Output 3: Improved access to health services in DFID
advertisement

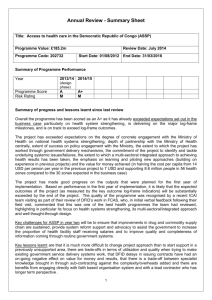
Type of Review: Annual Review Project Title: Accès aux Soins de Santé Primaires (ASSP) Date started: 1 April 2013 Date review undertaken: July 2013 Instructions to help complete this template: Before commencing the annual review you should have to hand: the Business Case or earlier project documentation. the Logframe the detailed guidance (How to Note)- Reviewing and Scoring Projects the most recent annual review (where appropriate) and other related monitoring reports key data from ARIES, including the risk rating the separate project scoring calculation sheet (pending access to ARIES) You should assess and rate the individual outputs using the following rating scale and description. ARIES and the separate project scoring calculation sheet will calculate the overall output score taking account of the weightings and individual outputs scores: Description Outputs substantially exceeded expectation Outputs moderately exceeded expectation Outputs met expectation Outputs moderately did not meet expectation Outputs substantially did not meet expectation 1 Scale A++ A+ A B C Introduction and Context What support is the UK providing? The UK is providing £184.9 GBP million over five years to strengthen basic health service provision in the Democratic Republic of Congo (DRC) in order to improve reproductive, maternal, neonatal and child health (£179.7m), and to strengthen the capacity of the central Ministry of Health to support service delivery (£5.2m). The programme will build on DFID’s proven track record of improving access to health care and delivering health results in the DRC as a result of its previous Access to Healthcare programme, which ended in March 2013. The programme will support 56 health zones (out of 515) in five of the eleven provinces in DRC, providing at least six million people with access to essential primary and secondary healthcare services. The design phase began in October 2012 with implementation running for five years from April 2013 to March 2018. DFID’s support focusses on engagement at three levels: 1. Engagement with non-state service providers to strengthen public sector health services DFID will continue to strengthen public sector provision of health services by working through non-governmental organisations, civil society and faith based networks to implement this programme, whilst strengthening government health management teams. Funding will allow for subsidisation of user fees, especially for vulnerable groups such as pregnant women and children under five. 2. Engagement with communities and individuals The programme will have an emphasis on strengthening empowerment and accountability at a number of different levels, ensuring that citizens have a greater voice and that both service providers and the government are more accountable for delivering quality basic health services. 3. Engagement with the state Improving basic service delivery is a key entry point to strengthening the social contract in DRC. DFID will focus on strengthening the role of the Ministry of Health to act as an effective steward, provide an enabling environment for service delivery from a range of providers, set policy and manage health information. The total budget for the programme consists of two high-level components: - The bulk of the budget (£179.7 million) is for support for service delivery and health systems strengthening at health zone and provincial levels. This has been supplemented by a contribution of SEK 34 million from Sweden (SIDA), bringing the total to value of this component to £182.9 million. Implementation of this component is being carried out by a consortium led by IMA World Health. - £5.2 million is for a sub-project called Renforcement des Capacités Institutionelles (RCI), to provide capacity building and technical assistance to the Ministry of Health at central level. This will focus on key stewardship/policy functions with a strong emphasis on strengthening public financial management, for example in budget planning and execution and strengthening information systems. Whilst this new programme builds upon DFID’s previous Access to Healthcare programme, it also differs from it in a number of key ways: 2 Greater focus on strengthening empowerment and accountability, to contribute to a more responsive government and potentially a stronger social contract. Greater emphasis on working through Faith Based Networks to support service delivery. More support to strengthen the Ministry of Health, by strengthening links between the provincial level, health zones and health centres, providing technical assistance in key areas such as public financial management, and strengthening the use of information for oversight eg through the national health information system (SNIS). Increased geographical coverage: the programme will support 56 health zones, compared to 20 in the previous programme Access to Healthcare. This is partly achieved through increasing our investment, but also by adopting a more costeffective approach which offers better value for money. Shift to a “managed programme” approach: rather than directly working through individual NGOs, we will provide our support through a consortium of organisations led by IMA World Health. This will facilitate a more coherent approach across the programme and provide a mechanism for closer quality assurance and cost monitoring. Better use of evidence: operational research / impact evaluation features prominently in the programme, allowing it to learn and adapt during implementation, and to contribute to policy engagement. What are the expected results? This programme will aim to provide life-saving essential primary health care to at least 6 million people over 5 years, with an emphasis on reproductive, maternal and child health. The programme will support 56 health zones (out of 515) in five of the eleven provinces in DRC. In addition to delivering health outcomes and health facilities/zones with better capacity, the programme will also support the government to be a more effective steward/provide an enabling environment and seek a stronger social contract through empowering citizens to hold both the government and non-state providers of health care (such as faith based organisations) to account. Impact: Improved reproductive, maternal, neo-natal and child health (RMNCH) in the Democratic Republic of Congo. Outcome: Increased coverage with essential reproductive, maternal and child health services in DFID-supported health zones target areas. Key results: This programme will deliver the following key results in target areas by the end of 2014/15: Reduce U5 mortality by 50% in target areas: o Vaccinate 64,600 one year olds against measles each year. 3 Improve reproductive and maternal health: o Provide contraception - 155,000 CYPs (couple years protection) cumulatively by 2014/15 and 355,000 CYPs by the end of the five year programme. o Ensure that 75,000 births per year are attended by skilled health personnel. o Make sure 100% of health facilities in target areas offer appropriate emergency obstetric care. o Provide 75,000 pregnant women with Intermittent Presumptive Treatment (IPT) for malaria during ante-natal visits. Provide 600,000 people with access to clean water and sanitation. The programme will also deliver additional benefits such as improved nutrition, enhanced empowerment and accountability, and institutional capacity building. What is the context in which UK support is provided? The DRC is the poorest country in the world according to the 2011 Human Development Index. Three in five of its 65 million people live on less than $1.25 (£0.80) per day. The DRC has some of the worst health indicators in Sub Saharan Africa. With one fifth of children born not reaching their first birthday, the DRC has the second highest level of child mortality. It also has the fourth highest level of maternal deaths, accounting for almost one in ten of all maternal deaths in Africa. Access to health services is extremely limited. It is estimated that less than a quarter of citizens have access to healthcare across the country. Some of this lack of access is related to the barrier of cost since user fees are the norm. DRC remains affected by conflict and fragility which continues to impact on the health system. This is a complex environment to work in with many challenges. But better access to basic health services and strengthened empowerment and accountability can have a positive impact on both recovery from conflict recovery and preventing further conflict. Government financing to health care is extremely limited and as a result the Ministry of Health takes very limited responsibility for the provision of salaries and other resources required for public service provision. Per person per annum, the government contributes $2, donors $4 and households $6. There is a strong link between subsidising care of vulnerable groups and delivering improved health outcomes. DFID will continue to ensure that user fees are not a barrier to care and will have a strong focus on operational research and evaluation so that findings can feed into policy discussions with the government and other donors. DFID has invested heavily in capacity building of government facilities/health zone management teams through international NGOs. However the government is unlikely to be able to take over running these facilities in the medium term, particularly while salaries and drugs remain unfunded. Faith based networks are likely to remain key to sustainable service delivery, supporting half of public sector delivery and co-managing health zones. Continued support through these networks is required to improve access to healthcare and public sector provision as a whole. DRC has potentially strong human resources in health and a strong public health approach so there is great potential to deliver good health results. 4 In general, donor support remains fragmented in DRC and DFID will work more closely with other donors to ensure coherence of support nationally. DFID’s comprehensive approach has strong support from the Ministry of Health and is in line with DRC policy, and there is good evidence that it is more cost effective in terms of averting Disability Adjusted Life Years. If DFID were not to continue support to healthcare it is expected that the results achieved by DFID over the past three years would be reversed, ultimately dropping back to the much lower levels of access to health services in the health zones concerned. This would contribute to compromising DRC’s progress towards Millennium Development Goals 4, 5 and 6. Unfortunately, the Government of DRC is not yet in a position to ensure that gains made under donor-funded interventions can be sustained. 