Immuno PPT Flashcards Unit 3
advertisement

Immuno PPT Flashcards Unit 3 What is autoimmune diseases? What is the cause of autoimmune diseases? What is central tolerance? How is autoimmunity maintained in the secondary lymphoid organs? Which one is implicated as primary mediators of autoimmune disease? Why is Th1 cells primary mediators of autoimmune disease? Which one react to foreign antigens? What makes an individual more susceptible to a particular autoimmune disease? What other several mechanisms are thought be contribute to autoimmunity? What is the example of antigens that are protected from encountering the circulation are not exposed to potentially reactive lymphocytes? What is the Molecular mimicry refers? What is the last major factor? What is the one B-cell defect in particular? How these defects may enhanced? What are some other defects of the immune system? Which hormone play a role? What affect estrogens? How autoimmune disease classified? What is Systemic lupus erythematosus? Who is more likely to these disease? There is an interplay between ________ Autoimmune diseases is a conditions in which damage to organs or tissues results from the presence of autoantibody or autoreactive cells. The loss or breakdown of self-tolerance brought by several mechanism, including clonal deletion of relevant effector cells and active regulation by T cell. It is the destruction of potentially self-reactive lymphocytes. By a delicate balance between the T helper cell type 1(Th1) and T helper cell type 2(Th20 populations. Th1 cell. Because they release pro-inflammatory cytokines. Th2 response. The inheritance of jean coding for a specific major histocompatibility complex (MHC). The release of sequestered antigens, molecular mimicry, and polyclonal B-cell activation. Sperm. It refers the fact that many individual viral or bacterial agents contain antigens that closely resemble self-antigens. Polyclonal B-cell activation. Fc receptor polymorphisms. By organisms such as gram negative bacteria and several viruses, including cytomegalovirus and Epstein-Barr-virus. The influence of hormones, and environmental conditions. Estrogens. They are known to affect cytokine production and may influence with T cells, either Th1 or Th2, are more active in a particular response. As systemic or organ specific. It is a chronic systemic inflammatory disease marked by alternating exacerbations and remissions. Women are much more likely than men, by a margin of 10 to 1. Genetic susceptibility and environmental. 1 Immuno PPT Flashcards Unit 3 and _________ factor in the development of the disease. Which play a role in presentation of HLA antigens. foreign or self- antigen to T cells and B cells? What abnormalities have also been found Fcy receptors on B cells, macrophages, dendritic in SLE? cells, and neutrophils that bind IgG and prevent excess immune reactions. Is environmental factors important? Yes it is include exposure to ultraviolet light, certain medications, and infectious agents. Is hormones are also important factor? Yes, because they may influence the regulation of genes for SLE expression. What are the clinical signs of SLE? It is extremely diverse, and nonspecific symptoms such as fatigue, weight loss, malaise, fever, and anorexia are often the first appear. What are another symptoms of SLE? Joint involvement, skin manifestations, a classic butter fly rash across the nose and cheeks may develop. What exhibit evidence seen in one-half The exhibit evidence of renal involvement, with to two-thirds of all patients? diffuse proliferative glomerulonephritis, being the most dangerous. What other conditions are develop? It develop include deposition of immune complexes in the sub endothelial tissues and thickening of the basement membranes. _____is the most frequent cause of death Renal failure. in patients with SLE. What other systemic effects may Cardiac involvement with pericarditis, tachycardia, include? or ventricular enlargement, pruritus with chest pains, neuropsychiatric manifestations such as seizures, mild cognitive dysfunction, psychosis or depression, or hematologic abnormalities such as anemia or lymphopenia. What was the first clue in the mystery of The discovery of the LE-cell by Malcolm Hargraves lupus? in 1948. What was the next discovery? SLE, is associated with more than 25 autoantibodies. Auto reactivity of T and B cell leading The production of autoantibodies. to_______. What is one of the main immunologic The constant presence of antigenic material that characteristics in lupus? triggers polyclonal activation of B cells What results from accompanying An enhanced production of certain cytokins that alteration in the function of both Th1 contribute to up regulation of antibody production by and Th2 helper cells? B cells. What does IL-10 trigger? An increase in antibodies directed against DNA. What does IL-10 stimulate to Platelet activating factor produce. When immune complexes are Because of the other possible immune system 2 Immuno PPT Flashcards Unit 3 formed, why can’t they be cleared as usual from the circulation? Why is accumulation of IgG to double stranded DNA seem to be the most pathogenic. How does drug induced lupus differ from the more chronic form of the disease? What are the most common drugs used for drug induced lupus What is the first test performed when SLE is suspected Why is fluorescent antinuclear antibody (FANA) testing used the most. FANA is a sensitive test and easy to use but has low diagnostic