here
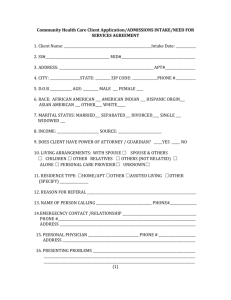
advertisement
IRNHAM LODGE SURGERY The Five Sign Up to Safety Pledges 1. Put safety first. Commit to reduce avoidable harm in the NHS by half and make public the goals and plans developed locally. Practice’s response: Irnham Lodge Surgery will aim to promote and develop a whole team culture in which patient safety and shared learning are at the heart of our practice values. Our mission statement will be adapted to reflect this and shared internally with our team and externally via our website home page. We will seek to promote our ‘no blame culture’ via staff training to ensure everyone understands this policy along with our over-arching Clinical Governance Policy which incorporates our approach to the learning from Significant Event and Near Miss Audits and complaints. Our goals and plans will be made public by: - Publishing the 5 safety pledges on our website; Publishing our goals and action plan in a suitable format on our website; An article in the December issue of our practice newsletter; Sharing future measures of performance towards our goals and action plan. Progress made: 2. Continually learn. Make their organisations more resilient to risks, by acting on the feedback from patients and by constantly measuring and monitoring how safe their services are. Practice’s response: Our practice already operates a robust complaints procedure and Significant Event Audit system which ensures that learning is shared appropriately internally, immediately when necessary, and with relevant external organisations when needed. Complaints are always treated as a Significant Event to ensure that a full audit is conducted and any learning is shared. The practice will seek to improve by: - - Encouraging patient feedback on the safety of our services and environment utilising the results of Patient Participation Group surveys, analysis from our suggestion cards, Friends and Family test comments, identify trends via complaint monitoring and through the audit of Significant Events and Near Misses; Publicising the review of our general complaints data on our website and via patient newsletters annually so that trends are identifiable to patients as well as our practice team; - Allocating chronic disease management leads to cascade latest guidance and learning from external sources to the team and to promote clinical audits to measure safety. Progress made: 3. Honesty. Be transparent with people about our progress to tackle patient safety issues and support staff to be candid with patients and their families if something goes wrong. Practice’s response: In line with our response to item 1, the practice will also strive to achieve the following: - - Actively promote and develop our ‘no blame culture’ internally to encourage and support transparency; Conduct staff training to ensure the robust operation of our complaints and Significant Event Audit procedures to encourage recording, reporting, sharing, follow up and review; Re-word our complaints statement on our website to emphasise our open, candid approach and commitment towards apologising to patients and their families when needed along with our internal ‘no blame culture’; Establish and monitor staff attitudes towards complaints and events and seek to make improvements where our ‘no blame culture’ may be failing; Encourage all individuals to reflect upon and share their personal learning from any events and consider how they would approach the situation if it were to happen again in order to continually improve. Progress made: 4. Collaborate. Take a leading role in supporting local collaborative learning, so that improvements are made across all of the local services that patients use. Practice’s response: Our practice will: - work with our West Somerset GP Federation colleagues to share learning from complaints, significant events and near misses where this may be beneficial to other local practices; - ensure that any local learning is cascaded to other service providers and commissioners where it is considered to be beneficial to the wider health community; - ensure that our whole team are aware of how to share learning externally via the CCG health professional feedback item which will be made available on all desktops. Progress made: 5. Support. Help people understand why things go wrong and how to put them right. Give staff the time and support to improve and celebrate the progress. Practice’s response: Our practice will strive to encourage individual team members to take the lead on the implementation of our patient safety and improvement culture by: - Encouraging personal reflection with a view to how people would approach the situation again; - Supporting individuals to present their ideas at departmental and MDT meetings; - Sharing the positive outcomes as well as the need for improvement by sharing results of audit and evaluation measures at departmental and MDT meetings; - Identifying individual training needs via our appraisal process and providing continuous professional development opportunities. Progress made: