OS 211 Lecture 21: Dizziness OS 211 [A]: Integration, Coordination
![OS 211 Lecture 21: Dizziness OS 211 [A]: Integration, Coordination](http://s3.studylib.net/store/data/007102827_1-16ddcae12e086824a7614c4bf8633097-768x994.png)
OS 211 [A]: Integration, Coordination and Behavior
Lec 21: Dizziness
Dr. Jose Leonardo R. Pascual
TOPIC OUTLINE
I. Introduction of Dizziness
II. Differentials for Dizziness
III. Vestibulo-ocular Reflex (VOR)
IV. Approach to Dizziness
V. Common Dizziness Syndrome
VI. Potentially Life-Threatening Causes of Vertigo
VII. Management of Dizziness
VIII. Summary
Learning Objectives:
1. Be aware of the different meanings of dizziness
2. Differentiate between vertigo versus non-vertiginous dizziness
3. Differentiate between peripheral and central causes of vertigo
4. Know the physical examination techniques to localize vertigo
5. Manage common dizziness disorders cost-effectively
We tried following sir’s flow of the lecture but for some parts, we combined those that we can since sometimes, sir jumped from one topic to another. We also removed those that were not discussed.
I .
INTRODUCTION OF DIZZINESS
“Dizziness covers anything from severe aural vertigo to a housewife feeling nervous in the supermarket.”
– Henry George Miller, 1968
Dizziness is one of the most common complaints bringing patients to your clinic o 5% of walk-in clinic patients o 4% of ER consults
Depending on where you’re thrown, it could be said in different ways: nalulula lilong-lilong lipong ribong-ribong maalindadaw
目眩 xuan yun 眩的
A very subjective complaint and can mean anything to the patient: o headache o light-headedness – floating sensation o vertigo (true dizziness) –spinning sensation o unsteadiness - neurologic, or ataxia
2016: Most causes are benign
Up to 30% of consults for dizziness are due to serious conditions (a.k.a. matter of life and death) such as: o stroke o transient ischemic attacks o cardiac arrhythmias o acute infections o anemia
II. DIFFERENTIALS FOR DIZZINESS
Good history taking entails asking the right questions. o “Does the room spin ?” o “Do you feel unsteady
?” o “Are you feeling lightheaded
?”
BEST QUESTION: “what do you mean by dizzy?”
Don’t ask leading questions and put any words in the patient’s mouth as this may lead to mismanagement.
What do you mean by dizzy?
Table 1. Differential Diagnosis for Dizziness
“I might faint”
“I’m giddy”
“I’m light-headed”
“I might fall”
Syncope/ near syncope
Disequilibrium
Cardiogenic
Neurologic
( Sense of poor equilibrium)
“I’m tilting or rocking”
“The room is spinning”
“I’m just dizzy”
(
True vertigo
Sense of spinning)
Ill-defined
(difficult patient)
Vestibular
Psychogenic/ psychiatric
A. SYNCOPE/ NEAR SYNCOPE
I might faint. I’m giddy. I’m light-headed.
Light-headedness o Feeling of impending loss of consciousness or about to pass out o May be due to a psychological condition ( anxiety or stress )
Gienah, AJ, Irene
1
December 9, 2013 o Patient may report to you some form of palpitation which confirms an anxious state or a cardiac condition o Ask yourself the right questions like what are the possible things that could cause light headedness?
Low blood pressure
Low blood sugar
Tilt Table Test
– test the cardiologist may order to confirm lightheadedness o Patient is tilt in varying degrees to see what elevation will cause light-headedness o Confirms the presence of light headedness that is due to a cardiac condition
Figure 1. Tilt Table Test
Overall, etiology points to a cardiovascular problem (Orthostatic hypotention, cardiac arrythmia, hypersensitive carotid sinus, vasodepressor spells/ vasovagal syncope, valvular or subvalvular aortic stenosis) or any form of strain like coughing, anything that could diminish blood flow to the brain, arrhythmia, medications, hyperventilation which induce vasoconstriction in the brain, hypoglycemia
Differential Diagnoses of Light-Headedness
Systemic Disorders
Cardiovascular presyncope o hypovolemia o postural hypotension o vasovagal o carotid sinus o postmicturition o posttussive o vasodilators o ANS dysfunction o Addison’s disease o brady/tachyarrhytmias o heart block o congestive heart failure o valvular heart disease
Medications
Hyperventilation
COPD
Infection
Hypoglycemia
Hyperglycemia o anemia o alcohol o street drugs
Ophthalmological disorders o glaucoma o lens implant o refractive errors o new prescription lenses o acute ocular muscle paralysis
B. DYSEQUILIBRIUM
I might fall.