specificity, why? What is the percentage that yield false positive results on the FANA test. What is the percent of SLE patients that yield false negative results What is the common practice to screen to avoid low positive titers in the normal population On FANA what does SLE patients show under the microscope Why are dsDNA antibodies most specific for SLE What does antibodies to ds-DNA typically produce on FANA testing What other assays can be used to detect antibodies to ds-DNA Why is EIA most widely used technique What is the second major antibody found in lupus patients What is histone What do histones do What can be detected in almost all patients with drug induced lupus What supports the diagnosis of drug disruptions. It forms complexes of an intermediate size that become deposited in the glomerular basement membrane of the kidney nephron which activates complement cascade and causes kidney damage. Symptoms usually disappear once the drug is discontinued Anticonvulsants and oral contraceptives Screening test for antinuclear antibodies (ANA) It detects a wide range of antibodies and is positive in about 95% of patients with SLE. Many of the antibodies are associated with other autoimmune diseases 2% of healthy individuals and up to 75% of older individuals 5% 1:80 dilution or 1:160 if the patient is over 65 Either a homogeneous pattern representing fluorescence of the entire nucleus or staining of the periphery of the nucleus occurs. They are mainly seen in patients with lupus and levels correlate with disease activity Peripheral or a homogeneous staining pattern Immunodiffusiom, RIA, EIA Because its considered more sensitive antihistone antibody A nucleoprotein that is a major constituent of chromatin They wrap the DNA like a spool of thread antihistone antibody Presence of antihistone antibody alone or combined 3 Immuno PPT Flashcards Unit 3 induced lupus Where else is antihistone antibodies found What does high levels of antihistone antibodies tend to be associated with How are antihistone antibodies typically detected What is it when antibodies stimulated by DNA complexed to histone known as How did anti-SM antibody get its name Why is anti-Sm antibody specific for SLE What kind of pattern does FANA testing show under a microscope What is used in simple slide agglutination test for SLE What also belongs to the family of extractable nuclear antigens Another method that ANAs can be detected is by What does Immunodiffusion method typically used for What does ouchterlony double diffusion detect and what does a positive reaction indicate EIA is also used to detect What are the benefits of EIA testing How does immunoblotting techniques separate out antigens What is used to visualize individual bands during immunoblotting techniques What are Antiphospholipid antibodies What does Antiphospholipid antibodies affect with antibody to ss-DNA Inrheumatoid arthritis and primary biliary cirrhosis The more active and severe forms of SLE by immunofluorescent assays, immunoblotting, EIA Deoxyribonucleoprotein Antibody to a preparation of extractable nuclear antigen was first described in a patient named smith Because its not found in other autoimmune diseases A coarsely speckled pattern of nuclear fluorescence Latex particles coated with DNP SS-A/Ro and SS-B/LA antigens Immunodiffusion To determine the immunologic specificity of a positive FANA test Detects antibody to several of the small nuclear ribonucleoproteins or extractable nuclear antigens (ENA), and is indicated by immunoprecipitation lines of serological identity Anti-ds-DNA, antihistone antibodies, anti-SS-A, and anti-SS-B Testing is quantitative, is less subjective and lends itself well to automation By means of polyacrylamide gel electrophoresis followed by blotting to a nitrocellulose sheet, and incubation with dilutions of patient serum, r Radiolabeled or enzyme antibody conjugates A heterogeneous group of antibodies that bind to phospholipid alone or are complexed with protein Affects every organ in the body, but they are especially associated with deep-vein and arterial thrombosis and with morbidity in pregnancy How was the lupus anticoagulant, Because it produced prolonged activated partial which was one of the several types of thromboplastin time (aPTT) and prothrombin time antiphospholipid antibodies, named? (PT) 4 Immuno PPT Flashcards Unit 3 What disease does the lupus anticoagulant can cause false positive results on. What risks do patients with lupus anticoagulant antibody have Another example of a systemic autoimmune disorder is What is the population that rheumatoid arthritis affects What ages does rheumatoid arthritis occur How can rheumatoid arthritis be characterized What is the progression of rheumatoid arthritis What is the strongest association of RA with certain MHC class II genes? What are the key symptoms of Rheumatoid Arthritis? What are the clinical signs of rheumatoid arthritis? About 20% of patients have nodules over the bones. Where can nodules also be found? What are the other systemic symptoms of RA? What are the symptons of Felty’s Syndrome? What are the proinflammatory cytokines found in synovial fluid? How much percent of patients with RA have the rheumatoid factor antibody? Where does complement protein C1 Syphilis An increased risk of clotting and spontaneous abortion, and platelet function may be affected Rheumatoid arthritis 1% population, women are three times as likely to be affected then men Between ages 35 and 50 but can occur at any age A chronic, symmetric, and erosive arthritis of the peripheral joints that can also affect multiple organs such as the heart and the lungs, and a decline in functional ability and reduced life expectancy It varies, because there may be spontaneous remissions or an increasingly active disease in some individuals that rapidly progresses to joint deformity and disability DR4 alleles Morning stiffness around the joints lasting at least 1 hour; swelling of the soft tissue around three or more joints; swelling of the proximal interphalangeal, metacarpophalangeal, or wrist joints; symmetric arthritis; subcutaneous nodules; a positive test for rheumatoid factor; and radiographic evidence of erosions in the joints of the hands, the wrists, or both Malaise, fatigue, fever, weight loss, and transient joint pain that begins in the small joints of the hands and feet. Myocardium, pericardium, heart valves, pleura, lungs, spleen, and larynx. Anemia, formation of subcutaneous nodules, perdicarditis, lymphadenopathy, splenomegaly, interstitial lung disease, or vasculitis Chronic RA coupled with neutropenia, splenomegaly, and thrombocytopenia Interleukin-1, interleukin-6, interleukin-8, interleukin-15, interleukin-18 and tumor necrosis factor-alpha 75 percent Immune complexes 5 Immuno PPT Flashcards Unit 3 binds to that activates the classical complement cascade? What is the lead marker for detection of RA? What is classically most often tested for to aid in making the initial diagnosis? What are the two types of agglutination tests for RF? Will the negative result for agglutination test rule out the presence of RA? What other diseases can RF be found in? How much percentage of RFnegative patients are positive for anti-CCP? What are the laboratory findings for the diagnosis of RA? What are the traditional therapy for RA? What does rituximab specifically targets on B cells? In the disease Hashimoto’s thyroiditis, the follicles with the thyroid are filled with material which is called? What is thyroglobulin? How does the TRH acts on the pituitary? Genes associated with a predisposition to thyroid autoimmunity can be divided into 2 groups: What are the 2 groups? What does immune-modulating genes include? What does thyroid-specific genes include? What is another name for Anti-CCP RF antibody One is using sheep RBCs coated with IgG and the other is using latex particles coated with the same antigen. No Syphilis, SLE, chronic active hepatitis, tuberculosis, leprosy, infectious mononucleosis, malaria, and Sjorgren’s syndrome. Approximately 35-40 percent CRP and ESR are elevated, and the level of complement components is normal or increased, indication increased synthesis. Anti-inflammatory drugs such as salicylates and ibuprofen to control local swelling and pain CD 20 antigen Colloid It is the primary constituent of colloid, a large iodinated glycoprotein, which is the precursor of the thyroid hormones triiodothyronine (T3) and thyroxine (T4) Induce release of TSH Immune-modulating genes and thyroid-specific genes. HLA antigens, cytotoxic T lymphocyte associated factor-4 (CTLA-4), and protein tyrosine phosphatase22 (PTPN22) the thyroglobulin gene and the thyroid-stimulating hormone receptor (TSHR) genes Under-secreting thyroid or chronic autoimmune 6 Immuno PPT Flashcards Unit 3 Hashimoto’s thyroiditis? What does Hashimoto’s thyroiditis patients develop? What are the symptoms of hypothyroidism? What is Graves’ disease characterized by? What are the disease manifestations of Graves’ disease? What are the major antibodies found in Graves’ disease? Does a negative test result for antithyroglobulin antibody test rule out Hashimoto’s disease? What is the treatment for Hashimoto’s disease? What is the chronic autoimmune disease that occurs in genetically susceptible individuals as a result of environmental factors? How do you characterize Autoimmune diabetes mellitus? What does progressive inflammation of the islets of Langerhans leads to? What disease is an inflammatory autoimmune disorder of the central nervous system? How are multiple sclerosis characterized? What are the 2 most common tests for diagnosis of MS? What is an autoimmune disease that affects the neuromuscular junction? What are the symptoms of myasthenia gravis? thyroiditis Patients develop a combination of goiter (or enlarged thyroid), hypothyroidism, and thyroid autoantibodies. dry skin, decreased sweating, puffy face with edematous eyelids, pallor with a yellow tinge, weight gain, and dry and brittle hair. Hyperthyroidism thyrotoxicosis, with an enlarged goiter, accompanied by nervousness, insomnia, depression, weight loss, heat intolerance, sweating, rapid heartbeat, palpitations, breathlessness, fatigue, cardiac dysrhythmias, and restlessness thyroid-stimulating hormone receptor antibody (TSHRab) and antibodies to thyroid peroxidase No Thyroid hormone replacement therapy, Monitoring the TSH levels, surgery to remove part of the thyroid gland Autoimmune diabetes mellitus, of IA diabetes insufficient insulin production caused by selective destruction of the beta cells of the pancreas, located in clusters called the islets of Langerhans Fibrosis and destruction of most beta cells Multiple Sclerosis the formation of lesions called plaques in the white matter of the brain and spinal cord, resulting in the progressive destruction of the myelin sheath of axons Oligoclonal banding and the CSF IgG index Myasthenia gravis. It is characterized by weakness and fatigability of skeletal muscles Early signs are drooping of the eyelids and the inability to retract the corners of the mouth, often resulting in a snarling appearance. Other symptoms may include difficulty in speaking, chewing, and swallowing and inability to maintain support of the trunk, the neck, or the head. If respiratory muscle 7 Immuno PPT Flashcards Unit 3 What is RIA? What is Goodpasture’s syndrome? What are the symptoms of Goodpasture’s syndrome? What is Addison’s disease? What disease can Addison’s disease progress to? What is scleroderma? What is pernicious anemia? What vitamin cannot be absorbed when you have pernicious anemia? When does autoimmune hemolytic anemia occurs? What is Idiopathic Thrombocytopenic Purpura? What is purpura? What are lymphoid malignancies weakness occurs, it can be life threatening. Onset of symptoms can be acute, resembling a stroke, or they may develop slowly and worsen over time. RIA is used to detect antibody, based on assays that block the binding of receptors by anti-ACH receptor (ACHR) antibody. A radio-labeled snake venom called α-bungarotoxin is used to irreversibly bind to ACHRs. Precipitation of receptors caused by combination with antibody is then measured. characterized by the presence of autoantibody to glomerular, renal tubular, and alveolar basement membranes That can rapidly progressed to renal failure. Signs of renal involvement include gross or microscopic hematuria, proteinuria, decreased creatinine clearance, and increased BUN and creatinine levels. Pulmonary symptoms include hemorrhage, dyspnea, weakness, fatigue, and cough. When the adrenal glands do not produce sufficient steroid hormones. Characterized by a low blood glucose, low blood pressure, and hyperpigmentation in the gums and nail beds. Addisonian crisis. Also known as systemic sclerosis, a chronic systemic autoimmune disease characterized by hardening of the skin. Loss of gastric parietal cells, which are responsible for the secretion of intrinsic factor, a protein essential for subsequent absorption of vitamin B12 in the ileum Vitamin B12 When antibodies directed against the person’s own RBCs cause them to burst, leading to insufficient plasma concentration Isolated low platelet count with normal bone marrow and the absence of other causes of thrombocytopenia. It causes a characteristic purpuric rash and an increased tendency to bleed. red or purple discolorations on the skin that do not blanch on applying pressure. They are caused by bleeding underneath the skin usually secondary to vasculitis from autoimmune distruction or dietary deficiency of vitamin C (scurvy). Leukemias and lymphomas 8 Immuno PPT Flashcards Unit 3 classified as? Differentiate leukemia and lymphoma. What does plasma cell dyscrasias primarily include? What does immunoproliferative diseases commonly involve? What is the term for an excess accumulation of cells? True or false?: Malignancies are generally due to one factor in onset. List two ways in which malignancies occur What is apoptosis? Why cells of the immune system are at great risk for malignant transformation? The lymphomas are divided into what two categories? The Rappaport classification is determined solely on what? The Working Formulation Classification Scheme, which ultimately became the standard, was based on what? How did the Working Formulation Classification Scheme classify lymphomas? 1994, the International Lymphoma Study Group proposed what classification scheme? What is Revised European-American Lymphoma (REAL) Classification? How does the REAL scheme divide NHL? In leukemias, malignant cells are primarily present in the bone marrow and peripheral blood. In lymphomas, the malignant cells arise in lymphoid tissues, such as lymph nodes, tonsils, or spleen. Multiple myeloma and Waldenstrom’s macroglobulinemia Bone marrow, lymphoid organs and other nonlymphoid sites. Malignancy False: Malignancies are generally multifactorial in onset. 1. Rapid proliferation of cells Normal proliferation of cells that fail to undergo apoptosis 2. Programmed cell death 3. The features that characterize the development of malignancy are also a normal part of the immune response – an antigenic stimulus results in proliferation of lymphoid cells and a high rate of mutation during gene rearrangement and affinity maturation 4. Hodgkin’s lymphoma (HL) and nonHodgkin’s lymphoma (NHL) 5. Morphological features by light microscopy 6. Lymph node architecture and cytology of malignant cells as seen by light microscopy 7. Low-, intermediate-, and high-grade processes, based on the aggressiveness of the untreated lymphoma 8. Revised European-American Lymphoma (REAL) Classification 9. A list that set forth the diagnostic features of lymphomas that the group members considered to be widely recognized and clearly diagnosable by contemporary techniques, including immunologic, cytogenetic, and molecular techniques. 10. Into neoplasms of precursor cells and neoplasms of mature cells of B, T, or natural killer (NK) cell lineage 9 Immuno PPT Flashcards Unit 3 What classification scheme is the basis for the one adopted by the WHO? What immunoproliferative disease is a highly treatable and often curable lymphoma that occurs both in young adults and older adults? Hodgkin’s Lymphoma (HL) is characterized by the presence of what cells and where? Describe Reed-Sternberg (RS) cells True or False: Reed-Sternberg (RS) cells may be in the B-Cell Lineage True or False: Epidemiological studies suggest that HL has an infectious etiology. In order to reflect the differences in clinical presentation, morphology, phenotype, and molecular features, the REAL/WHO classification recognizes a basic distinction between what two types of HL? Patients with HL have elevated levels of what? What is the causative agent of infectious mononucleosis? What is the most sensitive method to detect presence of latent EBV infections in RS cells? NHL includes a wide range of neoplasms. What % are B-cell lymphomas in the U.S.? True or False: NHL lymphomas tend to be slowly progressive and compatible with long-term survival, while others are typically highly aggressive and rapidly fatal if not treated Which is more difficult to characterize? T-cell or B-cell lymphomas? Why are T-cell lymphomas more difficult to characterize than B-cell lymphoma? 11. REAL scheme 12. Hodgkin’s Lymphoma (HL) 13. Reed-Sternberg (RS) cells in affected lymph nodes and lymphoid organs 14. Typically large with a bilobed nucleus and 2 prominent nucleoli 15. True 16. True 17. Nodular lymphocyte predominant HL (NLPHL) and classic HL 18. Antibody to Epstein-Barr Virus (EBV) 19. EBV 20. RNA assay for EBV-encoded RNAs: EBER1 and EBER2 21. 85% of NHL cases are B-cell lymphomas 22. True 23. T-cell lymphomas 24. B-cell lymphomas can be tested for monotypic light-chain expression; whereas no easy way exists to assay the clonality in a similar way with T-cell lymphomas. Also, 10 Immuno PPT Flashcards Unit 3 True or False: Some T-cell syndromes progress stealthily form atypical but non-clonal proliferations into clonal malignancies. What are the 2 general categories of leukemia? What type of leukemia is usually slowly progressive and compatible with extended survival? What type of leukemia is generally much more rapidly progressive but has a higher response rate to therapy compared to the chronic leukemias. This leukemia is characterized by presence of very poorly differentiated precursor cells (blast cells) in the bone marrow and peripheral blood Immunologically, ALL is divided into how many types? What are the 4 types of ALL? What type of leukemia is a group of diseases almost exclusively of B-cell origin. Chronic lymphocytic leukemia (CLL), small lymphocytic lymphoma (SLL), prolymphocytic leukemia (PL), and hairy cell leukemia (HCL) are examples of what type of leukemia? The World Health Organization (WHO) considers these leukemias a single disease with different clinical presentations. This leukemia is a common hematopoietic malignancy that involves the expansion of a clone of B cells that have the appearance of small mature lymphocytes. This leukemia is a rare, slowly progressive disease characterized by infiltration of the bone marrow and some T-cell syndromes progress stealthily form atypical but non-clnoal proliferations into clonal malignancies. 25. True Acute or Chronic 26. Chronic leukemia Acute leukemia Acute lymphoblastic leukemia (ALL) 4 CALLa (CD10)-expressing immature B cell ALL, pre-B cell ALL without CALLa, T-cell ALL, and Bcell ALL. Chronic lymphocytic leukemias/lymphomas Chronic lymphocytic leukemias/lymphomas Chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL), Chronic lymphocytic leukemia (CLL) Hairy cell leukemia 11 Immuno PPT Flashcards Unit 3 spleen by leukemic cells, without involvement of lymph nodes. In Hairy cell leukemias, patients usually present with cytopenias because of ____. True or False: In Hairy cell leukemia, the blood lymphocyte count is not very high usually. Describe appearance of malignant lymphocytes in HCL Plasma cell dyscrasias include several related syndromes. What are they? Plasma cell dyscrasias are characterized by the overproduction of what? True or False: M protein is usually associated with other lymphoproliferative disorders, such as non-Hodgkin lymphoma (NHL) or primary amyloidosis. True or False: Laboratory evaluation is not important in the diagnosis and differentiation of plasma cell dyscrasias conditions. Diagnosis and monitoring of the plasma cell dyscrasias depend heavily on detecting and quantifying what protein? What disease is a malignancy of mature plasma cells that accounts for about 10 percent of all hematologic cancers? Which is the most serious and most common of the plasma cell dyscrasias? Patients progress from the asymptomatic ___ to ___ to the symptomatic disease of multiple myeloma. Patients with multiple myeloma typically have excess plasma cells in Bone marrow infiltration True Round with a “bland” cytological appearance. They often have irregular, “hairy” cytoplasmic projections from their cytoplasmic surfaces. multiple myeloma, Waldenström’s macroglobulinemia, and the premalignant conditions monoclonal gammopathy of undetermined significance (MGUS) and smoldering multiple myeloma (SMM) A single immunoglobulin component called a myeloma protein (M protein), or paraprotein, by a clone of plasma cells. False. It is rarely associated with these. False M protein Multiple myeloma Multiple myeloma monoclonal gammopathy of undetermined significance (MGUS); smoldering multiple myeloma (SMM). bone marrow; bone lesions 12 Immuno PPT Flashcards Unit 3 ____ a monoclonal immunoglobulin component in the plasma and/or urine, and lytic _____. True or False: In multiple myeloma plasma cells infiltrating the bone marrow may be morphologically normal or may show atypical or bizarre cytological features. In multiple myeloma, the immunoglobulin produced by the malignant clone can be of any type. Which is the most common? In multiple myeloma, the immunoglobulin produced by the malignant clone can be of any type. After IgG, which 2 are the most common? Why are an excess of free light chains produced in multiple myeloma? In what percent of cases do myeloma cells exclusively produce light chains? Free light chains are rapidly excreted in ___. What are free immunoglobulin light chains (κ or λ) excreted in the urine? True or False: In multiple myeloma, very rarely, two or more distinct M proteins are produced, or a clinically typical myeloma may produce no secretory product In multiple myeloma, compare the level of normal immunoglobulin to the amount of M protein present in the serum The clinical manifestations of multiple myeloma are primarily ___, ___ and ___. What percent of patients with multiple myeloma develop light- True IgG (50%) IgA and IgM (light chains only) Very often the production of heavy and light chains by the malignant plasma cells are not well synchronized 10% Urine Bence Jones protein True The level of normal immunoglobulin is often decreased in proportion to the amount of M protein present in the serum Hematologic, skeletal, and immunologic. 15% 13 Immuno PPT Flashcards Unit 3 chain deposition disease or amyloidosis What two related disorders have free light chains or fragments of immunoglobulin deposited in the tissues? How do amyloid fibers stained with the dye Congo red appear when viewed under a polarizing microscope? Deposits of light chains in multiple myeloma can be identified in what specimens? With what techniques? Criteria for the diagnosis of multiple myeloma include? M proteins can be detected in serum or urine by what 2 methods? An important feature supporting the diagnosis of multiple myeloma is the presence of this protein in urine Free light chains can be detected in serum or urine by what 2 methods? What disease is a malignant proliferation of IgM-producing lymphocytes and corresponds to lymphoplasmacytoid lymphoma as defined by the WHO? Describe the malignant cells of Waldenström’s macroglobulinemia The clinical signs and symptoms of Waldenström’s macroglobulinemia are? The following symptoms are indicative of what immunoproliferative disease? Weakness, fatigue, anemia, bleeding, and hyperviscosity How common are lytic bone lesions, hypercalcemia, and renal tubular abnormalities in Waldenström’s macroglobulinemia? light-chain deposition disease and amyloidosis Apple-green birefringence Tissue sections; immunofluorescence or immunohistochemical staining with specific antibodies. plasma cells constituting greater than 10 percent of bone marrow cells or a plasmacytoma (a solid tumor mass of plasma cells), plus either serum M protein greater than 3g/dL, urinary M protein, or osteolytic bone lesions. electrophoresis and immunofixation Bence Jones protein electrophoresis and immunofixation Waldenström’s macroglobulinemia Malignant cells are more immature than plasma cells and have a microscopic appearance somewhere between that of small lymphocytes and plasma cells. Infiltration of the malignant cells into bone marrow, the spleen, and lymph nodes with the overproduction of monoclonal IgM Waldenström’s macroglobulinemia They are rare 14 Immuno PPT Flashcards Unit 3 All individuals with Waldenström’s macroglobulinemia have elevated serum monoclonal protein that migrates in the ___ region. True or False: In WM, the concentration of the monoclonal IgM varies widely, and it is not possible to define a concentration that differentiates this disease from other B-cell lymphoproliferative disorders In 10–20 percent of WM patients, the IgM paraproteins behave as ___. Cryoglobulins precipitate at what temperature? What type of proteins can occlude small vessels in the extremities in cold weather in WM? In WM, some IgM paraproteins have specificity for i or I antigens and will agglutinate red blood cells in the cold; they are referred to as ____. Approximately 20 percent of patients with Waldenström’s macroglobulinemia will present with what symptom? The laboratory is involved in how many major ways in evaluating lymphoproliferative disorders? The lab assesses the immunophenotype of hematopoetic cells in the bone marrow or lymphoid tissues using what technique? True or False? One of the major roles of the lab is to evaluate the amount and characteristics of immunoglobulins. An assessment of of genetic and chromosomal abnormalities in hematopoietic malignancies is not assessed by the laboratory. In the diagnosis and classification of leukemias and lymphomas, flow cytometry is used to analyze cell surface marker ___ antigen expression What lab technique is ideal for fluids Gamma True Cryoglobulins Cold temperatures; Cryoglobulins cold agglutinins peripheral neuropathy 3 Flow cytometry True False CD (cluster of differentiation) Flow cytometry 15 Immuno PPT Flashcards Unit 3 in which cells are naturally suspended, but it is also useful in lymphoid tissues, from which singlecell suspensions can be easily made What lab technique can simultaneously analyze, even in small samples, multiple-cell properties, including size, granularity, and surface and intracellular antigen. What is monoclonal gammopathy? The evaluation of a patient for the possibility of a monoclonal gammopathy requires both qualitative and quantitative analysis of what? The initial tests used to screen for the presence of a monoclonal gammopathy are? True or False? Quantitative measurement of serum or urine immunoglobulins is used in the diagnosis of some lymphoproliferative disorders What is the name of the technique in which serum proteins are separated on the basis of their size and electrical charge Additional evaluation of serum immunoglobulin is performed if the SPE shows a ___ component; if there is a significant quantitative abnormality of serum immunoglobulins, or if the clnical picture strongly suggests a plasma cell ____. Myeloma in which only light chains are produced may not be detected using what technique and why? After SPE, what 2 techniques that may be used in the next step in evaluating a monoclonal gammopathy? Compare immunoelectrophoresis Flow cytometry In a malignant disorder, the clonal proliferation of transformed plasma cells leads to overproduction of a single immunoglobulin Immunoglobulins serum immunoglobulin levels and serum protein electrophoresis True Serum protein electrophoresis (SPE) Monoclonal; dyscrasia Serum protein electrophoresis (SPE), because the light chains are rapidly cleared in the urine. immunoelectrophoresis (IEP) or immunofixation electrophoresis (IFE). IFE is much faster than IEP, has much greater 16 Immuno PPT Flashcards Unit 3 (IEP) and immunofixation electrophoresis (IFE) in terms of accuracy and sensitivity. On immunofixation, areas of diffuse staining indicate______, while monoclonal bands produce narrow, intensely stained bands The majority of B-cell lymphomas and some T-cell lymphomas are characterized by specific chromosome _____. Specific chromosome translocations are of particular value in diagnosis of disease such as many B-cell and Tcell lymphomas. These can usually be detected using: List two common secondary chromosome events (secondary to specific chromosome translocations) that are rarely specific to particular type of lymphoma but provide valuable prognostic information Traditional cytogenetic evaluation has been expanded by a technique known as? True or False: Lymphoid malignancies can also be evaluated by molecular genetic techniques. What methods are usually geared toward finding clonal rearrangements of the immunoglobulin gene in B-cell malignancies or of the T-cell receptor gene in T-cell malignancies. What type of rearrangements are too subtle to be detected by conventional cytogenetics and must use FISH or molecular genetic techniques? What technique allows the efficient measurement of expression for almost every gene in the human genome in a single overnight hybridization experiment. What genomic-scale approach has begun to reveal novel molecularbased subclasses of many malignancies, including lymphoma sensitivity, and is the most accurate assay for typing paraproteins. polyclonal immunoglobulins Translocations Cytogenic techniques Aneuploidy (abnormal number of chromosomes) and deletion of specific chromosome regions fluorescence in situ hybridization (FISH) True fluorescence in situ hybridization (FISH) and molecular genetic techniques. Clonal rearrangements of the immunoglobulin gene in B-cell malignancies or of the T-cell receptor gene in T-cell malignancies. complementary DNA (cDNA) microarray technology complementary DNA (cDNA) microarray technology 17 Immuno PPT Flashcards Unit 3 and leukemia? What organ system is a diverse and complicated network of many biochemical and cellular components? Primary immunodeficiency syndromes are rare, with the exception of ___ deficiency. True or False: a defect in one arm of the immune system may affect other aspects of immune function as well The components of the humoral and cell-mediated portions of the immune system interact extensively through many ___. A deficiency of one component of the system is often accompanied by _____of other component, including allergic or autoimmune manifestations Over how many different congenital forms of immunodeficiency have been reported, including defects in lymphoid cells, phagocytic cells, and complement proteins? True or False: The clinical symptoms associated with immune deficiencies range from very mild or subclinical to severe recurrent infections or failure to thrive. In general, defects in humoral immunity result in pyogenic bacterial infections, particularly where? Defects in T-cell-mediated immunity result in recurrent infections with what type of intracellular pathogens? What system is part of the innate, antigen-nonspecific immune response and includes neutrophils and mononuclear phagocytic cells. What system is activated to produce biologically active molecules that enhance inflammation and promote lysis of cells and microorganisms. What are the mechanisms of the agammaglobulinemias? Immune system IgA True Regulatory and effector loops hyperactivity 120 True upper and lower respiratory tract. viruses, fungi, and intracellular bacteria The phagocytic system The complement system Genetic defects in B-cell maturation or mutations leading to defective interactions between B and T 18 Immuno PPT Flashcards Unit 3 In evaluating immunoglobulin deficiency states, it is important to remember this varies with age When does IgM reach normal adult levels? When does IgG reach normal adult levels? True or False: In some normal children, IgA levels do not reach normal adult values until adolescence. All infants experience low levels of immunoglobulins at approximately ____ of age, but in some cases, the low levels persist for a longer time. Transient hypogammaglobulinemia of infancy (THI) may result due to what? What is the mechanism of transient hypogammaglobulinemia? In THI, what type of immunity is normal? In THI, what Ig is