5 Section A: Detailed Output Scoring Although the business case for this programme was approved in July 2012, implementation started in April 2013, in order to allow for the procurement process and a design phase to take place. As a result, at the time of this first annual review only three months of implementation have occurred, and baseline surveys have yet to be completed. For this reason, insufficient time has elapsed and no data are yet available to allow the progress of the programme to be meaningfully assessed against the logframe indicators. However, such an assessment will be possible at the next annual review: by then the baseline surveys will be complete, and data will have been collected against a full year of implementation. Output 1: Enhanced health service delivery and quality in DFID-supported health zones Unable to assess at this stage (baseline) Output 2: Increased empowerment and accountability in health service planning and delivery in DFID-supported health zones Unable to assess at this stage (baseline) Output 3: Improved access to health services in DFID-supported health zones Unable to assess at this stage (baseline) Output 4: Increased and sustainable access to safe drinking water, improved sanitation, hygiene education and better environmental health in rural and peri-urban communities Unable to assess at this stage (baseline) Output 5: Enhanced government capacity for key functions (RCI programme) Unable to assess at this stage (baseline) 6 Section B: Results and Value for Money 1. Progress and results 1.1 Has the logframe been updated since last review? IMA have proposed changes to the logframe, and the milestones now need to be completed and updated in view of the larger number of health zones than originally anticipated, and the outcomes of the design phase. This should be done through a joint working session between DFID and IMA in the coming weeks, and given the scale and complexity of the programme should ideally be supported by the DFID drawdown function for logframe reviews. 1.2 Overall Output Score and Description: Unable to assess at this stage (baseline). The overall progress of the programme is on-track, and for this reason an interim output score of A is applied. 1.3 Direct feedback from beneficiaries During the design phase, the design team met and consulted with a wide range of political authorities, health management teams and civil society representatives. In total, three Governors, four provincial Ministers for Health, four provincial Medecins Inspecteurs, five Medecins Chefs de Districts, 58 health zone management teams, 20 religious leaders and 11 civil society organisations were consulted. Feedback from the central Ministry of Health on the progress and approach of the programme has consistently been positive. MoH have been closely engaged in the design and early implementation of the programme. It is anticipated that the Ministerial Decree to formally establish the steering group for the programme (with joint membership from GoDRC, donors and IMA) will soon be signed. Limited direct feedback on the programme is currently available from political authorities at the provincial level, or from provincial and health zone management teams. During the field visit to Maniema and Province Orientale, there was evidence that provincial and health zone authorities and management teams do not yet have a sufficient understanding of the programme, the manner of its implementation (and how this differs to that of the previous programme), and their role in this. No direct feedback from service users is yet available for this first annual review. For future annual reviews, it is anticipated that this will become available through the operational research / impact evaluation and community empowerment and accountability components of the programme, as well as less formally through direct interaction with service users and the wider community during field visits. 1.4 Summary of overall progress Overall progress achieved by ASSP since approval of the business case is as follows: - A procurement process has been carried out in order to identify the lead implementation partner for the programme, according to OJEU procedures. This resulted in the selection of IMA World Health as the lead implementation partner, in consortium with technical partners who will provide specific expertise for key aspects of the programme such as reproductive health and operational research / impact evaluation. Further detail of the procurement process is provided in the section on value for money. - The programme has undergone a design phase, in collaboration between the programme consortium (IMA World Health and its partners), DFID and the Ministry of Health. This involved identification of the health zones to be supported, visits to four of the provinces involved in order consult with stakeholders and assess needs, and preparation of plans for implementation. - The institutional arrangements for the programme are now largely in place: o IMA World Health have selected the implementation partners that will provide direct support to health service delivery at the level of individual health zones, and have put into place sub- 7 contract with these organisations (World Vision in Equateur, SANRU in Kasai Occidental, Caritas Congo in Province Orientale and Maniema, and IRC in South Kivu). o Programme staff have been selected by IMA and its consortium partners, and all but a few posts (eg a WASH lead, a gender lead and a healthcare management information systems specialist) have been filled. o The programme steering committee (with membership form DFID, IMA and MoH) has not yet been established, but the MoH is currently preparing an Arrête Ministeriel for this purpose, and in the meantime there have been regular joint meetings between the parties to monitor and guide the design and early implementation of the programme. - A systematic situational analysis of the health zones and facilities that will be covered by the programme has been carried out. This offers a valuable repository of information for detailed planning, and for documenting the achievements of the programme. - Medical supplies, vehicles and equipment are being procured, and this has been a key activity during the early stages of the programme. o To date, IMA have been managing procurement directly, through international suppliers. This is considered a largely interim measure in order to maintain continuity of supplies in existing health zones and across the programme as a whole, whilst the capacity of national drug procurement agencies and depots (under the FEDECAME system) is strengthened. Over time, IMA plan to progressively transition from international procurement to procurement through national agencies and depots. With this in mind, IMA have conducted an assessment of the capacity of these facilities in each of the programme areas. - Health facilities in need of construction or rehabilitation have been systematically identified. Construction has not yet commenced, but there is evidence that planning for this has progressed well. o At present, IMA plan to build 350 health centres and to rehabilitate a further 323 (120 health centres have been identified as not being in need of rehabilitation). o IMA have proposed modifications to the government-approved plans for health centres, and are preparing architectural plans of these for confirmation. - Good progress has been made in strengthening data systems for health service management, and there are strong signs that this has been taking place in close collaboration with MoH: o DHIS2 has been adopted by the Ministry of Health (pending final sign-off by the Minister) as the software platform for healthcare management information systems (HMIS) and fifteen individuals from the Ministry of Health have been trained in its use. o Planned next steps include supporting the configuration of DHIS2 to meet the specific HMIS needs of DRC, provision of IT equipment to health zones, training of health zone management teams and healthcare workers, and piloting of the system in health zones and provinces supported by ASSP. Renforcement des Capacités Institutionnelles (RCI) The RCI project was approved alongside ASSP, but is being managed separately. The project seeks to improve core functions of the Ministry of Health such as stewardship/leadership, facilitating an enabling environment for service delivery (from a range of providers), policy setting, implementation/ quality control and information management. The total budget for RCI is £5.21 million over the period 2012/13 and 2017/18. £1.3 million has been allocated to support the Demographic Health Survey (see below), and further interventions to strengthen Ministry of Health capacity are currently being identified. Demographic Health Survey (DHS) The Demographic Health Survey entered implementation at the beginning of 2013, after delays during the planning process. DFID is providing its contribution to the DHS through a Memorandum of Understanding with UNICEF. The Minister of Plan chairs the steering committee on a quarterly basis and this meeting is attended by other donors and ICF Macro, the technical partner for implementation of the DHS. A technical committee also meets once a fortnight to discuss operational issues. 8 The pilot survey has been undertaken and fully evaluated. The findings of the evaluation will be used to refine the methodology and survey tools. Currently, field workers are being trained in using the tests for biomarkers. The survey will formally commence in August 2013 and is due to be completed by end June 2014. This coincides with the termination of World Bank and USAID funding and will allow for reporting against the 2015 Millenium Development Goals. 1.5 Key challenges Community empowerment and accountability During the design phase, the plans that were developed for the community empowerment and accountability component of the programme were not felt by IMA and DFID to be sufficiently strong to proceed with in their current form. For this reason, IMA elected to not to continue with its consortium partner for this element, but instead to develop their own proposals for community empowerment and accountability. This was agreed to, on the understanding that the default option would be to install a new technical lead for this crucial area of the programme, if IMA’s own proposals are not themselves felt to be sufficiently robust. These proposals have recently been received and are being considered. Procurement and distribution Although procurement of medical supplies and equipment have taken place fairly smoothly since the start of the programme, there have been difficulties, particularly in relation to distribution of drugs to existing health zones: - There have been stock-outs of Artemisinin-based Combination Therapies (ACTs, for treating malaria) in Maniema. IMA have reported that this was due to insufficient production to meet demand from ASSP and other programmes, and anticipated that supplies would once again become available within a week (and would be flown into Maniema to minimise further delay). - Also in Maniema, whilst other drug supplies have been arriving in that province, there have been delays in distributing these on to health facilities, resulting in stock-outs. The reasons for this are not clear, but it seems that imperfect communication between IMA and its implementing partner in Maniema (Caritas Congo) may have played a part. Current information is that stock-outs have also occurred in Kasai Occidental. 1.6 Annual Outcome Assessment The outcome for this programme is “Increased coverage with essential reproductive, maternal and child health services in DFID-supported health zones”. It is too early to assess the programme in relation to the achievement of its outcome. 2. Costs and timescale 2.1 Is the project on-track against financial forecasts: Yes. To date, approximately 4.5% of the budget has been spent, in the course of the design phase (October 2012 to March 2013) and the first quarter of implementation (April-June 2013). This first quarter represents 5% of the total duration of implementation. On this basis, the programme is on-track to remain within budget over its lifespan, particularly as a number of costs (supplies and equipment, salary supplements) are relatively front-loaded into the earlier part of the programme. 2.2 Key cost drivers The table below presents spending of the programme to date, including on the design phase (ie from October 2012 until present). So far, £8.1 million has been spent out of a total budget of £182.9 million. The major cost drivers have been procurement of supplies (drugs, mosquito nets, equipment), vehicles, solar panels, staff costs and management fees. A disproportionate amount of spending has taken place on supplies, vehicles and solar equipment, which is explained by the front-loading of procurement of these items as full implementation is prepared for. Conversely, little has been spent on construction or on Village Assaini (water and sanitation), as these activities have not yet commenced. 9 Expenditure to date Percentage of expenditure Medicines, supplies and equipment £4,048,818 49.7% Personnel costs £962,611 11.8% Management costs £685,140 8.4% Solar panels £571,058 7.0% Salary supplements for health staff £364,030 4.5% Transport £169,077 2.1% Storage and office space £158,464 1.9% Construction & Rehabilitation £11,078 0.1% Communications £2,198 0.0% Water and sanitation £0 0.0% Other £1,180,959 14.5% TOTAL £8,153,433 Note: ‘Other’ covers a range of items such as vehicles, training, developing promotional materials and radio messages, management of epidemics and emergency situations and Data Quality Audits. 2.3 Is the project on-track against original timescale: The initial expectation was that early implementation of ASSP would commence during the final part of Access to Healthcare, in order to create a period of parallel implementation that would facilitate transition between the two programmes. In the end, ASSP did not become operational until shortly before Access to Healthcare came to an end on 31 March. This was due to delays in key aspects of the design process, which took longer than expected and had knock-on effects on one other: for example, final selection of health zones was not completed until November; this in turn led to delays in the process for selecting implementing partners, which itself then took longer than anticipated. There have also been delays in finalising plans for certain sub-components of the programme, namely community empowerment and accountability and WASH. Despite these delays, the overall progress of the programme remains on track in relation to the timescale. Implementing partners were selected and in place (albeit under interim sub-contracts) in time for transition at the beginning of April, drugs and other supplies have been procured and have been arriving in-country, and scale-up into new health zones in Kasai Occidental and Equateur – planned to take place in July – is now ready to proceed. 3. Evidence and Evaluation 3.1 Assess any changes in evidence and implications for the project No changes in evidence have emerged that have implications for the programme at this stage. The operational research and impact evaluation component of the programme will generate evidence from the programme itself. This will allow minor or major adjustments to be made as required during implementation, as well as informing wider policy discussions. Key areas where this will take place are in relation to user fees and access to health services, and the extent to which government reforms and payment of healthcare worker salaries will be sufficient to allow the programme to achieve maximum impact. 3.2 Where an evaluation is planned what progress has been made? A substantial operational research and impact evaluation component is planned for the programme, and this is being led by Tulane University / University of Kinshasa. To date, a protocol has been developed for data collection at baseline, midpoint and endpoint, which will enable to overarching impact of the programme to be determined. This includes plans to compare progress in ASSP health zones with that in unsupported health zones, to permit a degree of attribution of change to the programme. Additional operational research protocols are being developed, including for studies to 10 examine the relationship between user fees and other determinants of health service utilisation, and the impact of community empowerment and accountability upon service delivery and quality. 4. Risk 4.1 Output Risk Rating: High 4.2 Assessment of the risk level At this early stage of implementation, the overall risk level for this programme is deemed to be high, for the following reasons: - The large scale and complexity of the programme: ASSP is being implemented by a consortium of no fewer than nine members, and consists of multiple domains (such as strengthening national drug procurement and supply systems, developing data systems for healthcare and human resource management, and community empowerment and accountability). Managing and coordinating these multiple organisations and areas of activity will almost certainly be challenging. - The delivery model for this programme: Avoiding or phasing out the payment of salary supplements (primes) to frontline healthcare workers whilst simultaneously adopting a much reduced NGO presence than was the case in Access to Healthcare gives rise to greater fiduciary risk, as staff have both a greater incentive and a greater opportunity to commit fraud. - The nature of the intervention: The current programme design is based upon a number of assumptions (such as willingness and ability to pay for services). Given that not all of these assumptions will necessarily hold, it is crucial that the programme recognises and tests them, and is prepared to adapt as needed (this includes being able to respond to adverse or favourable changes in context, for example if the Government opted to adopt a policy of gratuité in the health sector). - The operating environment: Most of the areas where the programme will be implemented offer minimal physical and institutional infrastructure to support service delivery or the activities of the programme partners. By way of illustration, it takes two days to reach Punia health zone by road. Whilst these risks are considerable, each is accompanied by potential benefits: - The diverse nature of the consortium brings with it considerable capacity and a broad range of expertise and experience, and the ambitious scope and scale of the programme have the potential to achieve maximum impact through comprehensive support to the health system at scale. - The delivery model reduces the risk of substituting the role of government, and leaves space for provincial and health zone management teams to assume greater responsibility for service delivery. - The intervention has the potential to provide cost-effective support to service delivery, and to achieve an incremental shift towards more sustainable financing of the health system. - With the challenging operating environment comes a high level of unmet need, and potential for positive impact. 11 4.3 Risk of funds not being used as intended The complexity of the programme, the presence of multiple downstream partners, the phasing out of salary supplements for frontline healthcare workers and the large investment in mobile assets (vehicles, drugs, equipment and construction materials) create added risk of misuse of funds in this programme. IMA are a credible partner in managing this risk, and have experience of doing so in similar programmes in DRC. A Due Diligence Assessment of IMA has been performed and this has identified a number of opportunities to optimise the management of fiduciary and other forms of risk in ASSP. 4.4 Climate and Environment Risk During the annual review IMA presented innovative plans for minimising adverse environmental effects of construction, including the use of stabilised blocks as a cheaper, more durable and less damaging alternative to fired bricks. Low-consumption low-smoke industrial and domestic stoves are to be trialled for the sterilisation of equipment at hospital and health centres respectively. IMA have begun to procure solar equipment for health facilities, and plan to install a solar-powered fridge for every two aires de santé in the programme. The climate and environment assessment for the business case anticipated that the programme would present a low level of risk and a medium level of opportunity, and at present there is no evidence that this assessment should change. 4.5 Other cross-cutting issues Conflict and resilience IMA have established from their situational analysis that 69% of health zones covered by the programme have a ‘very calm’ security situation, and 22% have a ‘moderately calm’ security situation. No health zones were identified as being insecure, although in 9% of health zones the security situation was not determined. The programme would benefit from a clear strategy for understanding and responding to the specific risks and causes of conflict in individual health zones and for achieving health system resilience in emergency situations. Gender A gender review was carried out as part of the annual review by participants in the workshop, using the standard DFID DRC methodology. This has ascertained that the programme currently has an amber rating for gender. Criterion Does the programme design include comprehensive analysis of the situation of women and girls? Observations Amber: The programme design includes a degree of analysis of the situation of women and girls, but this cannot be considered to be comprehensive. It was anticipated that this would be included in the baseline situational analyses performed in each of the health zones, but it is not clear that this has been done. There is as yet no specific gender strategy for the programme. Recommendations A gender strategy should be developed, and be based upon comprehensive analysis of the situation of women and girls in the health zones to be supported. Does the logframe include results and indicators relating to W&G, and those that include transformative change? Amber: The logframe includes indicators that relate specifically to women and girls, and disaggregation of indicators by age is planned. However, the current logframe does not fully capture transformative change for women and girls (although utilisation rates disaggregated by gender will do so to an extent). As the community E+A component is further developed, at least one indicator that captures the transformative impact of this for women and girls should be considered for inclusion in the logframe. Does the Theory of Change explicitly refer to W&G throughout? Amber: The proposed revised TOC presented by IMA refers explicitly to women and girls, but does not demonstrate how outcomes for women and girls are expected to be achieved, and what change will occur as a result. A specific theory of change for gender should be developed as part of the gender strategy for the programme. Does programme have elements that seek to address discriminatory socio-cultural norms? Amber: Implementation plans demonstrate some awareness of discriminatory socio-cultural norms, but this is not yet sufficiently systematic, nor is it clear yet to what extent and how these The gender strategy should include an analysis of such norms in the health zones that will be supported, and present realistic plans for challenging 12 will be challenged through the programme. these through the programme. Does programme contain specific measures on adolescent girls? Green: The programme contains specific measures for providing services to adolescents, including sexual and reproductive health services. Plans for meeting the needs of adolescents now need to be operationalized, and should as much as possible be included in the community empowerment and accountability component. The programme should reflect on the extent to which provision of SRH services to adolescents is constrained by the legal framework, and discuss with DFID where there may be opportunities to seek change. Does the programme have appropriate and adequate plans and resources for gender technical support? Green (provided this is implemented): During the annual review, IMA and Pathfinder confirmed that a gender lead will be recruited in the coming weeks, and that this individual will be responsible for overseeing development and implementation of a gender strategy for the programme. A clear job description should be developed, in order to obtain the appropriate scope and level of gender expertise. Do implementing partners demonstrate a strong commitment to gender issues, have adequate gender capacity and a clear gender action plan? Amber: The evidence for this is currently incomplete. A gender lead and a gender action plan are not yet in place, but commitments to these have been provided by the consortium. The level of commitment to gender issues will need to be further assessed at the next and subsequent annual reviews. Are the programme-specific commitments in the Action Plan for Adolescent Girls under implementation? Overall Amber: These commitments have been partly addressed. The commitments need to be addressed in the gender strategy for ASSP. Amber 5. Value for Money 5.1 Performance on VfM measures It is not yet possible to substantially assess performance in relation to specific VfM measures, beyond the extent to which this was done during the commercial evaluation during the procurement process through which IMA was selected as the consortium lead. Unit costs for activities and outcomes will become available for benchmarking during implementation. 5.2 Commercial Improvement and Value for Money There was a strong response to the call for tenders for the contract under which this programme is being implemented. Cost-effective delivery of health supplies and equipment will be a major factor in the success of this programme. IMA originated as a supplier of equipment and their winning bid showed an excellent understanding of procurement issues as well as a strong vision for the programme as a whole. A set of Key Performance Indicators will be used to test performance, and these will be assessed at the next annual review. 10% of the management/technical assistance budget line allocation is contingent on satisfactory attainment these key performance indicators. 5.3 Role of project partners There are currently nine direct project partners in the consortium that is implementing ASSP: - IMA World Health (consortium lead) - Technical leads: Pathfinder (reproductive health), Tulane University / University of Kinshasa (operational research and impact evaluation), HISP (healthcare management information systems) and Intrahealth (human resource information systems). A replacement technical lead for community empowerment and accountability now needs to be identified. - Implementing partners: SANRU (Kasai Occidental), World Vision (Equateur), IRC (South Kivu) 13 and Caritas Congo (Maniema and Province Orientale). DFID’s interface with the programme is primarily through IMA. As consortium lead, the role of IMA is to manage delivery by downstream partners, set the overarching operational framework for the programme, and to manage essential activities such as procurement and infrastructure development. Technical leads are responsible for providing the programme with specific expertise in key areas, and for supporting the implementing partners to deliver in each of those areas. The implementing partners in turn are responsible for directly providing support to service delivery at health zone level. This arrangement has the potential to provide a coherent but flexible approach to service delivery across a large number of health zones, supported by specialist expertise. However, its success will rely upon good coordination and communication between the consortium members, with clear allocation of roles and responsibilities. These relationships are just now beginning to be tested as the programme moves into implementation, and IMA must continue to ensure that they function well throughout. This is a key operational aspect of ASSP that should be regularly scrutinised, including at subsequent annual reviews. 5.4 Does the project still represent Value for Money: Yes. The value for money assumptions set out in the business case still hold. The extent to which they continue to do so will become more apparent over the course of implementation, and will be further examined at subsequent annual reviews. 5.5 If not, what action will you take? Not applicable. 6. Conditionality 6.1 Update on specific conditions Not applicable. 7. Conclusions and actions Overall, ASSP has performed adequately so far, and has met expectations. Although there have been some problems, the transition from Access to Healthcare to ASSP has taken place reasonably smoothly, and the foundations of the new programme are now in place. Significant early progress has been seen in key areas such as procurement, infrastructure and healthcare management information systems. This performance is reflected in an interim score of A (met expectation), pending availability of baseline and milestone data at the next annual review. However, this is a very early stage of the programme, and the coming challenges are considerable: with this comes a high level of risk. The following recommendations for the programme emerge from this annual review: 1. Continued progress is needed by the programme to proactively identify risks and assumptions, and to address these. More effective use needs to be made of theories of change to systematically identify those risks and assumptions. Once these risks and assumptions have been identified, strategies for managing the risks and testing the assumptions need to be further developed, including through operational research and contingency planning. 2. The diversity of the consortium charged with delivering the programme represents a major asset, but also brings with it risks. IMA need to give ongoing high priority to good coordination and effective communication between consortium members, supported by clear definition of roles. 3. Related to this, clear communication of the programme to stakeholders – including to service providers, healthcare workers and communities - is essential if those stakeholders are to develop a 14 sense of ownership of and commitment to it. Over the coming months, IMA should give high priority to articulating the programme and its approach to stakeholders, both directly and indirectly through its implementing partners. At the same time, DFID DRC should seek to maintain as high a level of interaction with provincial authorities as possible, in order to strengthen awareness of the programme at that level and generate commitment to it. 4. Management of drugs and supplies present a further specific area of risk to the programme, as is often the case with programmes such as this. IMA should develop and present an action plan for managing this risk (particularly in Maniema where drug management is thought to particular need of strengthening) in order to avoid stock-outs and minimise fiduciary risk. 5. Community empowerment and accountability is a crucial component of the programme, and finalisation of the plans for this should be considered a high priority. DFID will provide IMA with feedback on its proposals for community empowerment and accountability, and will work with IMA to identify an alternative technical lead if necessary. 6. The logframe needs to be reviewed and updated, ideally with support from drawdown service. 7. A gender strategy should be developed for the programme, as well as a strategy addressing issues of conflict and resilience. 8. Review Process The annual review process consisted of a field visit to Maniema and Province Orientale, followed by a workshop hosted by IMA World Health (with participation by the consortium partners, DFID DRC health, social development and evaluation advisers, and the Ministry of Health). In view of the scale and complexity of ASSP, for the next annual review DFID DRC should consider forming a team of relevant advisers (with additional external capacity if required) in order to carry out a detailed assessment of each component of the programme. 15