Peer group meetings of service users (self-help groups)
advertisement

Review of the concept of TREE (Towards Recovery, Empowerment and
Experiential expertise of users of psychiatric services).
Peer group meetings of service users (self-help groups)
Boevink, W & Kole, M. (2010). Planting (a) TREE: From experience to experiential expertise about
recovery. Not published summary.
Boevink, W. TREE: Towards recovery, empowerment and experiential expertise of users of
psychiatric services.
Boevink W (2006) From alien to actor. Lecture held during The Public Hearing on The Green Paper on
Mental Health, European Parliament, Brussels, June 8; see: ENUSP website:
www.enusp.org/documents/boevink_alien.pdfBoevink, W. (2012). Life beyond psychiatry. In:
Rudnick
Boevink W (2006) Stories of recovery. Working together towards experiential knowledge in mental
health care. (Utrecht: Trimbos-institute). To order: hkatsis@trimbos.nl
Introduction
In collaboration with the Trimbos-Institute (a national research institute for mental health care) a
protocolled program has been developed of how to achieve and organize service users on the basis
of their experiential expertise: TREE - ‘Towards Recovery, Empowerment and experiential Expertise’ by, for and with persons with long term and severe mental health problems. This program has been
researched for its effects on and contributions to recovery goals (publication in progress). TREE is
also a company developed and run by experiential experts. Participants in TREE activities have the
opportunity to develop their own skills as experiential experts.
Wilma Boevink is the instigator of TREE. She is researcher and works for the Trimbos-Institute. She is
also an experiential expert, suffering from a relapse of a psychosis every now and then.
The TREE-program is implemented in quite a number of mental health care services in the
Netherlands.
What will be realized?
-an essential element: clients recover a sense of self and identity
-clients acquire experiential knowledge about recovery, thus building on a new sense of self and a
new identity
All the individual stories together form collective experiential knowledge: knowledge about how it is
to live with mental vulnerability and its consequences. If one is capable of passing on this knowledge
to others in any form, then we use the word experiential expertise. Experiential expertise is essential
for the recovery of persons labeled mentally ill. On an individual level, it helps empower fellow
sufferers in their quest for their own strength(s). On a higher level, it paves the way for user
influence in improving mental health care services.
- the group members become aware of themselves as individuals taking an active role, both with
regard to their own mental health problems and the psychiatric care they use.
-the group members remove the diagnosis, prognosis and associated prescriptions from their selfimage and their way of thinking and acting. This is not the same as denying the reality of suffering.
But it does mean that they exchange the identity determined by their disorder for a self-chosen
identity, for a story told in their own words and for self-determined strategies aimed at finding a way
to control their ongoing vulnerabilities and to keep them under control.
- In the TREE program, participants develop, transform and disseminate experiential knowledge.
They perform these tasks themselves, as volunteers or in paid jobs in the mental health care
organizations where the program is implemented.
- The program promotes user/survivor led change within mental health care organizations towards
recovery-based services.
TREE has an important destigmatizing influence: research shows that the most effective way of
combating stigma is to bring the general public in direct contact with the stigmatized group (‘to know
one is to tolerate one’) {15}. TREE-participants are trained to make and tell their stories to a range of
target groups, among them subgroups from the general public.
How will it be realized?
-the program enables its participants to exchange experiences and offer mutual support.
-It also encourages them to develop knowledge and to use such knowledge by making it available to
others
- TREE-participants are trained to make and tell their stories to a range of target groups, among them
subgroups from the general public. Participants are offered training in constructing stories and
presentation techniques to help them convey recovery stories to other people.
The program consists of:
•
self-help groups and working groups;
•
training, courses and workshops for fellow users and survivors of psychiatry;
•
training programmes for professional caregivers;
•
training for professionals and users together;
•
consulting and coaching of TREE innovations in organizations in mental health care.
The TREE team (nationwide company) has a system of coaching in inter/supervision. Veterans
support juniors and mutual support among all is stimulated strongly. Not just in the recovery selfhelp groups, but also within the TREE team, mutual support and self-help is a powerful source of
resilience. When the TREE program is implemented in a psychiatric institution members of the TREE
team take the lead in close cooperation with local service users.
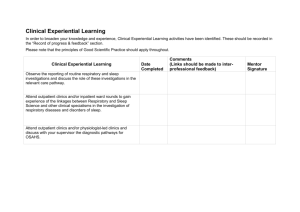
The first phase of TREE interventions in psychiatric institutions consists of TREE team members
visiting patients and telling them our own stories. This is organized by the TREE-team (the company
organized on national level). It is followed by a kick-off meeting where users, family members,
carers, managers and policymakers are invited. What ensues is usually the setting up of self-help
recovery groups. Recovery seminars can be organized for service users with their mentor nurse.
