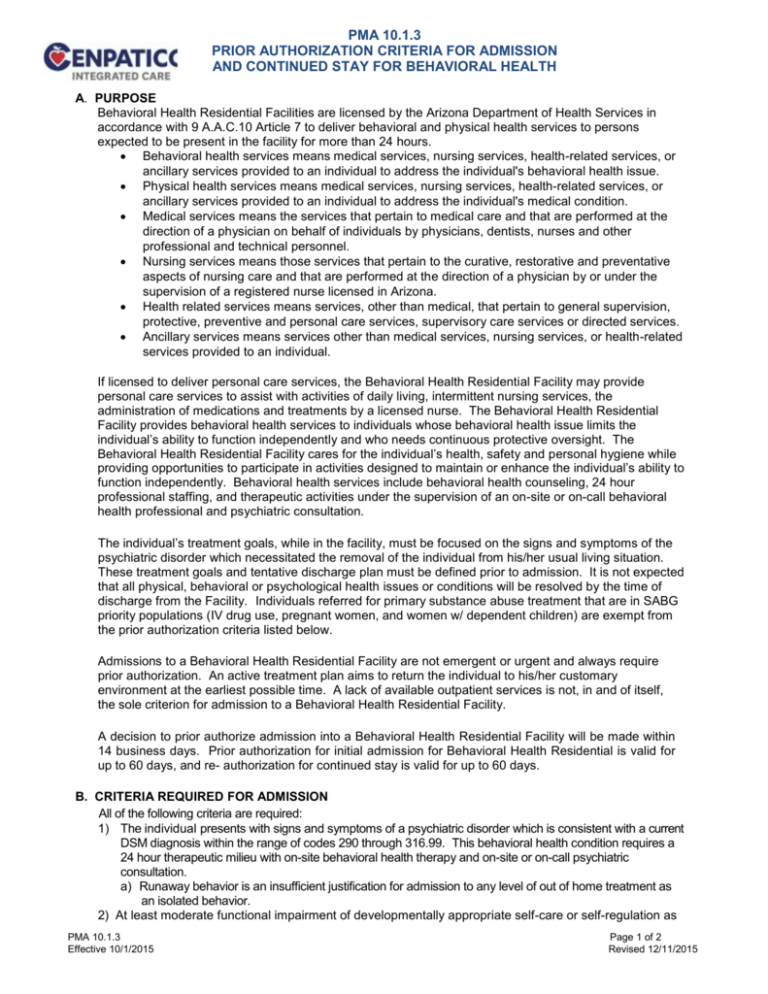
PMA 10.1.3 PRIOR AUTHORIZATION CRITERIA FOR ADMISSION AND CONTINUED STAY FOR BEHAVIORAL HEALTH A. PURPOSE Behavioral Health Residential Facilities are licensed by the Arizona Department of Health Services in accordance with 9 A.A.C.10 Article 7 to deliver behavioral and physical health services to persons expected to be present in the facility for more than 24 hours. Behavioral health services means medical services, nursing services, health-related services, or ancillary services provided to an individual to address the individual's behavioral health issue. Physical health services means medical services, nursing services, health-related services, or ancillary services provided to an individual to address the individual's medical condition. Medical services means the services that pertain to medical care and that are performed at the direction of a physician on behalf of individuals by physicians, dentists, nurses and other professional and technical personnel. Nursing services means those services that pertain to the curative, restorative and preventative aspects of nursing care and that are performed at the direction of a physician by or under the supervision of a registered nurse licensed in Arizona. Health related services means services, other than medical, that pertain to general supervision, protective, preventive and personal care services, supervisory care services or directed services. Ancillary services means services other than medical services, nursing services, or health-related services provided to an individual. If licensed to deliver personal care services, the Behavioral Health Residential Facility may provide personal care services to assist with activities of daily living, intermittent nursing services, the administration of medications and treatments by a licensed nurse. The Behavioral Health Residential Facility provides behavioral health services to individuals whose behavioral health issue limits the individual’s ability to function independently and who needs continuous protective oversight. The Behavioral Health Residential Facility cares for the individual’s health, safety and personal hygiene while providing opportunities to participate in activities designed to maintain or enhance the individual’s ability to function independently. Behavioral health services include behavioral health counseling, 24 hour professional staffing, and therapeutic activities under the supervision of an on-site or on-call behavioral health professional and psychiatric consultation. The individual’s treatment goals, while in the facility, must be focused on the signs and symptoms of the psychiatric disorder which necessitated the removal of the individual from his/her usual living situation. These treatment goals and tentative discharge plan must be defined prior to admission. It is not expected that all physical, behavioral or psychological health issues or conditions will be resolved by the time of discharge from the Facility. Individuals referred for primary substance abuse treatment that are in SABG priority populations (IV drug use, pregnant women, and women w/ dependent children) are exempt from the prior authorization criteria listed below. Admissions to a Behavioral Health Residential Facility are not emergent or urgent and always require prior authorization. An active treatment plan aims to return the individual to his/her customary environment at the earliest possible time. A lack of available outpatient services is not, in and of itself, the sole criterion for admission to a Behavioral Health Residential Facility. A decision to prior authorize admission into a Behavioral Health Residential Facility will be made within 14 business days. Prior authorization for initial admission for Behavioral Health Residential is valid for up to 60 days, and re- authorization for continued stay is valid for up to 60 days. B. CRITERIA REQUIRED FOR ADMISSION All of the following criteria are required: 1) The individual presents with signs and symptoms of a psychiatric disorder which is consistent with a current DSM diagnosis within the range of codes 290 through 316.99. This behavioral health condition requires a 24 hour therapeutic milieu with on-site behavioral health therapy and on-site or on-call psychiatric consultation. a) Runaway behavior is an insufficient justification for admission to any level of out of home treatment as an isolated behavior. 