Subjective feeling of pseudodrunkenness or unsure footing when walking/ambulating
Non-vestibular neurologic disorder / brain problem
Patients who complaint that they might fall, some form of imbalance
This can be due to anything outside the inner ear or the vestibular apparatus o Headache, migraine, sinusitis, post-traumatic concussion, seizure, degenerative disorders, peripheral disorders like diabetes, paraneoplastic cerebellar syndrome
Differential Diagnoses of Disequilibrium
Headache o sinus o muscle contraction
Complex partial seizures
Dementia
Peripheral neuropathy
Page 1 / 9
o migraine
Concussion (due to trauma)
Paraneoplastic cerebellar dysfunction
C. ILL-DEFINED LIGHT-HEADEDNESS
I’m just dizzy.
“Spacey” or “disconnected” dizziness without any feeling of motion or loss of balance
Patients who cannot describe what they mean by dizzy
Psychiatric mainly anxiety states
Differential Diagnoses of Ill-Defined Light-Headedness
Anxiety
Panic attacks
Depression
Psychogenic seizure (or even pseudo-seizure)
Conversion reaction
Malingering
D. TRUE VERTIGO
I’m tilting or rocking. The room is spinning.
Defined as a false sense of motion , either of self or the surroundings
Vestibular problem which can be central or peripheral o Peripheral
– anything outside the CNS beginning from the nucleus of CN VIII all the way to its peripheral nerve into the inner ear
ENT further subcategorize as cochlear or retrocochlear
Cochlear – lesion in the inner ear & labyrinth
Retrocochlear – lesion in CN VIII
Figure 2. Classification of
True Vertigo
Worsened by motion
Represents either physiologic stimulation or pathologic dysfunction in any of the 3 systems subserving spatial orientation and posture: the vestibular system , visual system , or somatosensory system
Lecture 21: Dizziness OS 211
Can be due to some form of middle ear problems like perforated ear drums later becoming granulomas eating the mastoid process
Can even have a stroke in the inner ear because the labyrinthine artery is a branch of AICA
Can be due to any problem that interfere with the electrolytes (mainly potassium) of the inner ear like
As a rule, consider peripheral vestibulopathy (cochlear lesions) in all episodes of vertigo NOT accompanied by neurologic symptoms
CN VI is important in peripheral vertigo because it is controlled by CN
VIII
Causes of Peripheral Vertigo
Middle ear lesions o Infections
Viral
Bacterial o Otosclerosis o Cholesteatomas o Tumors
Glomus tympanicum/jugulare
Squamous cell CA
Inner ear lesions (most common) o Benign positional vertigo* o Vestibular neuronitis* o Ménière’s disease* o Labyrinthitis
Infection or autoimmune o Vascular disorders
Vertebrobasilar insufficiency
Hemorrhage (rare)
Labyrinthine artery
Bleeding diathesis o Systemic disorders
Diabetes
Uremia o Trauma
Perilymph fistula o Ototoxins
Alcohol
Salicylates
Anti-epileptics
Aminoglycosides
Loop diuretics
Cinchona alkaloids (quinidine, quinine)
Heavy metals (cisplatin)
Retrocochlear
(CN VIII) lesions o Infection o Collagen vascular disease o Tumor
Schwannom a
Neurofibrom a
Meningioma
Metastasis
(Rare)
Figure 4. Big Circle (CNS) : vestibular nuclei, cerebellum, vestibulospinal tract, MLF, cranial nerve 3, 4, 6, cerebral cortex. Small
Circle (PNS) : ear, labyrinth, cranial nerve 8
Central Vertigo
Simply any disconnections in the central pathways involved in balance and spatial orientation
The central vestibular system includes the EOM cranial nerves , cerebellum and vestibular nuclei o EOM cranial nerves ensure that the visual image that falls on the retina remains focused, regardless of head position (vestibuloocular reflex) o Supranuclear connection from the cerebellum integrates signal o Vestibular nuclei are found in the medulla and acts on muscles to control posture
Figure 3. The Vestibular Apparatus
Peripheral Vertigo
Involve the nerve (CNVIII up to its nucleus in the brainstem)
Gienah, AJ, Irene Page 2 / 9
Lecture 21: Dizziness OS 211
Figure 7. Recall: Supranuclear connection from the cerebellum integrates signal. Vestibular nuclei are found in the medulla and acts on muscles to control posture.
VOR or Doll’s Eye Reflex
Doll’s Eye Sign
A test used to evaluate a patient’s VOR (especially a patient in coma)
Complex partial seizures
Demyelinating diseases o Multiple sclerosis
Trauma
Hereditary disorders o Friedreich’s ataxia o Refsum’s diseas e atrophy
Figure 5. The Central Vestibular Systems
Causes of Central Vertigo
Metabolic disorders o Alcohol cerebellar degeneration
Infection o Meningitis o Encephalitis
Developmental disorders o Malformations of the inner ear o Craniocervial junction malformation o Arnold-Chiari malformation
Downward displacement of the cerebellar tonsils through the foramen magnum, with concomitant hydrocephalus o O l ivopontocerebellar
III. VESTIBULO-OCULAR REFLEX (VOR)
A. INTRODUCTION
Figure 4 . Testing for Doll’s Eye Sign
PROCEDURE
1) Hold the patient’s upper eyelids open.
2) Quickly turn his head from side-to-side and note eye movements with each turn.
RESULTS
(+) patient’s eyes move to the opposite direction
( –) patient’s eyes remain fixed in midposition
The absence of this reflex means there is something wrong with the verstibular apparatus applicable to both peripheral and central vertigo
B. HOW IT WORKS
For example when turning your head to the right , the movement causes perilymph in the R horizontal semicircular canal to move to the left, causing hair cells to detect movement. turning head to the R activates R horizontal SC turning head to the L activates L horizontal
SC
Figure 6. Recall: Cranial Nerves to the EOM ensure that the visual image that falls on the retina remains focused, regardless of head position (VOR)
Gienah, AJ, Irene
Signals are sent via R vestibular nerve (CN VIII) to the R vestibular nuclei in the medulla.
The R vestibular nucleus (CN VIII) activates the L abducens nucleus (CN VI)
The L abducens nerve (CN VI) activates the lateral rectus of the L eye.
The R oculomotor nerve (CN III) is yoked by the MLF to the abducens nerve (CN VI).
Another nerve tract projects also from the L abducens nucleus by the medial longitudinal fasciculus to the R oculomotor nuclei , activating the medial rectus of the R eye .
Both eyes look to the left.
Page 3 / 9
Figure 8. VOR events when the head is turned to the right.
Turning your head to the right while your head is bent backward
R posterior canal is activated
Eyes look down and to the left
Turning your head to the right
R horizontal canal is activated
Eyes look to the left
Turning your head to right while your head is bent forward
R superior canal is activated
Eyes look up and to the left
Table 2 and Figure 9. Activation of the various semi-circular canals
Figure 10. Endolymph movement stimulates hair cells to detect direction of head movement
What happens when we move our heads? o The vestibular apparatus and nerve tells us where our head is going o The eyes drift as a result of stimulation of the contralateral
CN VI ( slow component ) o The contralateral frontal eye field quickly returns the eyes to midline position ( fast component = “ saccade ”)
Gienah, AJ, Irene
Lecture 21: Dizziness OS 211 o But the accuracy of returning eyes to the midline is controlled by the cerebellum
C. CEREBELLUM
Role of cerebellum: o Adjust your arms and legs to maintain steady upright position o Adjust your eyeballs to where you are in space.
IV. APPROACH TO DIZZINESS
Demonstration: Val pushes Mike .
Mike assumes the anti-gravity posture (elbows and knees bent, one leg forward) so he won’t tumble down.
This also demonstrates how the anti-gravity muscles – thighs, shoulders and trunk are important in upright posture.
Trying to be steady will be harder with eyes closed because the eyeballs will tell one where he is in space.
A. STEP 1: VERTIGINOUS OR NON- VERTIGIOUS
Is it vertiginous or non-vertiginous dizziness?
A good history can elucidate what exactly is the etiology of the patient’s dizziness.
Table 3. Vertiginous vs. Non-vertiginous Dizziness
Vertigo o sense of rotation of either the patient or his environment o sense of imbalance/disequilibrium in the head
(not the feet)
Unsteadiness due to
Cerebellar/
Proprioception
Deficits
Non-Vertiginous
Dizziness o ataxia/ sense of imbalance in the limbs or body o posterior column or cerebellar problem
Vague Dizziness o feeling of impending loss of consciousness (presyncope) o “light-headedness”, “fear of falling”, “swimming sensation” o psychological, emotional disturbance
Table 4. Differentiating Vestibular and Nonvestibular Dizzines
s
Property
Description
Time Course episodic or constant
Associated
Symptoms
Predisposing
Factors
Precipitating
Factors
Vestibular Dizziness spinning, whirling, rotating, off-balance nausea, vomiting pallor diaphoresis hearing loss, tinnitus congenital inner ear anomaly ototoxins ear surgery
Any head/body position changes ear infection or trauma
Nonvestibular
Dizziness light-headed, faint, dazed, floating episodic or constant paresthesias palpitations headache syncope syncope due to CVS disease psychiatric illness body position changes stress, fear, anxiety
hyperventilation
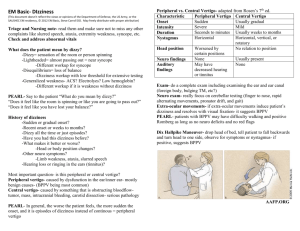
B. STEP 2: CENTRAL OR PERIPHERAL VERTIGO
Peripheral vs. Central Vertigo
There are several clues in the history that point to peripheral vertigo versus central vertigo o History of ear discharge or infection o Hearing loss and tinnitus o Intake of ototoxic medication o Sudden onset (e.g., due to stroke) o Absence of neurologic deficits
Table 5. Differentiating Peripheral and Central Dizziness.
Peripheral Vertigo Central Vertigo
Onset
Quality
Intensity
Occurrence
Duration sudden spinning, rotating severe episodic seconds, minutes, insidious disequilibrium mild to moderate constant weeks or longer
Page 4 / 9
hours, days
Exacerbation by
Head Movement
Nausea & Vomiting
Imbalance
Ear Pressure/Pain
Hearing Loss moderate to severe severe mild occasional frequent
Tinnitus frequent
Neurologic
Symptoms rare
*Central Vertigo – symptoms of imbalance mild mild moderate
None rare rare frequent
Differentiating Central from Peripheral Vertigo: Ototoxic
Examination
Check the ears. If there is a problem in the ears (e.g. perforation or swelling of the eardrums), it usually indicates a vestibular or peripheral origin
Differentiating Central from Peripheral Vertigo: Focused Neurologic
Examination
Watch out for deterioration of sensorium o CNS infection o Space-occupying lesions (brain tumors) o Encephalopathies (toxic /metabolic)
A. CRANIAL NERVE EXAMINATION
Possible findings o Anisocoria (pupils of different size) , papilledema (swollen, indicates high intracranial pressure)
Make sure to check pupils and perform a fundoscopy o Vertical diplopia
Indicates a lesion in the brainstem; a red flag!
Can be an interruption of MLF o Abnormalities of smooth pursuit
Tested by instructing the patient to follow your fingers with his eyes
Indicates a lesion in the cerebellum o Dysmetria of saccadic eye movements (overshooting of fingers or eyes) o Pathologic nystagmus (lesion in the cerebellum, brainstem) o Sluggish corneal reflex o Facial paralysis o Hearing loss/lateralization CN VIII
Indicates an ear problem o Impaired gag reflex o Tongue deviation
B. MOTOR EXAMINATION
Possible findings o Tremors o Carpopedal spasm after hyperventilation and turning pale
Young individuals may have carpopedal spasms (toes & fingers stiffen, become cupped) due to nervousness such that it looks like they’re going to pass out
Muscle atrophy
Muscle fasciculations
Hypotonia
C. CEREBELLAR TESTTING
Possible findings o Limb ataxia o Truncal ataxia o Gait ataxia o Remember to ask the patient to sit up/get up from bed and walk, even if they’re dizzy. You can’t check for ataxia if the patient is lying down.
