File
advertisement

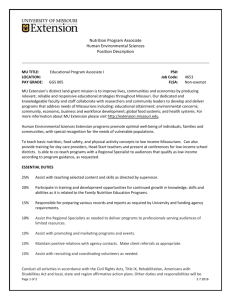
Neonatal Case Study JUNE 11, 2013 Mikaela Hew MS, CN UCSD MEDICAL CENTER | DIETETIC INTERN CLASS OF 2012-2103 Abstract Gastroschisis is a structural defect of the abdominal wall occurring in utero that allows the abdominal organs of a fetus to herniate to the outside of the abdomen. Because of the abnormal development of the bowel, it is susceptible to atresia with areas of necrosis, ischemia and perforation increasing the risk of lengthy hospital stay and postnatal complications. Developments in neonatal surgical procedures demonstrate long term positive patient outcomes for Gastroschisis. However, adequate nutrition and tolerance continue to be a challenging area for the care team, especially with consideration of any additional hospital complications. Some Gastroschisis cases ultimately require long term total parenteral nutrition (TPN) support. Baby Boy, “BB” was born at 34 weeks and 4 days, at a birth weight of 2064g via cesarean section to a 20 year old mother. BB was born with congenital Gastroschisis and was unable to have his gastrointestinal organs “reduced” back into the abdominal cavity and receive primary closure of the abdomen immediately after birth. Thus requiring placement of a protective covering over the organs (known as a “silo”) with gradual reduction of the herniated abdominal contents. Severe ischemic and necrotic bowel was found at birth requiring exploratory laparotomy with segmental small bowel resection, creation of jejunostomy and mucous fistula. Due to variability in bowel function and low “po” (by mouth) intake, BB has required TPN support since birth. Nipple and gavage feeding have been continually promoted in order to wean BB from TPN and to keep the digestive tract stimulated. Distal re-feeds were used to help stimulate the bowel and encourage adaptation. BB’s medical course has been complicated by cholestasis of parenteral nutrition, high ostomy output, multiple procedures interrupting po feeds and overall poor po intake. He is now status post stoma closure with anastomosis and continues on TPN with ongoing encouragement of po feeds. Introduction Normal gestation is 37-40 weeks with an infant being considered “term” between these two points. Infants born earlier than term are at risk of complication (s) and medical problems. Alternatively, infants with complication (s) in utero are at increased risk of being born premature. Prenatally, gestational age of an infant is determined based on several factors including maternal dates, uterine fundal height, and the presence of heart tones along with ultrasound evaluation (1). 1|Neonatal Case Study Hew The following categories are provided to classify an infant based on gestational age: Preterm <37 weeks gestation Term 37-42 weeks gestation Post Term >42 weeks gestation And the following categories for infant birth weight: Low birth weight (LBW) <2,500 g Very low birth weight (VLBW) <1,500 g Extremely low birth weight (ELBW) <1,000g At the same gestational age, the infant born at lower birth weight has a higher mortality rate than the infant born at appropriate weight. Mortality risk decreases with increasing birth weight and gestational age until birth weight reaches 4500 g or the infant becomes post-term (1). The choice of feeding method is influenced by gestational age. Gastrointestinal development occurs at an early stage in utero. At four weeks gestation, the intestine is a small tube. By the fifth week, it begins elongating faster than the trunk, so that by 40 weeks the intestine is 1,000 times longer than it was at 5 weeks. The length of the small intestine for an average newborn is said to be 200-300cm (1). A small bowel of 253 cm would be divided roughly into 5cm of duodenum and 248 cm of jejunum and ileum. The colon averages 45cm, which is 1/6th the small intestine (1). By the sixth week, closure of the skin folds making up the abdominal wall occurs. If there is incomplete closure, the intestines and/or stomach is susceptible to herniation (2). Gastroschisis Gastroschisis is a structural defect, or “hole” in the abdominal wall in which gastrointestinal organs herniate to the exterior of the abdomen of a fetus. Gastroschisis differs from Omphalocele in that the organs usually herniate to the right of the normally inserted umbilicus and are not covered by a protective sac. The proposed reasons for herniation include: defective development of mesenchyme in the abdominal wall or abnormal involution of the umbilical vein causing weakness or rupture of a small Omphalocele with absorption of the sac and growth of skin between the resultant opening and the umbilical cord (3). Gastroschisis is diagnosed using prenatal ultrasonography as early as 14 weeks after