2) At least moderate functional impairment of developmentally appropriate self-care or self-regulation as PMA 10.1.3 Effective 10/1/2015 Page 1 of 2 Revised 12/11/2015 3) 4) 5) 6) 7) evidenced by: a. D ocumentation of recent occurrence(s) of suicidal/homicidal ideation without plan or intent, and the inability of the individual and support system to carry out a safety plan; or b. D ocumentation of disturbance of mood thought or behavior that clearly impair daily functioning, persist in the absence of stressors, and impair recovery from the presenting problem. Any present medical condition can be safely managed within the Behavioral Health Residential setting. Medically necessary outpatient behavioral health services do not meet the treatment needs of the individual and there is documentation of a failure to respond or an inability to be safely managed in a less restrictive level of care. The medically necessary behavioral health treatment can be properly provided within a Behavioral Health Residential setting. The admission is not used primarily and therefore clinically inappropriately as: a) An alternative to detention, incarceration or as a means to ensure community safety in an individual exhibiting primarily delinquent/antisocial behavior; or b) The equivalent of safe housing, permanent placement, or c) An alternative to parents’/guardians’ or other agencies’ capacity to provide for the individual, or d) A behavioral health intervention when other less restrictive alternatives are available and meet the individual’s treatment needs. A preliminary discharge plan of aftercare services and supports has been developed and presented with the request for prior authorization. C. CONTINUED STAY CRITERIA There is documented evidence of all of the following: 1) Active treatment, only available at this level of care, is being provided by the facility on a 24 hour basis with direct supervision/oversight by professional behavioral health staff; and 2) The treatment is reducing the severity of the behavioral health issue that was identified as the reason for admission; and 3) The Child and Family Team or Adult Clinical Team has met every 4 weeks or more frequently, if clinically indicated, to review progress and revise the service plan to address any lack of progress; and 4) There is an expectation that continued treatment can reasonably be expected to improve or stabilize the individual’s condition so that this type of service will no longer be needed. D. DISCHARGE CRITERIA To be considered for discharge from a Behavioral Health Residential Facility the following criteria are met: 1) There is a written plan with specific discharge criteria, written as behaviorally measurable goals. 2) There is documentation that the Child and Family Team or Adult Clinical Team is involved in the writing of the discharge plan. 3) The plan complies with current standards for medically necessary covered behavioral health services, cost effectiveness, and least restrictive environment and is in conformation with federal and state clinical practice guidelines. 4) The individual’s treatment plan goals as identified at admission to this level of care have been accomplished; OR the individual is not making progress toward treatment goals and there is no reasonable expectation of progress at this level of care. PMA 10.1.3 Page 2 of 2