D. SENSORY EXAMINATION
Possible findings o Impaired proprioception o Perioral numbness (hyperventilating patients) o Glove and stocking paresthesias
suggestive of peripheral neuropathy (diabetes)
o Romberg’s Test
Differentiates between a proprioceptive vs a cerebellar cause of imbalance
E. DEEP TENDON REFLEXES
Possible findings
(1) Hyporeflexia
(2) Hyperreflexia
(3) Pendular reflexes – swaying back and forth due to cerebellar problem
Gienah, AJ, Irene
Lecture 21: Dizziness OS 211
ROMBERG’S TEST
PROCEDURE
RESULTS
1) Ask patient to stand, with feet together and arms apart.
2) Eyes are open initially.
3) Ask patient to close eyes.
(+) falls with eyes closed (dorsal column problem)
You don’t say negative RT, just say: does not fall with eyes closed
Falls with eyes open (cerebellar)
If vision is taken away and patient loses balance, it means that there is a vestibular disorder or a proprioceptive disorder
Basis of this test is balance involves a combination of proprioception, vestibular input, and vision; if any 2 of these systems are working, the person should be able to demonstrate a fair degree of balance
(+) Romberg indicates a dorsal column problem.
Differentiating Central from Peripheral Vertigo: Spescial Maneuvers
To Test the Labyrinth
A. HEAD SHAKING – test for vestibular problem
Ask patient to shake his head, as in saying “no”, for
PROCEDURE
20 seconds.
-Check for nystagmus- slow phase moves toward the side of the unilateral peripheral lesion.
RESULTS
(+) falling, marked intensification of dizziness because the vestibular apparatus is overwhelmed
( –) no change
Figure 11. Frenzel Lenses. Patient can wear Frenzel lenses which are high diopter lenses that prevent fixation, allowing vestibular nystagmus to be seen clearly and to separate him from the environment Magnifies the eyes
B. RAPID IMPULSE TEST
Also called the head thrust test or passive head movement test
Used to test for ocular instability
Among the most reliable bedside tests for labyrinthine function
PROCEDURE
1) Ask patient to relax first, then fixate on a target.
2) Explain the need to relax the neck muscles while remaining focused on the target.
3) Examiner quickly rotates the patient’s head by 10°.
4) Observe patient’s eyes for slippage from target with quick saccadic correction.
NORMAL eyes remain on target
RESULTS
ABNORMAL slippage with quick saccadic motion
Page 5 / 9
Lecture 21: Dizziness OS 211
MECHANISM OF DIX-HALPIKE
Dix-Hallpike maneuver (change from position A to position B) triggers the movement of the otolith into the more slender lumen (like a roller coaster) leading to
BPPV nystagmus.
Figure 12. Rapid Impulse Test.
A & B: Normal finding. The patient’s eyes stay fixated on the target even with head rotation.
C, D, & E: There is a R-sided lesion. The eyes remain in midposition with quick saccadic correction (by frontal eye fields and cerebellum)
Ocular instability is elicited when head is turned toward the side of the peripheral lesion o The eyes overshoot towards the side of the lesion. It does not move to the other side to stay fixated on the object. o Then the frontal eye fields and cerebellum compensate to bring eyes back to direction of the target causing saccades .
C. DIX- HALPIKE MANEUVER
A diagnostic maneuver used to identify Benign Paroxysmal
Positioning Vertigo (BPPV)
History and a (+) Dix-Hallpike are sufficient to make a diagnosis of
BPPV (no need for further tests or imaging studies).
MECHANISM OF VERTIGO IN DPPV
Figure 13. Dix-Hallpike Maneuver.
PROCEDURE
RESULTS
1)
Patient’s head is rotated 45° sitting down.
2) Quickly move the patient from the sitting position to the supine position with the head tilted 30 °-40° over the end of the table. Maintain this position for
30s with patient’s eyes open to see if eyeballs have nystagmus.
3) Rapidly bring up the patient to the sitting position.
4) Repeat the procedure with the patient’s head rotated 45° to the left side, then again rotated 45° to the right side.
(+) nystagmus
( –) no nystagmus
Rule of Thumb: 30 seconds (not shorter, because this is the time when the patient will say that they are dizzy)
After a latency of few seconds the patient develops sudden vertigo.
Dysfunctional ear is the one that is downward when vertigo occurs.
Rotatory torsional nystagmus: the fast component moves away from the affected ear (ear is firing unnecessarily).
Duration of vertigo and nystagmus: 30-40 seconds , usually less than
15 seconds.