conception. An additional way to diagnose Gastroschisis is detection of Maternal Serum Alpha-Fetoprotein (MSAFP) which is done during the Triple, Quad, or Penta screens used to check for Down syndrome and other birth defects (4). The exposure that the organs have to amniotic fluid in utero can interfere with normal development and 2|Neonatal Case Study Hew function. Also, because of the unusual position and location, the organs can become kinked, blocked and lead to atresia with resulting loss of blood supply. Fetuses with Gastroschisis are more likely to be born premature. Treatment of Gastroschisis requires surgery early after birth to remove any necrotic segments and to “reduce” the bowel into the abdominal cavity (if possible). If the bowel is unable to be reduced, and the abdomen closed, a silo will be placed. A silo is a protective covering placed over organs exposed to the outside environment while the bowel is slowly reduced (by hand) back into the abdomen (5). A silo increases hospital stay by 10-14 days. Complications of Gastroschisis are very common, especially those related to the gastrointestinal tract (6). In about 15% of cases, babies have atresia which can cause intestinal perforation with resulting leakage of contents into the abdominal cavity, or as mentioned earlier, the abnormal positioning of the gastrointestinal organs could cause a disruption in blood supply. These complications may require multiple surgeries and bowel resection along with gastrostomy, ileostomy or jejunostomy which allows stool to pass through into a bag on the abdominal wall (4). Additionally, hypothermia (due to exposure of the intestines to the environment), dehydration, sepsis, or hypoglycemia may complicate the medical course. Prolonged feeding problems and slow weight gain most often occur when an atresia, intestinal leak or poor intestinal blood flow complicates Gastroschisis. Until gastrointestinal function normalizes, babies are fed via neonatal parenteral nutrition (PN) (4). The etiology of Gastroschisis is unknown, however some research suggests environmental factors, elevated estrogen levels, smoking, drug or alcohol use as possible causes. The main risk factor is young maternal age (7). “Part of the complexity in unravelling the relative risk factors remains the bias inherent in any study attempting to retrospectively correlate peri-conceptual diet and behavioral factors, including exposure to putative environmental hazards and toxins, with a subsequently identified congenital abnormality (8).” Reported survival rates are good for Gastroschisis, approximated at 90% over the last decade (9). However, the postoperative hospital stay is often lengthy, and while advancements in neonatal surgical procedures have improved infant outcomes, there remains limited data on the long-term prognosis of gastrointestinal function, cardiopulmonary and neurodevelopmental outcomes (8). Neonatal physicians in Minnesota are currently conducting a study on the longterm outcomes of Gastroschisis patients and so far the results show that most babies develop normally, although they 3|Neonatal Case Study Hew may grow slowly in the first few years (4). For nutrition clinicians it may be speculated that depending on how much of the bowel was affected by ischemia and/or necrosis with resulting surgical resection during hospital stay, the dietary management may mirror that of a short bowel/short gut syndrome patient with requirements for long term PN and monitoring for malabsorption as the diet advances. Long-term complications to consider include intestinal dysmotility, malabsorption resulting from mucosal injury or gastroesophageal reflux (3). Case Study Patient Baby Boy; “BB” was born at 34weeks and 4days via C-section to a 20 year old mother. The mother is G2P0111 which means she was pregnant twice, did not carry any to full-term, had one pre-term, had one abortion (or spontaneous abortion which is commonly referred to as miscarriage), and one is living. Mother is not married, and the father of the child is involved. Mother denied tobacco, alcohol, or drug use during pregnancy. At birth BB did not have a spontaneous cry and was floppy. He was placed on the radiant warmer and in a plastic bag to be stimulated. He required positive pressure ventilation and began to cry after 2 minutes. BB was intubated at 17 minutes of life and taken to the Neonatal Intensive Care Unit (NICU). BB was born with Congenital Gastroschisis with areas of necrosis, ischemia and perforation. He was immediately made nil per os/nothing by mouth (NPO) and prepped for the operating room for silo placement versus primary closure of the bowel and abdominal cavity. APGAR: An APGAR test is a quick test performed on a baby at 1 and 5 minutes after birth. The 