There are training programs both for users and professionals. TREE also experiments with new
formats, like theatre, photography and voice exercises.
Where do professionals have to reckon with (conditions and necessities for actualization)?
Some quotes (where ´our´ or ´us´ is used then this refers to service users)
-In order to help us to identify and use opportunities for recovery, it is vital that professionals in
psychiatry and other mental healthcare disciplines are familiar not only with our past and our hopes
for the future, but also with our ordinary personal circumstances. Our lives do not consist only of the
times when we are “seen” in the consultation room. Recovery takes place outside it.
-It is important that our professional helpers do not take away our hope of recovery. After all, no one
can predict the course that our lives will take.
- Our stories of recovery are not automatically stories of success. Although the recovery concept
seems to be increasingly claimed by people who talk of progress, development, and even cure, our
recovery attempts do not automatically lead to visible progress and improvement. Crises and periods
of apparent apathy may still occur. During these periods it is important that there is someone to help
us to find the meaning of it all. Especially when we ourselves no longer believe in our recovery, it is
important that others help us to regain hope.
- Processes of recovery cannot be represented as one steady upward line on a graph, but rather are
subject to temporary setbacks or what may seem to be a standstill. Allow us these lesser periods. We
need to use such occasions to take stock and consolidate what we have achieved. We cannot
continually chase progress. No one has the stamina to do this.
- We do not need a so-called “treatment relationship”, but rather a relationship of collaboration. A
shared understanding is very important. It is vital that there is a shared understanding of what is
going on. And “shared” does not mean that patients should share in the understanding of the
professional, thus becoming compliant and blessed with this so-called insight into the illness. For
professionals in psychiatry the process of “helping to find the meaning of what is happening” can
easily change into “knowing things better”, particularly when they have little time available and their
case load is too large. “Sharing” actually implies that there is mutual give and take.
Review of the facilitation of the recovery process and how experiential
expertise can be applied in mental health care
As the TREE concept is much more something of service users themselves (but with important
´lessons´ for professionals) I broadened the survey to the question how experiential expertise can be
applied in mental health care. I collected the following white papers, and inventory documents.
Van Haaster H., Wilken JP., Karbouniaris S. & Hidajattoelah D. (2013). Kaderdocument
Ervaringsdeskundigheid [ Framework/Inventory of Experiential Expertise] (herziene versie januari
2013). Kenniscentrum Sociale Innovatie, University of Applied Sciences Utrecht: Utrecht.
GGZNederland. (2009). Naar Herstel en gelijkwaardig Burgerschap. Visie op de (langerdurende) zorg
aan mensen met ernstige psychische aandoeningen [From Recovery to citizenship. the national
agency’s vision on long term care for persons with severe mental health disorders]. Accessed
01082014 at wwww.ggznederland.nl
Den Oude T. Van Oosterum L. & De Leeuw R. (2011). Inzet ervaringsdeskundigheid in de ggz: van
stigma naar succes.[ How to apply experiential expertise in mental health care: from stigma to
success].MGv 66 (7/8); 506 – 517
Droes, (2009). Het alledaagse ongewoon [the ordinary is unusual]. Rob Giellezing.
-----------------------------------------------------------------------------------------------------------------------------------What will be realized (outcomes)?
-vision of the national branch organization of Mental Health Care Institutions (GGZNederland): in the
care for persons with severe mental disorders the perspective of (personal) recovery must be
guiding, but not at the cost of basic care that aims at functioning stable in daily life. Someone’s own
life story must hold a central place. Experiential knowledge must be acknowledged and used. Care
should work towards strengthening the client’s own direction. Improvement in the quality of life is
the ultimate goal. Improvement of the quality of care must be measured regularly. The degree in
which care programs are oriented towards recovery and how successful they facilitate and support
recovery can best be measured with the so-called ROPI-index. Measurement of Outcomes more
generally should include Quality of Life, performance indicators formulated by the national branch
organization and the CQ-index.
How will it be realized?
-How to assist clients in recognizing, improving and supplementing their spontaneous efforts at
recovery?
1.
2.
3.
4.
5.
6.
7.
The professional is ‘present’(theory of presencing) and attentful and responsive to the client.
Give ample space for the input of experiential knowledge and peer contact
Support clients in making their own story and concur with this personal story
Use your professional framework in a reticent and modest way
Have ample attention for causative factors: psychological, social, biological.
Assist clients in finding and using his ‘personal medicine”.
Assist clients in evaluating their own solutions by comparison with alternatives: CBT, how to
8.
9.
10.
11.
12.
13.
cope with voices.
Acknowledge and stimulate the client’s own powers of resilience, individually as well as
collectively.
Assist clients to develop new strategies to cope with phenomena (‘symptoms’) and how to
connect this with recovery goals: Illness Management Recovery (IMR) is a program that can
be used to this aim.