Changing from supine to sitting position reverses the direction of vertigo and nystagmus.
Changes in position confirms labyrinthine involvement (this is already a confirmatory test for benign positional vertigo ; no need for MRI)
Jerking is caused by the frontal eye field.
Repeated maneuvers may no longer result in vertigo and nystagmus
(“ fatigue
”).
Gienah, AJ, Irene
Figure 13. Mechanism of R Horizontal SCC Lithiasis.
small arrows – direction of otolith movement large arrows
– direction of deviation of the cupula o Pathology: otolith breaks off. It will move downward and will give a sensation of movement when there wasn’t any. o Usually in the lateral semicircular canals (SCC)
Unilateral stimulation of SCC by movement of otoliths when there is no head movement -> an exaggerated response without a stimulus (mind is tricked, you feel like you are turning around even if you’re just stationary)
D. CALORIC MANEUVER
Tests for diminished labyrinthine response to thermally-induced nystagmus on the affected side
Involves alternate irrigation of the external auditory canals by cold
H
2
O followed by warm H
2
O
Checks if labyrinths are functional or not by inducing change in temperature of fluid in the inner ear
A test for comatose patients. Brain dead patients will have no response.
Figure 14. Caloric Testing.
Page 6 / 9
PROCEDURE
RESULTS
1) The patient’s he a d is tilted forward 30 ° above the horizontal so that the horizontal SCC assumes a more vertical position.
2) Irrigation first with cold water (7 ° below body temperature) for 30s.
3) After 5 min, irrigation with warm water (7
° above body temperature) for 30s.
NORMAL eyeball deviation
ABNORMAL no eyeball deviation
Cold Water
Warm Water
Fast phase of nystagmus to the side opposite from the cold water filled ear
Fast phase of nystagmus to the same side as the warm water filled ear
Absence of response will indicate the paretic side
“
COWS
” (
Cold Opposite , Warm Same )
E. OTHER ELABORATE MANEUVERS
1 . Barany Chair: Used in NASA to prepare astronauts for zero gravity environment; also for anti-vertigo treatment
2. Unterberget Test – to assess whether a patient has vestibular pathology, not useful for central disorders of balance
PROCEDURE Patient is asked to walk on spot with eyes closed.
NORMAL no rotation
RESULTS
ABNORMAL rotation to side of labyrinthine lesion
3. Fukuda Test – diagnosis of vertigo-associated disease
PROCEDURE 1) Ask patient to march in place.
RESULTS
NORMAL no rotation
ABNORMAL 10-
20° angle deviation to the L or R
V. COMMON DIZZINESS SYNDROME
A. BENIGN PAROXYSMAL POSITIONING VERTIGO
Also simply called benign positional vertigo.
The most common cause of vertigo in clinical practice
The usual onset is middle age
Brief periods of vertigo induced by position changes of the head; vertigo is precipitated by certain events (e.g. rolling over in bed, getting in or out of bed, bending over, extending the neck)
Vertigo typically lasts a few seconds, always less than one minute
Pathophysiology
Caused by dislodgement of CaCO
3
crystals from the otolithic membrane in the utricle o Cupulolithiasis
Settling on the cupula o Canalolithiasis
Free floating in the membranous portion of the posterior SCC
Figure 15. Positions of Crystals in BPPV.
Diagnosis
Based on history and supported by a (+) Dix-Hallpike test
Torsional rotatory nystagmus with fast component toward the affected ear when it is placed downward
Treatment
Most patients’ symptoms resolve without treatment (1/3 - 2/3 of patients) within a week to a month o During period of illness, can be very distressing to the patient o Symptoms recur in more than half of patients
Vestibular Suppressants o Do not prevent vertigo o Long-term use of these medications is discouraged
Gienah, AJ, Irene
Lecture 21: Dizziness OS 211
Vestibular Rehabilitation Exercises
Canalith Repositioning Maneuvers o Has showed improvement rates of 67-89%
Semont Maneuver o Performed 3x a row, 3x a day (morning, noon, and night) o Most patients become free of symptoms after doing this for 3 days
Figure 16. Semont Maneuver.
PROCEDURE
1) The patient initially in a sitting position, with his head turned 45
° to the side of the unaffected ear.