1-minute score determines how well the baby tolerated the birthing process. The 5-minute score tells the doctor how well the baby is doing outside the mother's womb. The APGAR rating is based on a total score of 1 to 10. The higher the score, the better the baby is doing after birth (10). Each category is scored with 0, 1, or 2, depending on the observed condition as seen in FIGURE 1: 4|Neonatal Case Study Hew FIGURE 1: Apgar scoring system; BB Case Study For BB, APGAR scores as follows: (1 minute) Total: 2 (5 minutes) Total: 8 (-1 color, -1 respiratory effort) Summary of Medical Course BB was born with Congenital Gastroschisis and severe ischemic and necrotic bowel with suspicion of atresia. He required silo placement with secondary closure, exploratory laparotomy, segmental small bowel resection measuring 10 centimeters in length, jejunostomy, and mucous fistula placement. TABLE 1 lists the key procedures pertaining to the digestive tract BB underwent throughout his medical course to date. He developed hyperbilirubinemia, cholestasis of parenteral nutrition along with other complications detailed further in TABLE 2. He is now status post stoma closure and anastamosis of bowel segments with full closure of the abdomen. TABLE 1 Timeline of key procedures/hallmarks pertaining to the digestive system since birth for BB Case Study: Date Procedure Indication/Findings 1/18/2013 Primary closure versus SILO placement 1/24/2013 2/4/2013 SILO Fascial Closure Bowel Ultrasound attempt to close the abdomen, with gastrointestinal contents in place. BB required silo placement in the operating room to temporarily house the intestines reduction of the bowel found non-perfused tissue masses in the center of the abdomen, minimal peristalsis, care team with guarded prognosis of bowel survival 5|Neonatal Case Study Hew 2/12/2013 Upper Gastrointestinal Series 2/17/2013 3/6/2013 Bowel ultrasound Barium enema 3/12/2013 Exploratory laparotomy, segmental bowel resection, jejunostomy and mucous fistula Bloody output from proximal ostomy Kidney, Ureter, Bladder (KUB) Distal ostomy contrast study Herniation of proximal stoma Small bowel follow-through Stoma closure/anastamosis KUB 4/6/2013 4/17/2013 4/17/2013 5/6/2013 5/13/2013 5/16/2013 6/1/2013 series of x-rays found mid-bowel distension and stoppage of flow probably a result of atresia loop of bowel without perfusion, bowel improving found massive distension of proximal and mid-jejunal loops in the right side of the abdomen, indicating obstruction by probable adhesions or stenosis. The findings are consistent with the history of small obstruction and relatively unused colon commonly referred to as “Loop ostomy”, an ostomy was created and mucous fistula which was used for re-feeding. BB made NPO negative for obstruction caliber of colon appeared normal, no colonic stricture found required pressure, small blood loss no obstruction attachment of bowel, stoma closure, required NPO non-obstructive bowel gas pattern, suggestive of mild bowel wall edema Additional Medical Complications/Lab Values BB has had an extensive stay in the NICU, and in addition to the above required procedures and tests resulting from Gastroschisis, additional complications to the medical course include: TABLE 2 Additional medical complications for BB Case Study: Date Medical complication Indication/Findings 1/17/2013 1/19/2013 Prematurity Anemia 1/28/2013 2/4/2013 2/11/2013 2/23/2013 Elevated triglycerides Candidal dermatitis Cholestasis of parenteral nutrition/direct hyperbilirubinemia Peripheral pulmonic stenosis born at 2064g (categorized as low birth weight infant) requiring three transfusions; 1/30,2/21,3/23; attempting to keep Hemoglobin within 10-12 TPN lipids reduced to 2g/kg 2/23/2013 3/7/2013 Neonatal thrombocytopenia Hypochloremia w/ metabolic alkalosis 3/28/2013 Neonatal abstinence syndrome-suspectedresolved 4/3/2013 Elevated GIR, Dbili 4/6/2013 Left Hydrocele Ongoing High ostomy output with episode of dumping 6|Neonatal Case Study upward trending bilirubin levels; fish oil started 4/14 A narrowing in the pulmonary arteries that take blood from the heart to the lungs. This is common in babies and usually goes away on its own. low platelet count Acid-base disorder in which the pH of the blood is elevated beyond the normal range of 7.35-7.45. Likely caused by too much acetate and too little chloride in TPN (1). Group of problems that occur in a newborn exposed to addictive illegal or prescription drugs while in the mother’s womb. Also of consideration; resulting from pain medication given to infant from birth. Direct bilirubin levels continued to trend upward. With consideration of high glomerular infusion rate (GIR), A recommendation to decrease dextrose came from nutrition team. Fluid-filled sac