Kowalczyk_Chap_3_lInvestigating_Disease_Outbreaks
advertisement

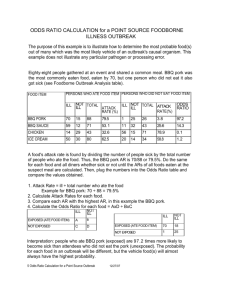
lInvestigating Disease Outbreaks MED 6301- Chp. 3 Dr. John Kowalczyk Spring 2009 lInfectious Disease Process “Chain of Infection” -Infectious Disease Process -Results from the interactions of the 3 components of the epidemiological triangle: -Agent -Host -Environment -Chain of infection includes 6 chain links which all must happen in succession- break any link in the chain, the disease spread will cease Chain of infection-1 Causative Agent: -The entity capable of causing disease -Agents are one of three types: 1.Biological- protozoa, metazoa, bacteria, viruses, fungi, rickettsia 2.Chemical- pesticides, additives, industrial chemicals 3.Physical- heat, light, ionizing radiation, noise, vibrations *note- most diseases are caused by biological agents; chemical and physical agents cause chronic long term illnesses Chain of infection-2 Reservoir of Agent -The normal habitat in which an infectious agent lives, multiplies, and grows (not all diseases have one) -These habitats include humans, animals, and environment -2 major categories of human sources of infection: -Acute clinical cases. Less likely to cause transmission due to early diagnosis and treatment (going to doctor) -Carriers- person who harbors infection but has no overt signs or symptoms Why is a carrier dangerous? Don’t express Sx but spread to others. -Chain of infection-3. -Portal of exit of agent from Host There are 5 means of exit from the human body: 1.Respiratory tract- very common but difficult to control Common cold, Influenza, TB, Airborne droplets 2.Genito-urinary tract- urine, semen Syphilis, Gonorrhea, Schistosomiasis (blood flukeworm inside body, eggs leave thru urine- urinate in the lake; eggs enter skin while wading in water, enters bloodstream 3.Alimentary tract- mostly related to food- by mouth; also vomitus, feces, saliva Rabies- dog bite Cholera-intestinal tract 4.Skin- Superficial wounds- cuts, gashes, burns, puncture wound—or smallpox 5.Transplacental mode (mother to fetus)- pregnant woman passes disease thru placenta-umbilical cord to baby Rubella, Syphilis, Hepatitis B, HIV+ Chain of infection-4. Mode of transmission of agent to new host -Direct transmission (person to person)- touching, biting, kissing, sexual intercourse -Indirect transmission-Vehicle borne (inanimate) blood, water, food, surgical equipment, eating utensils, clothing, etc -Vector borne- feces, eggs, biting (saliva) -Chain of infection-5. Portal of entry into new Host Basically the same as #3- portal of exit Mouth, nose, Skin, Genital/anal, transplacental Chain of infection-6. Host susceptibility -Depends upon: -Genetic factors -General resistance -Specific acquired immunity (natural or thru vaccinations) +skin toughness -malnutrition +gastric acidity -poor health +cough reflex -repressed immune Surveillance of Disease -Entire process of collecting, analyzing, interpreting, and reporting data concerning incidence of disease, injuries, or death -USA- Centers for Disease Control (CDC) federal agency responsible for surveillance activities of acute and infectious diseases -Local and state health departments also responsible on local and state level for surveillance Baseline Data -Endemic levels of disease- usual level of disease in a community -Evaluation of time trends: -Long term secular trends- over time period a disease is looked at to determine trends -Seasonal variation trends- based on route of spread; i.e. respiratory route for influenza is during winter and early spring; insect vectors in summer time for Lyme or West Nile; Epidemic -Disease outbreak at an unusual or unexpected frequency; above and beyond usual endemic level -Pandemic- epidemic outbreak affecting several countries or continents; pandemic flu will likely be pandemic over many countries in the world when it happens -Epizootic- ‘upon animals’- unusual pattern of disease in animal populations Procedures- 5 steps 1. Define the problem and establish diagnosis: determine from outset whether this epidemic (outbreak) is real. What needs to be looked at? -Surveillance - Endemic levels -Foodborne Outbreak Definition -Two or more persons (except for botulism and chemical poisoning it may be only one person affected) -Who all ate the SAME food at the same location….. -AND ALL became ill at about the SAME time, and with the SAME symptoms. -Oh, yeah.. The Poo-Poo Story! Outbreak in residence hall, dinner party, all ate subs, 45/60 sick. Sx 6-12 incubation, V/D, nausea, cramps, headache, Staph aureas infection! Baby poop in kitchen. 