Session 2 - A Curriculum for Nurse Training
advertisement

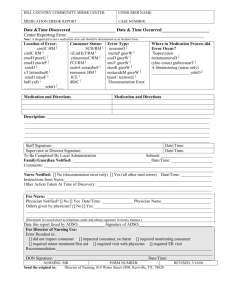
Wendy Hawkesworth – A Curriculum for Nurse Training (Supplementary Papers) Module 1: Awareness of judgements Introduce In- practice reflective template to inform clinical decision making at the time. To be used during education and within clinical practice as part of ongoing supervision post education. In practice reflective template Comments Awareness Reasoning Communication Knowledge 1.1 Admission Scenario John* is a 35-year-old man living with schizophrenia. His last admission to the inpatient unit was four months ago. He was admitted via his case manager who tells you the following admission details: He was alerted to John’s unit by the neighbours who said that John had been knocking on their door accusing them of listening in to his conversations and poisoning his cat. The case manager had gone around to John’s house that day to see what was happening but John refused to let him in. He informed John that he would like him to see the psychiatrist for an assessment. John refused to talk to him shouting abuse and accusations about him being in allegiance with the neighbours. He called the police who are escorting John to the unit under the mental health act. John is not resisting this show of force. It is not an uncommon occurrence that people are admitted to the unit under highly charged conditions. What picture do you have of John from this information? (Assumptions are a normal part of how we understand the world around us. Information is judged according to the values we hold this is influenced by our past personal and professional knowledge. Being mindful of our judgments is a way we can consider others point of view). What assumptions do you make about John? What are these assumptions based on? Think about your past personnel and professional knowledge how are these influencing your thoughts? What other information do you need? Complete reflective template. Clarifying assumptions: It may help to think of the reason why John maybe thinking this? Have another look at the scenario. What do you think John’s values may be? What questions would you be putting to the case manager around what is happening for John? Think about the medical perspective - What is known about stress vulnerability and psychosis? John’s perspective I am scared. The voices are so strong. They are calling me a filthy person… that I shouldn’t talk to anyone. My voices are getting worse. I can’t concentrate any more they have been waking me up at night I haven’t slept for two weeks I know the neighbours have been watching me they have been knocking on my door asking if I am ok but I don’t want to talk to them they were the ones that called the police last time I was admitted. My case manager came snooping around banging on the door wanting to take me away. I am not letting him in. I have no one to talk to I haven’t been to my club house stepping stones for a week. I haven’t seen my cat for three days they must have poisoned her. Does this change your picture? 1.2 Therapeutic communication It may be the case that at this time the person with schizophrenia may not be in a position to articulate his feelings in such a concise way as this. What is your experience of this? The concern is the other perspective is either ignored or pathologised where it isn’t understood. Being mindful of this allows a seeking of further information /clarification or acceptance of being unclear at this time. Recommendations: Communicate in a way that attempts to meet where the person is at Slow down Avoid pre-judgments Attempt to understand Gather information from other sources .There may be other folks that can add light on the picture Mindful of only working from one perspective. Is there anything else that you have found which helps with this? Language Is there anything that strikes you about the language in the scenario? What does “show of force” mean? (Challenge the idea that this is akin to control) Is this what mental health nursing is about? What other language do we use that relates to control? (e.g. “take down” , “lock down” ) What is the alternative language that can be used? Module 2: Admission to the ward The result of human reasoning is context dependent. The structure of memory not only the long term storage organization (what do I know) but also current context (what is in focus at the moment).We believe that this is an important feature of human thought not an inconvenient limitation (Hubert Dreyfus, social researcher) John is admitted to the ward .The nurse who does the admission is David. David is a 42 year old nurse that has worked in the inpatient unit for two years. David has two teenage children from his second marriage. He used to work as a manager in a correction facility but left to work in mainstream acute psychiatry because he wanted to work closer to home. David has nursed John before and has seen John when he is well. John remembers David and is pleased to see him. David is nearly at the end of his shift. He offers John a cup of tea, shows him to his room and says ok let’s get down to it. “It’s good to see you John I am sorry that you have been admitted again. It sounds like you have been having some trouble with the neighbours? Everywhere is the same as before. Do you remember where the bathroom is? OK Now I need to do a quick risk assessment for our record and ask you a few questions and then I’ll leave you to it.” David conducts the risk assessment. Do you hear voices? Are you feeling suicidal? At this point John stands up and starts yelling. “Now calm down mate” “I do not want to be here I am not unwell I need to leave” “Look you’ll be ok. The doctor will see you soon I just need to fill in these forms and then I’ll have finished.” John is getting increasingly angry. What is happening within this communication? Discuss the relationship of communication and risk. What is the risk for John? Consider this in light of Support the persons wellness through a process of care based on sharing and support . 