surrounding a testicle causing swelling of the scrotum (11) episodes of high ostomy output warranted feeding adjustments. The care team also attributed some of the dumping to fish oil supplementation, and discontinued its use on 4/27. See Table 3 for details. Hew Additionally, the Alkaline Phosphatase level continued to rise (APPENDIX II) which will be discussed in further detail, as it is an indicator (along with elevated bilirubin) of cholestasis. Infant Growth Appropriate growth is critical in monitoring the efficacy of medical nutrition therapy provided to premature infants, especially in a patient with a lengthy medical course, and hospital stay. Despite the many procedures and interruptions in oral feeds BB experienced, the PN provided adequate nutrition for him to continue growing (see APPENDIX 1). It is normal for a preterm infant to lose weight right after birth, and then birth weight should be regained by 2 weeks of life. Approximately ≤15% can be lost as body water compartments contract. Maximum weight loss is expected by the fourth to sixth day of life (1). Despite his medical course, BB continued to gain weight between the 10th%tile and 50th%tile as demonstrated in the growth charts (see APPENDIX 1). The desired weight gain for an infant of his gestation would be 20-35g/d, or approximately 13.3-14.2g/kg/d (1). He gained approximately 30.5g/d over the last month. Desired length gain of a preterm infant is about 0.8-1.1cm per week (1). In BB, length had been variable with a few distinct drops in measurements 2/1, 2/21, 3/1 and 3/28. To date, length has trended back up, and is now >50th%tile (see APPENDIX 1). Length is a very important measurement in the neonatal population because it more accurately reflects lean body mass and is not influenced by fluid status (1). It is also normal for an infant to lose head circumference during the first postnatal week by approximately 0.5cm due to contraction of the extracellular space. Catch-up growth usually occurs quickly, with an average of 0.5cm/wk growth in the infant between birth and 3 months of age (1). For BB, head circumference growth generally was steady, and trends between 50th%tile to 90th%tile (see APPENDIX 1). Medications/Supplements Vitamin and mineral supplementation is extremely important in the premature infant, particularly in those requiring PN (1). For instance, fat soluble vitamin supplementation may be warranted from birth due to deficiencies, or throughout medical course depending on complications such as malabsorption. Premature infants are born with lower liver stores of vitamin A and have lower serum retinol values than term infants (1). Recommendations for supplementation range 7|Neonatal Case Study Hew from 700-1500IU/kg/d (12). Preterm infants are also born with low body stores of vitamin E however supplementation recommendations vary primarily with regards to formula fed infants or for those receiving supplemental iron, which acts as a pro-oxidant. Vitamin E supplementation would then be warranted to prevent vitamin E deficiency-induced hemolytic anemia. If therapeutic doses of iron are administered, vitamin E supplementation may also be necessary to reach the preterm goal of 6-12IU vitamin E/kg/d. Preterm infants have limited reserves of Vitamin D, and evidence suggests supplementation of 150-400IU Vitamin D to maintain normal vitamin D status in most term infants (1, 13). Lastly, endogenous vitamin K production by intestinal flora may be impaired by long term parenteral nutrition and antibiotic usage. Current guidelines suggest a dose of 80 µg/kg/d for preterm infants (14). Minerals such as sodium and potassium are excreted quickly during the first 10-14 days of birth in preterm infants. Sodium is needed up to 2-3mmol/kg/d, and potassium of 2-3mEq/kg/d. Calcium, phosphorus and magnesium are all accrued during the last trimester of pregnancy. Therefore, preterm infants may require higher amounts than term infants. This is difficult to do in patients on PN, so osteopenia is common in some very low birth weight premature infants (12). Preterm human milk contains approximately 40mg of calcium/100kcal, 20mg of phosphorus/100kcal, and has been associated with impaired bone mineralization (12). Calcium intake is recommended at 60-90mg/kg via parenteral nutrition, 120-230mg/kg for enteral nutrition. Phosphorus is recommended at 47-70mg/kg via parenteral route and 60-142mg/kg via enteral route. Magnesium is recommended at 4.3-15mg/kg (14). Iron levels are lower in the preterm infant at birth than the term infant and supplementation may be needed. But, the physiologic anemia of prematurity may not be ameliorated by iron therapy, so blood transfusions may be necessary. However this practice is controversial (12). Iron supplementation is not commonly practiced during the first 2 weeks of life. Unless an infant is human milk fed, iron at 2-4mg/kg/d should be initiated at 2-4 weeks of age (12). This supplementation should continue to 12 months of age. Supplementation is also not necessary if an infant is on full enteral nutrition with mom’s breast milk, or a standard formula at volume of >180mL/kg until 4-6months of age (14). Additionally, trace mineral supplementation may be needed, notably zinc, copper and iodine. Zinc levels in colostrum decrease postpartum, and zinc deficiency has been reported in preterm breastfed infants. Recommendations are 400mcg/kg. Copper absorption is affected by dietary zinc, and copper deficiency has been identified among infants 8|Neonatal Case Study Hew being fed cow milk or copper-free PN (1). The recommended level in PN is 20mcg/kg or 120-150mcg/kg in enteral nutrition (1). Lastly, iodine levels of human milk vary depending on the mom’s intake, and formulas supply the recommended amount. Intake recommendations are 1mcg/kg for PN route, and 30-60mcg/kg via enteral route (1). A pediatric multivitamin would be warranted in an infant that is taking <1000mL volume of breast milk, or <32 ounces of formula. If a baby is stable and on PN, a pediatric multivitamin should be provided at 2cc/kg (14). In consideration of the general supplementation recommendations, BB received the following supplements: *Note: Pertinent nutrition related medications are also listed and will be addressed again in further along in the paper. At birth: Plasmalyte A IV bolus 21mL and 1,000mL infusion (water, electrolytes and 21kcal/L) NaCl 26mL, Vitamin K 1mg, Dextrose 10% + Heparin 0.5units/mL. AQUADEKS 0.5mL 4/24-5/15 (likely supplemented in suspicion of malabsorption) Cholecalciferol 400units 4/8-4/26 and 4/28-5/15 and 5/26-5/30 and 6/4-6/6 Epoetin Alfa 300units/kg 4/14-4/23 Pepcid 1.1mg 4/7-4/7 Prevacid 4/19-5/11 and 5/25-5/30 and 6/4 to current Ferrous Sulfate 6.9 mg 4/14-4/25 (increased while on epoetin alfa) Ferrous Sulfate 4.65mg 4/25-4/26 and 4/28-5/11 (decreased once patient started on small enteral feeds) Ferrous Sulfate 5.4mg 5/11-5/15 Ferrous Sulfate 11.5mg 5/29-5/30 Fish Oil/DHA 100mg/mL 4/14-4/26 Actigall 15mg/kg 4/17-5/15 NaCl infusions since birth Na Acetate in TPN since birth Trace elements in TPN since birth Pediatric multivitamin in TPN since birth Summary of feeding changes BB’s bowel was unable to be utilized immediately after birth due to Gastroschisis, necrotic tissue and ischemia requiring immediate operating room procedure for silo placement versus attempted primary closure. BB was immediately started on TPN and has continued to receive TPN for duration of hospital stay which has met 100% of calorie and protein needs in the absence of adequate enteral nutrition. Mother’s breast milk was used for three months while initiating nipple feeding and once it ran out, baby was transitioned to Pregestimil which he did not tolerate, so ended up on Neocate. Neocate is an appropriate formula as it is elemental and indicated for bowel resection, short gut syndromes and other digestive medical complications. TABLE 3 summarizes the significant changes to BB’s feeding regimen which was 9|Neonatal Case Study Hew complicated by high ostomy output, frequent NPO orders for procedures or tests, persistently elevated bilirubin, triglyceride levels, recent bilious residuals and the development of oral aversion. TABLE 3: Summary of feeding changes; BB Case Study Date Birth: 1/17/13 1/22/13 Total Fluids mL/kg/d 140 1/28/13 2/3/13 160 2/14/13 3/20/13 Infant Weight (kg) 150 Nutrition TPN Provides/%Needs Glucose infusion rate (GIR) Significance of feeding change D10% AA 6g +plasmalyte 8mL/hr 2.064 D10% AA 3.5g IL 2.5g/kg 2.064 D11% AA 3.5g IL 2g/kg 2.29 2.55 3.74 3/21/13 3.83 3/22/13 3.905 3/24/13 4.075 3/25/13 4.075 4/2/13 4.305 4/6/13 4/7/13 4.425 4/11/13 4.55 81.6kcal/kg/d / 75% 3.49g/kg/d / 100% 85.8kcal/kg/d / 70% 3.49g/kg/d / 100% 8.8mg/kg/min D13% AA4g IL 2.5g/kg 111.6kcal/kg/d / 100% 4g/kg/d / 100% 14.5 mg/kg/min D14% AA4g IL 2.5g/kg +MBM Bottle nipple feeding 68% D14% AA4g IL3g/kg +MBM 1mL/hr via Gavage D14% AA4g IL3g/kg +MBM 2mL/hr via Gavage D14% AA4g IL3g/kg +MBM 1mL/hr via Gavage 117.5kcal/kg/d / 100% 4g/kg/d / 100% 117kcal/kg/d / 100% 4g/kg/d / 100% 117kcal/kg/d / 100% 4g/kg/d / 100% 117kcal/kg/d / 100% 4g/kg/d / 100% 15.5 mg/kg/min D14% AA4g IL3g/kg +MBM 1mL/hr via Gavage + nipple feed 3mL q3h-->24mL q3h (40mL/kg/d) D14% AA4g IL3g/kg +MBM 1mL/hr via Gavage + nipple feed 21mL q3h (40mL/kg/d) D14% AA4g IL3g/kg +MBM Nipple Feeds 21mL q3h+ Distal feeds via stoma 3mL q 12hrs D5% NPO d/t bloody output 117kcal/kg/d / 100% 4g/kg/d / 100% 14.6 mg/kg/min 117kcal/kg/d / 100% 4g/kg/d / 100% 14.6 mg/kg/min 117kcal/kg/d / 100% 4g/kg/d / 100% 14.6 mg/kg/min D12% AA4g IL3g/kg +MBM Nipple feeds 69mL/kg/d, advancing by 3mL q12hr D14% AA4g IL3g/kg + MBM+ HMF+ BP Nipple feeds 69mL/kg/d, advancing by 3mL q12hr-->77mL/kg/d 118kcal/kg/d / 100% 4g/kg/d / 100% 14.7 mg/kg/min 118kcal/kg/d / 100% 4g/kg/d / 100% 14.6 mg/kg/min 10 | N e o n a t a l C a s e S t u d y 10.6mg/kg/min DBILI 0.8 (1/24)<-0.5(1/21) <--0.5(1/19) IL Kept low due to RISK of HYPERBILI 14.6 mg/kg/min 14.6 mg/kg/min 14.6 mg/kg/min HIGH OUTPUT reduced gavage feeds HIGH OUTPUT reduced nipple feed NPO Hew Difficulty w/ Nipple Feeding 4/12/13 4/20/13 4.55 160 4.706 4/23/13 4.884 4/23/13 4.884 4/27/13 4.895 5/1/13 5.206 5/6/13 5.188 5/9/13 5.188 5/10/13 5.188 D14% AA4g IL3g/kg + Pregestimil Nipple feeds Pregestimil not tolerated, changed to Neocate 40mL q3hr Nipple feeds + Distal refeeds at 6mL/hr D14% AA4g IL3g/kg + Neocate 20mL q3hr Nipple feeds +Distal refeeds at 6mL/hr NPO for PICC Line Extraction + D12% AA4g IL3g/kg D12% AA4g IL3g/kg + Neocate 20mL q3 hr Nipple feeds + Distal refeeds at 7.5mL/hr 118kcal/kg/d / 100% 4g/kg/d / 100% 14.6 mg/kg/min Mom ran out of MBM 21kcal/kg/d / 100% 4g/kg/d / 100% 15.3 mg/kg/min HIGH OUTPUT 13.3 mg/kg/min NPO 111kcal/kg/d / 100% 4g/kg/d / 100% 13.3 mg/kg/min 117kcal/kg/d / 100% 4g/kg/d / 100% 15.5 mg/kg/min 117kcal/kg/d / 100% 3.76g/kg/d / 94% 15.5 mg/kg/min 117kcal/kg/d / 100% 4g/kg/d / 100% 15.6 mg/kg/min 117kcal/kg/d / 100% 4g/kg/d / 100% 15.6 mg/kg/min 117kcal/kg/d / 100% 4g/kg/d / 100% 15.6 mg/kg/min 117kcal/kg/d / 100% 4g/kg/d / 100% 15.5 mg/kg/min 107kcal/kg/d / 98% 4g/kg/d / 100% 91kcal/kg/d / 83% 4g/kg/d / 100% 90kcal/kg/d / 82% 4g/kg/d / 100% 13.7 mg/kg/min 5/16/13 120 5.431 5/21/13 140 5.75 D14% AA4g IL2.5g/kg + Neocate 20mL q3hr Nipple feeds + Distal refeeds at 7.5mL/hr D14% AA4g IL2.5g/kg + Neocate Nipple feeds advancing 4mL/d as tolerated D14% AA4g IL2.5g/kg + Neocate 30mL q3hr + Distal feeds at 10mL/hr NPO for Sutures on central line loosened + TPN D14% AA4g IL 2.5g/kg D14% AA4g IL2.5g/kg + Neocate Nipple feeds 30mL q3hr + Distal feeds at 10mL/hr NPO for stoma closure/ anastamosis + TPN D14% AA4g IL 2.5g/kg + Distal feeds at 16mL/hr TPN D14% AA4g IL 2.5g/kg 5/23/13 5.68 TPN D14% AA4g IL 1g/kg 5/29/13 5.79 5/30/13 5.84 TPN D14% AA4g IL 1g/kg + Neocate Nipple Feeds 80mL q3hr advancing 6mL q12hr TPN D14% AA4g IL 1g/kg + Neocate Nipple Feeds 80mL q3hr advancing 6mL q12hr 6/3/13 5.98 6/6/13 5.93 TPN D14% AA4g IL 1g/kg + Neocate Nipple Feeds 20mL q3hr advancing 10mL/kg/d q24hr TPN D14% AA4g IL 1g/kg 11 | N e o n a t a l C a s e S t u d y 13.2 mg/kg/min 13.2 mg/kg/min 90kcal/kg/d / 82% 3.96g/kg/d / 99% IL reduced for high DBILI NPO NPO Decreased IL due to high TBILI Bilious residuals NPO for 2 days for green bilious residuals + central line replacement 90 kcal/kg/d / 82% 3.94g/kg/d / 99% 92 kcal/kg/d / 77% 4g/kg/d / 100% NPO for 2 days, large bilious emesis Hew In general, the goal for glucose infusion rate (GIR) is clinically managed at <26mg/kg/min, but this can vary greatly on a case by case basis factoring the infant weight, total fluids and overall tolerance to TPN. For example, a 1.5kg infant at 150mL/kg of total fluids should be kept around 13mg/kg/min and a 2.0kg infant at 120mL/kg of total fluids may go up to 16.6mg/kg/min (1). To encourage bowel adaptation and absorptive function, around April, BB started to receive ‘distal re-feeds’ through the mucous fistula. This means that any output to the ostomy was re-fed to the mucous fistula at a designated rate. In premature infants with diverting ostomies and mucous fistulas, this practice prevents disuse atrophy (possibly making anastomosis and stoma closure easier), can reduce PN requirements and help eliminate cholestasis by stimulating enterohepatic circulation (15). Cholestasis of Parenteral Nutrition BB’s direct bilirubin (or conjugated bilirubin) and alkaline phosphatase continued to trend upward from birth (see Appendix II). About one month after birth, BB was diagnosed with cholestasis of parenteral nutrition (also parenteral nutrition-associated conjugated hyperbilirubinemia (PNAC)) which is a common problem in the NICU. Cholestasis is defined as any condition in which the flow of bile from the liver is slowed or blocked (1). PNAC primarily results from long term dependence on TPN, but is also notably caused by overfeeding, prematurity and Gastroschisis which are applicable to the case study of focus (16). Although the pathogenesis is still unclear, the literature suggests that cholestasis occurs late in TPN support in association with elevated serum alkaline phosphatase and bilirubin concentrations. The hyperbilirubinemia results from impaired hepatic bile flow, immature organ development including adynamic gallbladder (resulting from bowel disuse), an upsurge in release of conjugated bilirubin as the infant matures (16, 17) and direct liver damage resulting from TPN. Scientific literature suggests the increased alkaline phosphatase levels detected result from a damaged liver which regurgitates hepatic alkaline phosphatase back into the serum, or the when there is impaired biliary excretion of the enzyme (1,18). 