Dizziness > 2 weeks
advertisement

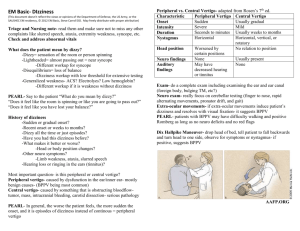
Dizziness Your capsule coffee is a little weak after the morning’s efforts but time seemed a little precious to justify a barista run. Turns out Mrs DZ doesn’t speak a word of English. You have proudly mastered two phrases in Arabic ل ل ترح يب ه تافand ت تأل م؟ هل. You try out the first which results in a hopeful smile but any further attempts at verbal communication are met with a blank stare. Fortunately Mrs Zs daughter appears through the curtain and can translate. Mrs Z had been brought in by ambulance 70 minutes ago and has already been through the Early Assessment Pod. Colleagues have spoken to the ambulance officers and daughter and noted that the dizziness had developed the previous afternoon. Notes: 68F Onset of dizziness while hanging out washing yesterday PM ++. ?spinning. Nauseated this morning. No chest pains, fever or headache. Hx HT, TAH, PAF, Thyroid, Anxiety. Aspirin, Mirtazapine, Thyroxine, Rosuvastatin, Irbesartan, Lercanidipine. Exam: Pupils normal, no facial droop, symmetrical power. Vital signs were within normal limits. Sao2 98% (air). ECG - has been autographed. It shows AF and there are no evidence of acute ischaemia. CT Brain. FBE, UECr, LFT, Troponin I, CRP TSH. Medication Chart: 12.5mg Prochlorperazine IM (given 15 minutes ago). She has a 20G IV cannula in her L) hand. Provisional diagnosis – Vertigo? Plan – Trial Stemetil? SSU Realising this case may need a lot more sorting out than first thought you regret opting for that namby pamby capsule coffee. The quick win scenario is when you can quickly confirm a history of true vertigo, exclude a central cause with a quick examination and get her admitted to SSU and off your screen. You remember Drs Lee and Cheng extolling the virtues of the HINTS exam and it all seemed so clear then but you’ve only performed this test on a real patient twice. Is this really necessary? You sneak a quick glance at James Hayes’ clinical resource on vertigo to brush up before performing this act of clinical wizardry on Mrs Z but scrolling down the guideline you are reminded that in a patient over 60 a whole raft of processes enter the list of possible aetiologies. You’re not sure whether to go back to the beginning. Where is House when you need him? Then the flow coordinator pages you to enquire if you have completed the SSU referral yet...apparently the next bus is coming in and Mrs Zs bed is needed pronto...$%#@&&..!! Time is precious but this is another situation where following the shortest route may lead to some thorny bushes...especially in older patients…where do you start? There are two questions to answer: 1. Is this true vertigo? 2. If so is it peripheral or central? Dizziness The below table should help with question 1. Category Vertigo = spinning sensation = disorientation in space pathophysiology Peripheral Central Presyncope =fainting sensation Reduced cerebral perfusion dysequilibrium Gait disorder Light-headedness = disconnection from environment Psychological Psychoactive drugs/ medication aetiology Labyrinthitis Vestibular Neuronitis Meniere’s Otitis Media Benign Positional vertigo (BPV) Trauma Acoustic neuroma Foreign body in ear canal Posterior circulation CVA/ TIA Infection Vertebral basilar insufficiency Vertebrobasilar migraine Posttraumatic (temporal #) Temporal lobe epilepsy Tumours Multiple sclerosis Subclavian Steal Cervical spine dysfunction Neurally mediated Orthostatic sepsis cardiac Myelopathy Neuropathy Parkinsonism TIA/ CVA Anxiety/ depression drugs Differentiating the presence of true vertigo is usually possible by asking whether there is a spinning sensation. If positive ask about focal weakness and sensory changes. If vertigo is confirmed then you need to address question 2: It is critical to also enquire about possible ataxia and instability which are more suggestive of a central process. Vertigo which occurs in any positon rather than only with particular movements is also more suggestive of a central process. Peripheral causes of vertigo do not affect alertness and cognition. The common causes are BPV, neuronitis and viral labyrinthitis. With labyrinthitis the whole of the inner ear is involved leading to hearing deficits and possibly tinnitus. Drugs are important: Aminoglycosides, anticonvulsants and tetracyclines are directly vestibulotoxic. Alcohol use can lead to cerebellar syndrome with resultant disequilibrium. Dizziness A history suggestive of vertigo allows you to short cut to your neurological exam including the Hallpike manoeuvre12 and HINTS if you are confident in their execution. A neurological exam looking for other focal signs to suggest a central lesion. Careful examination of pupils and eye movements is critical. HINTs comprises Head Impulse, examination for multidirectional Nystagmus and Test for Skew. The best way to learn this is to observe and be coached by an expert who can verify your findings. The next best option and a good starting point is to listen to EMCrit Podcast 33 - Posterior stroke. http://emcrit.org/podcasts/posterior-stroke/ (cited April 2014). There are links on the site to video demonstrations of this technique by neurologist Dr David Newman-Toker. Also worth checking out is this discussion on HINTS: Radecki R. HINTS vs ABCD2 in dizziness. http://www.emlitofnote.com/2013/11/hints-vsabcd2-in-dizziness.html This reminds us of some of the limitations of HINTS. This a great test and a validation study in the research setting showed excellent sensitivity and specificity but was conducted on a high risk cohort of patients (high pre-teat probability) using 2 experienced