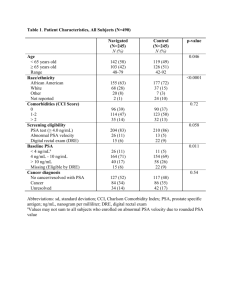
Supplementary Chart 3. Characteristics of the included

Supplementary Chart 3. Characteristics of the included observational studies
Support and conflict of interest/ Registrie´s inclusion criteria
SAAD 2009 [26] and SAAD 2010 [27, 28]
British Society for Rheumatology Biologics Register
(BSRBR) receives restricted income from Abbott
Laboratories, Amgen, Schering-Plough and Wyeth
Pharmaceuticals
Subjects included in the study were selected from the
BSRBR.
The BSRBR aims to recruit patients with rheumatic diseases receiving anti-TNF therapies in the UK.
The register does not have any exclusion criteria other than patients must be registered within 6 months of starting therapy.
From 2002 to 2006, the BSRBR recruited patients starting anti-TNF therapies for PsA.
The analysis was restricted to subjects with a physician diagnosis of PsA who had started treatment with etanercept, infliximab or adalimumab.1
Study´s inclusion and exclusion criteria
The British Society for Rheumatology guidelines for
PsA published in February 2005 recommend that anti-
TNF drugs should be reserved for patients with active
PsA:
≥3 tender joints and ≥ 3 swollen joints despite adequate therapeutic trials of at least two standard DMARDs individually or in combination
VIRKKI [29]
The ROB-FIN register was supported by Abbott,
Roche, Schering-Plough, UCB and Wyeth
Study founded by Victoria Foundation, Wilhem and
Else Stockmann Foundation, Waldemar von Frenckell
Foundation, Finska Lakaresallskapet, perklen
Foundation, Sigrid Jusélius Foundation, EVO grants and the TBGS National Graduate School of
Musculosckeletal Disorders and Biomaterials.
Inclusion in the ROB-FIN register requires informed consent from the patient receiving biological therapy for inflammatory arthritis.
Patient selection for biological therapy of PsA with peripheral arthritis has, presumably, been based on the
Finnish evidence-based treatment recommendations for
RA, but with modification based on the clinical judgment of a specialist to accomodate individual patient needs:
Having swollen and tender joint counts ≥ 6,
+ morning stiffness > 45 minutes and/or erythrocyte sedimentation rate (ESR) ≥ 30 mm/h and/or
C-reactive protein (CRP) ≥ 28 mg/l,
Therapeutic regimen
During the study, etanercept was administered as a subcutaneous injection of 25 mg twice weekly or 50 mg once weekly; adalimumab was administered as a subcutaneous injection of 40 mg every 2 weeks; infliximab 5 mg/kg was administered at weeks 0, 2, 6 and 8, and then every 8 weeks thereafter
It was recommended that infliximab be administered in combination with MTX.
At the time of initiation of the anti-TNF therapy, the rheumatologist or rheumatology nurse specialist completed a consultant baseline questionnaire .
Each patient completed a patient baseline questionnaire, including quality of life assessments.
The rheumatology consultants/nurse specialists were sent a 6-monthly postal follow-up questionnaire for 3 years and then annual follow-ups thereafter.
Treatment and follow-up occured mainly in outpatient rheumatology clinics of central or regional hospitals.
Continuation of treatment was warranted if he/she responds favorably to the biological drug, reaching
ACR50 response by 3 months of therapy.
The register data are provided by Finnish rheumatologists on a continuous, regular basis using structured forms available from the Website of the
Finnish Society for Rheumatology.
Reporting occurs at baseline and subsequently at prespecified intervals during therapy (at 3 and 6 months, and semiannually thereafter), and on discontinuation of therapy
Support and conflict of interest/ Registrie´s inclusion criteria
Patients starting biological therapy between June 2000 and February 2006 were included in the study (1) if the patient had been diagnosed with psoriatic arthritis; and
(2) if a baseline report, i.e., patient demographic data and disease profile at commencement of biological therapy, had been filed.
SAOUGOU [30]
No information on support
No conflict of interest section
A cohort of 221 patients with PsA was followed up in
University of Ioannina, Greece.
From these, 65 patients with severe PsA and recalcitrant severe psoriasis were recruited between
January 2003 and December 2003.
All patients fulfilled the European Spondyloarthropathy
Study Group criteria (ESSG criteria) and were refractory to at least 2 DMARDs.
Study´s inclusion and exclusion criteria
+ response to conventional DMARD and combinations thereof is not satisfactory
At the time of enrollment, patients were required to have active PsA: presence of 5 swollen or 5 tender joints (based on joint counts of 66 and 68, respectively)
+
C-reactive protein (CRP) level 10 mg/L and/or morning stiffness lasting 45 minutes or longer, and/or active psoriatic plaque 2 cm in diameter and negative results of serum tests for rheumatoid factor.