2) The patient is laid on the side of the affected ear, with head still turned. The position is maintained for about a minute. o Induces movement of the particle in the
SC by gravity, leading to rotatory nystagmus toward the lower ear that extinguishes after a brief interval
3) With the head still in the same place, patient is rapidly swung over to the side of the unaffected ear, so that the nose now points downward. This position is maintained for about a minute. o Particle in SC now moves toward the exit from the canal
4) The patient returns slowly to sitting position. o Particle settles in utricular space, where it can no longer induce rotatory vertigo
Surgery o Rare patients who fail to respond to vestibular rehabilitation or canalith repositioning are candidates o Done only if the correct ear and correct semicircular canal has been identified (usually the posterior SC)
Mechanical Occlusion
Division of the Singular Nerve
Division of the inferior vestibular nerve that supplies the posterior SC
Disconnect the SC from its nerve supply
B. PHOBIC POSTURAL VERTIGO
Also called non-otogenic dizziness and psychogenic dizziness
Second most common cause of vertigo
Attacks are precipitated or exacerbated by stressors, which can be typical situations (e.g. crowds, empty spaces, driving)
Patient’s personality is usually of an obsessive-compulsive or reactive-depressive type
At the onset of the disorder, there’s a vestibular disturbance (25%) or a stress ful situation (70%)
Clinical Features
Postural vertigo with unsteadiness of stance and gait
Neurologic exam and ancillary tests are generally unremarkable
Fluctuating unsteadiness of stance and gait with attacks of fear of falling, but without an actual fall
Anxiety and autonomic disturbances during or after the attacks
Increasingly severe avoidance behaviour is common
Page 7 / 9
Treatment
A thorough diagnostic assessment to allay the patient’s fear of having a serious organic disease
– tell patient that there is really nothing wrong with them
Psycho-educative therapy to inform the patient of the pathologic mechanism and the precipitating factors and situations
Desensitization by self-exposure (i.e. deliberately seeking out situations that precipitate vertigo, e.g. riding roller coasters)
Light sporting activity or consumption of a small amount of alcohol can also improve symptoms
If symptoms persist, pharmacotherapy, e.g. selective serotonin reuptake inhibitors (SSRIs), and/or cognitive behavioral therapy
Treatment markedly improves symptoms in about 70% of patients
C. MENIERE’S DISEASE
Impaired drainage of endolymph due to lymphatic channel dilation leading to accumulation of endolymph inside the SCC
Attacks usually last <24 hours
Cause is usually idiopathic, but may be due to trauma, ear surgery, or ear infections
NORMAL EAR
MÉNIÈRE'S DISEASE
EAR
Figure 17. Build-
Up of Endolymph in Ménière’s Disease.
Clinical Features
Triad of inner ear pathology: episodes of dizziness , tinnitus , and hearing loss
Sensation of fullness in the ear
Temporary hearing loss and distorted hearing during attacks
“Drop attacks” = sudden vertigo leading to falls
Histopathology
Distension of endolymphatic system
Episodic ruptures the of endolymph into perilymph
K + in endolymph damages hair cells in the organ of Corti, leading to hearing loss
Cause is usually idiopathic, but may occur after trauma, ear surgey, or ear infection
Figure 18. Distension of the
Semicircular Canals in Ménière’s
Disease.
Treatment
Management is empirical: antiemetics and vestibular suppressants
Patient is maintained on low salt diet and diuretics
May lead to deafness if untreated
D. VESTIBULAR NEURITIS
A diagnosis of exclusion or a wastebasket diagnosis
Symptoms usually peak within 24 hours
Patient lies relatively immobile because movement worsens the symptoms
Symptoms will subside in several days, up to 3 months, until the patient’s vestibular system compensates
Gienah, AJ, Irene
Lecture 21: Dizziness OS 211
Clinical Features
Figure 19. Vestibular Neuronitis.