2. Appraise the existing data: evaluate known distribution of cases with respect to person, place, and time -Case identification- find all potential cases involved in the outbreak; start with index case- first person to get sick and transmit to others; how did it spread? -Clinical observations- record number, types, and patterns of symptoms associated with disease -Tabulation & spot maps- cases of disease are plotted on a map (Dr. John Snow- Cholera); these can be done by date/time of disease onset of symptoms, geographical clustering; graphing can show time of onset over period of time -Plot an epidemic time curve graph -Identification- determine the responsible agent (biological, chemical, physical)- How? 3. Formulate a hypothesis: -What are possible sources of infection? -What is likely agent? -What is likely method of transmission? (spread of disease) -What is best approach to control the outbreak? 4. Test the hypothesis: -collect data needed to confirm or refute your initial suspicions; -continue to look for more cases; evaluate alternative sources of data; -begin laboratory investigations 5. Initiate Control Measures and Draw conclusions to formulate practical applications -Sanitation -Prophylaxis -Diagnosis and treatment -Control of disease vectors -based on results of investigation, likelihood of new programs, policies, or procedures will need to be implemented -long term surveillance and prevention efforts to prevent recurrence of similar outbreaks Measures of Disease Outbreaks -Attack rate- same as ‘incidence rate’; looking at number of new cases of disease per unit of population per unit of time. -Occurrence of disease in population increases greatly over a short period of time, often related to specific exposure -Attack rate= # ill persons x 100% # ill + # well persons -Attack Rate Table- to find specific food responsible for outbreak A (ate the food) ill not ill ‘A’ total attack rate% ex: 10 + 3 13 77% B (did not eat food) ill not ill ‘B’ total attack rate% ex: 7 + 4 11 64% Identifying Food that Caused Outbreak 1.List all foods consumed at event 2.Persons involved in outbreak: -A (ate food) -B (did not eat the food) 3.Calculate attack rates for each food item with well and ill persons 4.After calculating AR, find difference in attack rates A-B between those who ate and those who did not eat -Identifying Food that Caused Outbreak- cont’d 5.Repeat process for each food item suspected in outbreak 6.Foods that have greatest difference in attack rates may be the foods that were responsible for the illness -Secondary Attack Rate -S.A.R.= Number of cases of an infection that occur among contacts within the incubation period following exposure to a primary case in relation to the total number of exposed contacts -Denominator is restricted to susceptible contacts when these can be determined -Is a measure of contagiousness and useful in evaluating control measures -Secondary Attack Rate Formula SAR%= # new cases in grp - initial case(s) # susceptible persons in grp – initial case x100 Initial case- index case + co-primaries Index case- case that first comes to attention of public health officials Co-primaries- cases related to index case so closely in time- same generation of cases -Epidemic Curve -Defined as a graph in which cases of a disease that have occurred during an epidemic period are graphed according to the time of onset of illness in the cases -Provides a simple visual display of the outbreak’s magnitude and trends -How to Draw an Epidemic Curve -You must first know time of onset of illness -Number of cases plotted on the y-axis (vertical axis) -Unit of time on x-axis (hortizontal axis) -Time is usually based on hours -Show pre and post epidemic period on your graph -Interpreting Epidemic Curve -Consider overall shape- this will determine pattern of epidemic- common source or person-to-person transmission -Curve with steep up slope and gradual down slope indicates a point source epidemic where people were exposed to same agent over brief period of time -Person-to-person transmission spread will have series of progressively taller peaks one incubation period apart -Cases that stand apart are called ‘outliers’ and also should be looked at closely Case: hillside elementary school. Potluck picnic 135 students, 315 parents. – 275 parents & 125 students ate all of the students. 45 students & 65 parents staph food poisoning 90 ate potato salad, 105 ate lasagna, 50 had only drinks. Calc Attack Rate. Food specific AR for lasanga & potato salad. AR: Attack rate= # ill persons x 100% # ill + # well persons total = 450 ill # = 110 AR = 24.4% Food specific attack rate: Lasanga AR = 105/400 x 100 = 26% Potato salad AR = 90/400 x 100 = 22% Denominator – people who ate only Culprit = lasanga had highest AR