Acknowledge, use and stimulate the support of the client by important others.
Shared decision making for medication and other therapies
Formulating a diagnosis is a collaborate process of finding out what is the matter and should
be concluded with a shared vision.
Professional efforts aim at making suffering more bearable and at strengthening the client’s
own direction and autonomy.
-Experiential experts who work within care teams in mental health care use self-disclosure in their
contact with clients. They tell about their own experiences and their own background and show their
own vulnerability. Experiential experts recognize the experiences of clients, related problems and
the feelings associated with them and they know how to communicate with clients about this. In this
way experiential experts show clients that they are many similarities between them. The exemplary
function of experiential experts helps to break the self-stigmatization of clients. The self-disclosure of
experiential experts makes clients believe again in their own recovery and reduces feelings of shame.
Where do we have to reckon with?
-a basis condition for recovery is meaningful spending your time every day. Therefore having a job
and being paid for it is important. Implementation of IPS (Individual placement and Support) method
in rehabilitation is therefore strongly recommended. Besides finding a job also possibilities of
supported learning must be strengthened.
-Thinking of psychosis as a crisis of meaning and refinding one’s identity. Phenomena can have a
double meaning: for instance woodshedding (withdrawing from contacts to protect oneself from too
many stimuli or inactivity as a negative symptom), low turning points (moments of crisis but also
necessary moments of disintegration followed by integration of the identity at an higher level ). Both
are efforts at recovery and can also be symptoms of schizophrenia (negative symptoms). “A given
characteristic, such as a symptom, may have different functions and different effects at different
times. Processes can have either illness or coping impacts depending on the degree and the context
in which they occur” (Srauss, 1989).
-network approach is necessary: the organization of community support systems in which health care
and other service providers and societal organizations collaborate in order to contribute to better
possibilities of participation in society and also to provide coherent services attuned to needs in all
areas of life.
Competences
Knowledge
-The distinction between the personal recovery process and medical recovery
-The phases in the recovery process: Gagne (2004) distinguishes 4 phases:
1.
Being overwhelmed by the mental health disorder
2.
Wrestling with the disorder
3.
Living with the disorder
4.
Living beyond the disorder
-There is the distinction between experiential knowledge and experiential expertise. Experiential
knowledge can be acquired solely on individual experiences (one’s own history) or can be broadened
and enriched by encompassing collectively built experiential knowledge. We can speak of
experiential expertise when a person has reflected on his experiences and has assimilated them. The
expertise concerns how to cope with your own recovery process, how to deal with professional
caretakers, other carers and family, how to cope with reactions from society and last but not least
how to communicate with peers and be able to support them in their recovery process.
-there is the distinction between experiential expert and experiential worker. The experiential
worker is an experiential expert who works in a professional context, e.g. mental health care.
-experiential workers have various roles, among them: peer support, advocacy, participation in antistigma campaigns, directing peer support groups or working as team member in an ACT-team
(outreaching ambulatory mental health care) or in clinical settings where one can be responsible for
emergency assistance, psycho-education, therapeutic group work etc. (alongside professional
colleagues).
Skills
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
The professional is ‘present’(theory of presencing) and attentful and responsive to the client.
Give ample space for the input of experiential knowledge and peer contact
Support clients in making their own story and concur with this personal story
Use your professional framework in a reticent and modest way
Have ample attention for causative factors: psychological, social, biological.
Assist clients in finding and using his ‘personal medicine”.
Assist clients in evaluating their own solutions by comparison with alternatives: CBT, how to
cope with voices.
Acknowledge and stimulate the client’s own powers of resilience, individually as well as
collectively.
Assist clients to develop new strategies to cope with phenomena (‘symptoms’) and how to
connect this with recovery goals: Illness Management Recovery (IMR) is a program that can
be used to this aim.
Acknowledge, use and stimulate the support of the client by important others.
Shared decision making for medication and other therapies
Formulating a diagnosis is a collaborate process of finding out what is the matter and should
be concluded with a shared vision.
Professional efforts aim at making suffering more bearable and at strengthening the client’s
own direction and autonomy.
Emotional intelligence/attitudes
Salovey and Mayer divided emotional intelligence into four areas of skills: 1) perceiving emotions, 2)
using emotions to facilitate thoughts, 3) understanding emotions and 4) managing emotions.
Professionals can help service users to cope with their emotions and understand them as elements of
a personal story. They need empathic resonance to do so, but they can also support the process of
making sense of their experiences with disease and recovery by facilitating storymaking, for instance
with the IMR/programme (a mix of peer group meetings, educational sessions, etc.).
´Acknowledging´, ´stimulating´ are important emotional interpersonal skills that imply an open mind
for causative factors of mental disorders /symptoms (and how functional they can be) and narrative
competences to assist clients in finding their own story.