2.2 A shared approach Discuss Three Keys to a Shared Approach (2008) 1. Active participation, with key folks including service providers and carers 2. Different provide perspectives, within an MDT 3. Person centred perspective building on strengths, resilience and aspirations as well as needs and challenges How can David connect with where John is coming from? Write down a conversation that you think David may have with John that may show a shared understanding. (getting close to the subjective ) Understanding the person’s perspective from a narrative (rather than reductionist) point of view. Empathising with John’s position is a way of finding a shared understanding. This doesn’t mean you have to agree or go along with John but it puts you in a better space to work with where John is coming from. What would you feel like if you had been brought in by the police? If you thought you did not have a mental illness and yet you were being told that you did? Have you ever been accused of something that you do not believe? 2.3 Balancing science and values A balanced approach: What options does David have around the process of admission? Emphasis on the process rather than the task If someone is unwell, particularly in a crisis situation, they may not be able or want to be actively involved in how their problems are being assessed. Rather, assessment should be ongoing so that an individual can bring in their own understanding of their problems when they are well enough to do so. Cameron walks past. Cameron is one of the consumer companions. You ask Cameron if he can be with John a while. John feels more at ease with Cameron. Provide a choice of clinician wherever possible: Most people select as confidents people who share their own values, beliefs and experiences. (Fehr 1996) 2.1 Recording information Documentation David writes down: difficulty with engagement, angry, resistive, concerned that he will leave the unit cannot agree on his safety to be nursed on a constant observation high risk of AWOL. Complete a reflective template. What is missing in this documentation? What would the documentation look like if it was to reflect a shared approach? What is John struggling with? What are his difficulties? What are his needs and what are his strengths, resources and aspirations? Handover What information would be included in the handover as a result of this thinking? Module 3: Dining room - Analysis of knowledge influencing practice Dining room (Scenario 1) It is a Tuesday morning and you are the clinical Nurse in charge of a busy shift at the hospital. You have five nurses working on the shift, one of which is agency and the others regular staff. There are ward rounds, ECT, escorts to x-ray and discharges to be arranged. The ward is full to capacity and there are a couple of folks waiting in ED to be admitted. It is 8am in the morning time for breakfast and medications. It is practice for staff to be in the dining room. Today there are four staff in the dining room talking about their day ahead and observing consumers interactions. 3.1 Questioning practice What is the reason for observing meal times? Whilst walking through the dining room you over hear Sue who is one of the nurses telling another nurse that John has been observed to be responding to voices and has been jumping up and down from his seat and going to other consumers and shouting. She is concerned about him disrupting the others. She asks the nurse to keep a watch on him whilst she goes to get some extra medication. You talk to Sue about her decision. She says her reason for deciding to give John medication is that he is decompensating in his mental state that she is concerned that he will disturb the others that he is escalating and needs to take medication to calm down. 3.2 Ethical reasoning What are the ethical reasons behind the decision? Beneficence Maleficence Autonomy Justice Is there any other knowledge that could be included? Complete a reflective template to consider your response. Knowledge about the situation Knowledge about John’s perspective. What might be the organisational, professional and personal values that drive Sue to make this decision? If Sue was more informed of the reason for John’s behaviour would her decision have been different? What knowledge of psychosis is driving Sue’s thoughts at this time? How is John’s behaviour viewed? How do we come to know about this behaviour? (interpretation and observation) What is it within this medical knowledge frame that the nurse is basing her decision on? Comes to the above conclusions through medical professional knowledge, an interpretation of the person’s behaviour as an internal problem fixed by medication. Is the nurse balanced in her decision making? Balance between a problem base versus an understanding perspective. How does this fit with a recovery approach? What is the evidence around medication with the person who is psychotic? What happens next? In between the nurse getting the medication, John walks over to a table away from the window and sits down on his own. One of the nurses brings his breakfast over. He continues to talk to himself however he is focusing on eating his breakfast rather than shouting at others. Is this significant? (Dynamic reasoning) 3.3 Case-based reasoning Discuss case based reasoning as a compliment to principle based reasoning. Do you think this change in behaviour should be considered? Why would it not be considered? What was the consequence of this? Ignoring the consumer values can lead to conflict. Refusing medication The nurse approaches John with the medication. She says, “Here John, take this. It will make you more settled” “I don’t want that. I am fine. Take it away,” John replies. The nurse reiterates to him, “No John, you are unsettled and you need to take this. It will help you to settle. Please take your medication, John it will help you” “No. I don’t want to take it. I am fine.” John’s response is to shout at the nurse, that he is not going to take that, that he needs to speak to someone in higher authority. He is sick and tired of being pulled and pushed from pillar to post in this place whilst all the nurses do is to control and talk about him. “You take it if you need it, I am not having it.” Concerned that he is becoming more agitated and disturbing to the other consumers, the nurse says that he needs to take this to calm down and if he doesn’t take this medication, she will have to call security and give him an injection. What has happened? What could have been the demands on the nurse at the time? What are the barriers to finding shared understanding? How could this have been different?