12 | N e o n a t a l C a s e S t u d y Hew Several approaches to medical nutrition therapy may be taken in the infant with cholestasis of parenteral nutrition including: Discontinuation of TPN with advancements of enteral feeding (16,19) Cyclic TPN to give the liver a rest (19) Decreased doses of lipid infusion (19) Fish oil based intravenous fat emulsions (IVFE) vs. soybean IVFE are safe and effective, but research is still needed; with a grade C evidence (20, 21). Ongoing research including a newer study out of Texas Children’s Hospital suggests fish oil based lipid emulsions can resolve cholestasis in surviving infants (22). Studies show that it could take up to 1 month for the fish oil to have a lowering effect on direct bilirubin, and must be administered on a regular basis (20,22). Currently, the evidence analysis library of the Academy of Nutrition and Dietetics nor ASPEN do not provide guidelines for medical nutrition therapy for cholestasis of parenteral nutrition in neonates (23,24). Estimated nutrition needs Nutrition needs were estimated at the following for BB upon initial assessment: Total Fluids 150-200mL/kg/day 110-120kcal/kg 3-4g/kg Protein Re-estimated nutrition needs (3/26/13) Total Fluids 150-200mL/kg/day 120-130 kcal/kg 3-4g/kg Protein Rationale Estimated nutrition needs are calculated based on established reference ranges provided in kcal/kg and g/kg protein for an infant on TPN with small enteral feeds, and born at >1,000g (25). Total fluids are decided using the same criteria, but are ultimately stated per the primary care neonatologist. Nutrition Diagnosis Statement (PES) Patient with altered GI function r/t Gastroschisis AEB parenteral nutrition. Monitoring and Evaluation The primary goal for BB during hospital stay was to continue gaining weight at approximately 30g per day and to advance from TPN to enteral feeding as soon as medically able. In order to evaluate these goals, continuation of TPN with necessary adjustments of GIR and trending of direct bilirubin were important to assessing the adequacy of TPN with 13 | N e o n a t a l C a s e S t u d y Hew meeting needs, as well as for assessing tolerance until BB was taking more po. In addition, the nutrition team monitored for weight changes, the baby’s GI status and availability for enteral feeding initiation along with feeding progression, and pertinent lab values. Prognosis/Conclusion BB was born with Congenital Gastroschisis with areas of necrosis, ischemia and perforation. In Gastroschisis, the digestive organs herniate to the outside of a fetus’ body, and pose risks to the medical course such as the need for multiple surgeries, possible bowel resection and nutrition support via PN. BB is now 145 days old and received several ultrasounds, an exploratory laparotomy, 10 centimeter segmental bowel resection, jejunostomy with the placement of a mucous fistula. He recently received stoma closure and anastomosis. Because of his extensive medical course, enteral feedings were challenging, and BB required TPN since birth. He developed cholestasis of parenteral nutrition and hyperbilirubinemia. The nutrition support course was challenged by frequent NPO orders resulting from recurrent procedures, high ostomy output, now with recent bilious emesis and bilious residuals. More recently, the care team suspects BB has developed an oral aversion and BB received nasogastric tube placement for feeding support. The team has proposed breast milk only or changing formulas. Despite the complicated medical course, the long term prognosis for Gastroschisis is promising; however the challenges resulting from the need for long term TPN in the setting of poor po can continue to compromise organ function and can increase the risks of metabolic bone disease (13) in the developing neonate. 14 | N e o n a t a l C a s e S t u d y Hew References: 1. Groh-Wargo S, Thompson M, Cox JH. Nutritional care for high-risk newborns. Bonus Books; 2000. 2. Gastroschisis. University of Michigan Health System website. http://www.med.umich.edu/fdtc/diagnoses/fetal_diagnoses/abdominal/gastroschisis.shtml. Accessed May 31, 2013. 3. Pediatric Omphalocele and Gastroschisis. Medscape. http://emedicine.medscape.com/article/975583-overview#a0104. Accessed May 19, 2013. 4. Gastroschisis, what to expect. Minnesota Neonatal Physicians, P.A. website. http://www.minnesotaneonatalphysicians.org/info_gastroschisis.php?thisPage=parents. Accessed May 31, 2013. 5. Gastroschisis treatments. UCSF Medical Center.org. http://fetus.ucsfmedicalcenter.org/gastroschisis/treatment.asp. Accessed May 27th, 2013. 6. Durfee SM, Benson CB, Adams SR, et al. Postnatal outcome of fetuses with the prenatal diagnosis of gastroschisis. J Ultrasound Med. 2013;32(3):407-12. 7. Birth Defects: Gastroschisis. CDC.gov. http://www.cdc.gov/ncbddd/birthdefects/gastroschisis.html. Accessed June 8th, 2013 . 8. Holland AJ, Walker K, Badawi N. Gastroschisis: an update. Pediatr Surg Int. 2010;26(9):871-8. 9. Santiago-Munoz PC, McIntire DD, Barber RG, Megison SM, Twickler DM, Dashe JS. Outcomes of pregnancies with fetal gastroschisis. Obstet Gynecol 2007:110 (3); 663–8. 10. Apgar Scores. Medline Plus Website. http://www.nlm.nih.gov/medlineplus/ency/article/003402.htm. Updated December 2, 2011. Accessed March 12, 2013. 11. Hydrocele. Mayo Clinic website. http://www.mayoclinic.com/health/hydrocele/DS00617. Accessed May 28, 2013. 12. M.D. RE. Pediatric Nutrition Handbook. American Academy of Pediatrics; 2009. 13. Nehra D, Carlson SJ, Fallon EM, et al. A.S.P.E.N. Clinical Guidelines: Nutrition Support of Neonatal Patients at Risk for Metabolic Bone Disease. J Parenter Enteral Nutr. 2013;1-29 14. Beaston, L. Preterm Infant Nutrition Guide. Rady’s Children’s Hospital 2013;1-3. 15. Wong KK, Lan LC, Lin SC, Chan AW, Tam PK. Mucous fistula refeeding in premature neonates with enterostomies. J Pediatr Gastroenterol Nutr. 2004;39(1):43-5. 16. Klein CJ, Revenis M, Ravenis M, Kusenda C, Scavo L. Parenteral nutrition-associated conjugated hyperbilirubinemia in hospitalized infants. J Am Diet Assoc. 2010;110(11):1684-95. 17. Causes of Neonatal Cholestasis. UpToDate. http://www.uptodate.com/contents/causes-of-neonatal-cholestasis. Accessed June 4th, 2013. 18. Enzymatic Measures of Cholestasis. UpToDate. http://www.uptodate.com/contents/causes-of-neonatal-cholestasis. Accessed June 4th, 2013. 19. Rees C. Management of PN-induced Cholestasis. Practical gastroenterology 2005: (24);62-68 20. Klein CJ, Havranek TG, Revenis ME, Hassanali Z, Scavo LM. Plasma fatty acids in premature infants with hyperbilirubinemia: before-and-after nutrition support with fish oil emulsion. Nutr Clin Pract. 2013;28(1):87-94. 21. Rangel S, Calkins C, Cowles R, Barnhart D, Huang E, Abdullah F, Arca M, Teitelbaum D. Parenteral nutrition-associated cholestasis: an American Pediatric Surgical Association Outcomes and Clinical Trials Committee systematic review. J of Pediatric Surgery 2012: 47(1); 225-240. 22. Premkumar MH, Carter BA, Hawthorne KM, King K, Abrams SA. High rates of resolution of cholestasis in parenteral nutritionassociated liver disease with fish oil-based lipid emulsion monotherapy. J Pediatr. 2013;162(4):793-798.e1. 23. Cholestasis. Evidence Analysis Library of Academy of Nutrition and Dietetics. http://andevidencelibrary.com/search.cfm?keywords=cholestasis&x=0&y=0. Accessed June 3, 2013. 24. Evidence Analysis Library. Academy of Nutrition and Dietetics. http://andevidencelibrary.com/default.cfm. Accessed June 4th, 2013. 25. Tsang R, Lucas A, Uauy R, Zlotkin S, eds. Nutritional needs of the pre-term infant: scientific basis and practical guidelines. Pawling, NY: Caduceus Medical Publishers, Inc for Williams & Wilkins, 1993 15 | N e o n a t a l C a s e S t u d y Hew Hagadorn, James I; Wolkoff, Leslie; Esposito, Patricia; Brumberg, Heather L; Emerick, Karan; Gerace, James R. Alterations in parenteral nutrition management for the treatment of parenteral nutrition‐associated cholestasis in term and preterm infants. Cochran Library 2009: 2 Hagadorn, James I; Wolkoff, Leslie; Esposito, Patricia; Brumberg, Heather L; Emerick, Karan; Gerace, James R. Medical therapies for parenteral nutrition‐associated cholestasis in term and preterm infants. Cochran Library 2009: 2 Feldman D, Pike JW, Adams JS. Vitamin D. Academic Press; 2011. Mutlu M, Cayir A, Cayir Y, Ozkan B, Aslan Y. Vitamin D and Hyperbilirubinaemia in Neonates. HK J Paediatr 2013;18:77-81 Burstyne M, Jensen GL. Abnormal liver functions as a result of total parenteral nutrition in a patient with short-bowel syndrome. Nutrition. 2000;16(11-12):1090-2. Brumbaugh D, Mack C. Conjugated hyperbilirubinemia in children. Pediatr Rev. 2012;33(7):291-302. Mehta NM, Compher C. A.S.P.E.N. Clinical Guidelines: nutrition support of the critically ill child. J Parenter Enteral Nutr. 2009;33(3):260-76. 16 | N e o n a t a l C a s e S t u d y Hew APPENDIX I Weight for Age Growth Chart 17 | N e o n a t a l C a s e S t u d y Hew Length for Age Growth Chart 18 | N e o n a t a l C a s e S t u d y Hew Head Circumference Growth Chart 19 | N e o n a t a l C a s e S t u d y Hew APPENDIX II Direct Bilirubin Alkaline Phosphatase 20 | N e o n a t a l C a s e S t u d y Hew