Patients were excluded from this study if they had evidence of latent or active tuberculosis (that is, they had to have clear chest radiograph findings and a negative purified protein derivative skin test) or if they had chronic or clinically significant infection, malignancy, or congestive heart failure.
CHASTEK [31]
Immunex and Wyeth
Authors declared conflict of interest
This retrospective cohort study used administrative claims data from a large, national United States (US) commercial health plan affiliated with
OptumInsightTM.
Patients were followed for up to 24 months, with response assessments at 3, 12, and 24 months of therapy
Therapeutic regimen
Patients were treated with either etanercept (25 mg subcutaneous injections twice weekly) or infliximab (5 mg/kg) at weeks 0, 2, 6, and every 8 weeks thereafter for a period of 5 years.
If the clinical response was insufficient, the interval between the infusions was shortened to 6 or 4 weeks.
Moreover, patients were treated with adalimumab subcutaneously (40 mg every other week).
To be eligible, patients were adults (age 18–64 years) at the time of therapy initiation, were continuously enrolled in the health plan for at least 6 months before and at least 12 months after initiation of therapy, and had at least one claim with a diagnosis of PsA (ICD-9
696.0) from 6 months before through 30 days after therapy initiation.
Patients were followed up every 2 months and safety evaluations (including adverse events) and data concerning efficacy, tolerability, concomitant therapy, and drug discontinuation were recorded.
The initial TNF-blocker dose was defined as the average weekly dose of the initial prescription fill based on the quantity, drug strength, and number of days’ supply. Patients were categorized according to their initial weekly dose of etanercept (50mg weekly, <50 mg weekly, or other) or adalimumab (40 mg weekly,
40mg eow, or other).
Gaps in therapy were defined as the time between the
Support and conflict of interest/ Registrie´s inclusion criteria
The Life Sciences Research Database (formerly the
Ingenix database) comprises fully adjudicated medical and pharmacy claims for over 27 million adults across the US.
Patients with a diagnosis of PsA who started therapy with etanercept or adalimumab as index therapy between January 1, 2006 and December 31, 2008 were included in the analysis.
BONEFEDE [32]
No information on support
Authors declared conflict of interest
This is retrospective analysis of data from the Truven
Health Analytics MarketScan Commercial Claims and
Encounters (Commercial) and Medicare Supplemental and Coordination of Benefits (COB) Research
Databases.
These databases include enrollment data from approximately 150 large employers and health plans across the US, which provide private healthcare coverage.
Patient´s first claim for either etanercept or adalimumab was their index claim, and this defined their index agent. The study period was between July 1, 2005, and
September 30, 2010
Study´s inclusion and exclusion criteria
Patients were excluded from the study if they had a diagnosis for which TNF-blockers are often used during the 6 months prior to therapy initiation, through disenrollment or end of study.
Patients with cancer or human immunodeficiency virus infection were also excluded.
Patients could not have had etanercept or adalimumab administered in a physician’s office (evidence that the patient did not self-administer medications) or have a claim for other biologics during the 6 months prior to therapy initiation.
Adult (≥18 years of age) patients with psoriasis, psoriatic arthritis or both, who initiated therapy with etanercept or adalimumab and who had medical and pharmacy benefit eligibility ≥6 months prior and ≥12 months following initiation of treatment, were included in the analysis. Patients were followed for 12 months after their index date.
Patients were biologic-naïve for 6 months prior to their index claim.
Patients with cancer or with another indication for which etanercept or adalimumabe could be prescribed were excluded.
Therapeutic regimen run-out of a fill until the date of the next prescription refill.
Gaps in therapy of at least 7 days (pauses in therapy) were identified.
Pauses in therapy were not identified following the last prescription fill.
The FDA-recommended doses for etanercept are 50 mg weekly administered subcutaneously .
The recommended doses for adalimumab are 40 mg eow subcutaneously.
The initial dose was the average weekly dose of the index prescription fill.
Gaps in therapy were identified as the time between the run-out of a fill until the date of the next fill.
Persistence to index medication was measured as the number of days from the index date to either the date of a switch toanother TNF-blocker or a gap in therapy ≥45 days over the run out of the fill (fill date plus days supply), whichever came first.
Patients with a ≥60-day gap who did not have a subsequent claim for any biologic approved for either psoriasis or psoriatic arthritis during the 12-month follow-up period were considered to have discontinued index medication.
Time to restarting or switching to another biologic was calculated as the total number of days from the index date until the time that a patient restarted or switched therapy; patients who did not switch therapies
Support and conflict of interest/ Registrie´s inclusion criteria
Study´s inclusion and exclusion criteria Therapeutic regimen or have a ≥60-day gap in therapy were considered persistent on therapy for the entire study period.
DMARD: disease modifying antirheumatic drugs; eow: every other week; MTX: methotrexate; NSAID: non-steroidal anti-inflammatory drug; PsA: Psoriatic Arthritis; TNF:
Tumor Necrosis Factor