Sudden severe vertigo with nausea/vomiting in the absence of auditory symptoms
Absence of hearing impairment/tinnitus
Absence of neurologic deficits
Vertigo with spontaneous nystagmus , with fast component beating away from involved ear (usually unilateral)
Treatment
Short-term use of antihistamines / anticholinergics
Anti-emetics
Benzodiazepines (if necessary, for sedation)
Corticosteroids (if started early, shorten duration of the disease)
Avoid prolonged immobility
Vestibular rehabilitation
Low salt diet and diuretics
VI. POTENTIALLY LIFE-THREATENING CAUSES OF VERTIGO
T Percentage of dangerous diagnoses increases as age increases, with the highest percentage (about 25%) in patients
≥75 years old
(+) neurologic deficits or the 5Ds (dizziness, dysphagia, dystaxia, diplopia, dysarthria)
A. CEREBROVASCULAR DISEASE
5 Ds: Dizziness, diplopia, dysarthria, dysphagia, dystaxia
May result from the following: o Anterior Inferior Cerebellar Artery Infarction (AICA)
Supplies the brainstem and labyrinth, so presents with inability to hear in one ear o Posterior Inferior cerebellar Artery Infarction (PICA)
Supplies the medulla o Cerebellar Hemisphere Infarcts o Cerebellar Hemorrhage
By compressing the 4 th ventricle, you get hydrocephalus which may cause hernia
B. BACTERIAL LABYRINTHITIS
Life-threatening if not promptly treated with antibiotics
Acute purulent infection of the labyrinth, usually an extension from chronic mastoiditis
Bilateral cases may occur with bacterial meningitis
VII. MANAGEMENT OF DIZZINESS
Stabilize the patient
Rule out the most life-threatening diagnosis (5D’s) and manage accordingly
Depending on the localization, refer to a neurologist/otorhinolaryngologist/cardiologist/psychiatrist
Guided by history and PE, perform diagnostics (but you don’t need to s pend money on these) o Routine work-ups (CBC, blood chemistries; R/O SLE) o Cardiac enzymes, 12-lead ECG (R/O cardiac problems) o Arterial blood gases, pulse oximetry, CXR (R/O metabolic problems) o Imaging of the skull and brain (CT/MRI) if you think there’s a structural problem of the inner ear, middle ear, or the brain
Therapeutics o Reassure the patient o Semi-prone, lie on the side to avoid aspiration of vomitus o Supplemental O
2
via nasal cannula, if necessary o Insert IV line only when they need fluid resuscitation o Vestibular suppressants :
Page 8 / 9
Antihistamines – reduces motion sickness, also have anticholinergic activity, only those which cross the blood brain barrier are useful
Meclizine 25 mg tab PO q8
– q12 hours
Dipenhydramine 25-50 mg tab PO q6 hours
Anticholinergics - only for prevention, not for cure
Scopolamine 0.5mg transdermal patch q3-q4 days (behind ear)
Histamine (H3) agonists
Betahistine 8mg-32mg TID
Increase blood circulation to the labyrinth
Considered as placebo by US FDA o Anti-emetics
– if necessary
Promethazine 25-50 mg PO/PR q6 hours o Anxiolytics and antidepressants
If warranted, try to avoid these because they induce dependence
Diazepam 2mg tab PO q8-q12 hours
Clonazepam 2mg 0.5mg tab PO q12 o
Vestibular rehabilitation
VIII. SUMMARY
Allow the dizzy patient to explain how he feels in his own words
Determine if your patient has vertigo vs. non-vertigo
Localize the vertigo o Is it in the ear or CNS? o Is it in the labyrinth, vestibular nerve, or brainstem?
Stabilize the patient
Treat the vertigo and the nausea/vomiting
Reassure the patient and refer (e.g. to ORL)
END OF TRANSCRIPTION
G: Hello 2017 (Reign Supreme!)! Hello transmates! Hello researchmates, clingy, anatomates. Hey hey , Phivestar, Extradyizz,
Ampliphi! Hello buddy Martin! Watch and download the soundtrack of
Frozen and watch Wicked next year. Chuck Palahniuk has a new book
(Doomed) grab a copy! Also, merry merry Christmas and happy happy
2014 in advance! :D
Lecture 21: Dizziness OS 211
“Choose your battles wisely. After all, life isn't measured by how many times you stood up to fight. It's not winning battles that makes you happy, but it's how many times you turned away and chose to look into a better direction. Life is too short to spend it on warring. Fight only the most, most, most important ones, let the rest go.” –C. JoyBell C.
A: MER RY CHRISTMAS CLASS 2017! Let’s not forget the real reason for the season!
I: Last trans before Christmas vacation! Huling tumbling na lang! To the people na kasama ko nung Friday, you guys are deeply appreciated!
Labyu powz!!! :D
Gienah, AJ, Irene Page 9 / 9