expert examiners. Be aware that the accuracy of your less experienced examination is likely less reliable. It has been noted that novices tend to overcall positive head impulse tests (which then leads to a falsely negative HINTs exam and potentially missed central causes). Rotational and vertical nystagmus and nystagmus that changes in direction with position are rarely due to peripheral causes. If there has been sudden onset of vertigo with associated ataxia or other symptoms or signs suggestive of posterior circulation event that day then a code stroke should be paged and the acute stroke process followed. Investigation: Not all patients with vertigo need imaging. CT with angiogram and MRI should be arranged if there is any suggestion of a central cause. MRI is more useful if neoplasia (including acoustic neuroma) and Multiple Sclerosis is considered. CT angiography may be preferable for acute CVA or TIA. Both are useful for vertebral Basilar Insufficiency. Imaging should be considered for all elderly patients or those at high risk for cerebrovascular disease. Non vertiginous Dizziness: If vertigo is not really apparent then the history and examination needs to expand to further define the symptoms and consider the long list of possible causes. History: Time course, precipitants and duration (if intermittent) Seek causes of primary autonomic failure (dementia/ multiple system atrophy) and secondary autonomic failure (diabetes/HIV neuropathy ). Drugs - new or adjusted doses of antihypertensives, diuretics and antidepressants are common culprits leading to hypovolaemia or orthostatic hypotension. 1 2 www.bmj.com/content/339/bmj.b3493.full Waterson J. Dizziness: How to Treat. Australian Doctor, 7 March 2003;106:484-5 Dizziness Cardiac - Patients may not be aware of palpitations suggesting arrhythmias. Examine for signs suggestive of structural heart abnormalities including cardiomyopathy, valvular and pericardial disease. Ask about chest pain, syncope and exertional dyspnoea. Respiratory – Risk factors for Pulmonary Embolus. Examination: Vital signs and conscious state. Check for delirium Look for anaemia, dehydration. Examine for murmurs and carotid bruits. In younger patients try a Valsalva manoeuvre listening for the systolic murmur of HOCM. Further examination is guided by the history but should be thorough and include a diligent neurological exam. Bedside Tests: BSL. Look closely at the ECG for: AF prolonged QT interval (>500ms) Bradycardia/ pauses on rhythm strips/ monitor review. Brugada (J point ST elevation V1-3 and R) BBB. WPW (short PR and delta waves. AV blocks RV dysplasia R) BBB with QRS>110ms in V1, epsilon waves in V1-2 and T-wave inversion in R) precordia leads. Urinalysis – infection? Pathology: Add magnesium to requests for electrolyte levels. Troponins may be elevated but be mindful any elevation is likely to represent a non-occlusive AMI I the absence of chest pain or a STEMI pattern on ECG. D Dimer may be helpful if there are genuine risk factors for or signs of PE. Patients on Digoxin need a digoxin level. CT should not be ordered routinely but considered if there is a possibility of trauma. Any head strike in a patient on antiplatelet agents or anticoagulants requires a CT head. Case resolution: You decide to take a more detailed history and determine there have been intermittent episodes of dizziness over the last 2 months and two episodes of syncope in the last three weeks. These were brief (<30 seconds) and occurred at rest. There was no warning, seizure activity or apparent focal weakness. Recover was rapid. There was no clear change with posture. A visit to the LMO had led to adjusted antihypertensive medications and advice to come to hospital if it recurred. Social history Dizziness reveals an active married grandmother who takes care of four active young grandchildren after school during the week. Non-smoker. No alcohol. Examination: HR 88 irregular. Afebrile, BP 130/90 lying, 125/80 sitting. RR 16. Well hydrated JVP approx. 4cm. Apex beat displaced to LSE. Ejection murmur radiating to carotids but there is no enhancement with a Valsalva. Soft bibasal crepitations. Respiratory and gastrointestinal exam - unremarkable. Neurological exam – Slight slow nystagmus on extreme L) lateral gaze Gait apprehensive but steady. Nil other focal findings No apparent change in affect. Pathology results and CT head are unremarkable and you review Mrs Z to relay these findings and a suggestion that outpatient halter monitoring and echocardiogram are indicated. Mrs Z and her daughter are unhappy with this and feel there is something serious wrong. She is monitored in SSU that night and has two further negative troponins. Early the next morning she has a number of sustained runs of bradycardia and a 16 seconds of ventricular standstill. Cardiology admit her the next day for an echocardiogram (hyperdynamic systolic function only). They request an MRI and MRA head which is normal and plan to insert a dual chamber pacemaker the next day. The discharge diagnosis is an uncommon but important cause of non-vertiginous cause of dizziness - Arrhythmia. You realises your decision to admit to SSU was really based on a combination of story of syncope and the family’s concern. Anonymously chuffed you start explaining to the consultant your need for lunch when the ANUM wanders past a mentions something about a hypotensive young lady just about to be wheeled in to resus 2… She looks at you expectantly…





![OS 211 Lecture 21: Dizziness OS 211 [A]: Integration, Coordination](http://s3.studylib.net/store/data/007102827_1-16ddcae12e086824a7614c4bf8633097-300x300.png)