the most affected, dropping at least 2 SDs below the age-adjusted mean? THI patients have normal numbers of circulating CD19 positive B-cells unlike what agammaglobulinemia? First described in 1952, this agammaglobulinemia is X chromosome–linked, and so affects males almost exclusively. Patients with X-linked agammaglobulinemia lack what type of circulating cell? Patients with X-linked agammaglobulinemia lack immunoglobulins of what class? Patients with Bruton’s agammaglobulinemia have no plasma cells in their lymphoid tissues, but do have this type of cell in their bone marrow? What type of lymphocytes are found in normal numbers and function in cells. blood levels of immunoglobulins 1st year of age 5-6 years of age True. 5-6 months Low levels of immunoglobulins past 5-6 months of age Unknown Cell-mediated immunity IgG Bruton’s agammaglobulinemia Bruton’s agammaglobulinemia Mature CD19 positive B-cell All classes pre-B cells T cells 19 Immuno PPT Flashcards Unit 3 Patients with Bruton’s agammaglobulinemia? What type of recurring infections do these patients develop beginning in infancy, as maternal antibody is cleared. What results from arrested differentiation at the pre-B cell stage, leading to a complete absence of B cells and plasma cells. What is the underlying genetic mechanism in X-linked hypogammaglobulinemia? What enzyme is the apparent cause of failure of Vh gene rearrangement? Agammaglobulinemia can be differentiated from transient hypogammaglobulinemia of infancy by the absence of what? Are most patients with IgA deficiency symptomatic or asymptomatic? Those patients with symptoms usually have infections of the respiratory and gastrointestinal tract and an increased tendency to what types of autoimmune diseases? What other disorders are more common among these patients. Although the genetic defect has not been established, it is hypothesized that the IgA deficiency is caused by what? What group of disorders is common variable immunodeficiency (CVI)? This disorder is considered a lowincidence disorder; although it still remains the most common primary immune deficiency with a severe clinical syndrome. How is the CVI disorder acquired? Is it seen more in men or women? What is CVI characterized by? What can it lead to? recurrent bacterial infections X-linked hypogammaglobulinemia It is a deficiency of an enzyme called the Bruton tyrosine kinase (Btk) in B-cell progenitor cells. Lack of the Btk enzyme CD19 positive B cells in the peripheral blood, by the abnormal histology of lymphoid tissues, and by its persistence beyond 2 years of age. asymptomatic Systemic lupus erythematosus, rheumatoid arthritis, celiac disease, and thyroiditis. Allergic disorders and malignancy Impaired differentiation of lymphocytes to become IgA-producing plasma cells. It falls under the heterogeneous group of disorders. The common variable immunodeficiency syndrome. Congenital or acquired, familial or sporadic. It occurs with equal frequency in men and women. Hypogammaglobulinemia Recurrent bacterial infections, particularly sinusitis and pneumonia. 20 Immuno PPT Flashcards Unit 3 What percentage of CVI patients develop herpes zoster (shingles)? What immunoglobulin is usually deficient? What type of reoccurring infections are typically seen when diagnosing patients that demonstrate a low serum IgG level? In contrast to X-linked agammaglobulinemia, most patients with CVI have normal numbers what type of cell? How many subclasses of IgG are in humans? Out of the IgG, what percentage of the IgG1 is normally present? Out of the IgG, what percentage of the IgG2 is normally present? Out of the IgG, what percentage of the IgG3 is normally present? Out of the IgG, what percentage of the IgG4 is normally present? In patients with recurrent infections, what other testing should be performed if the total IgG levels are normal but the clinical picture suggests immunoglobulin deficiency. If the total IgG level was normal could there still be a deficiency in one of the subclasses? Increased bacterial infections may result from what? Defects in cell-mediated immunity can result from abnormalities in what stages? What types of defects can result in severe combined immunodeficiency (SCID)? Besides primary defects in cellmediated immunity what other effects can happen? In general, defects in cellular immunity are more difficult to manage than what other defects? Patients with severe defects in cellmediated immunity may develop 20 percent, which is a much higher incidence than in immunologically normal young adults. Both IgA and IgG, but selective IgG deficiency may occur. They tend to have recurrent bacterial infections. Mature B cells Four About 70 percent About 20 percent About 6 percent About 4 percent levels of the different subclasses should be measured. Yes, a deficiency of a single IgG subclass may not result in a total IgG level below the normal range. IgG subclass deficiencies. Many different stages of T-Cell development Molecular defects Can also have secondary effects on humoral immunity. Defects in humoral immunity They can develop graft-versus-host (GvH) disease. 21 Immuno PPT Flashcards Unit 3 what disease? This happens when the donor lymphocytes are allowed to survive, proliferate, and attack the recipient’s tissue as foreign. When can GvH disease occur? GvH disease also occurs in patients who have received this type of transplant. This anomaly affects thymic development. All organs derived from these structures can be affected. DiGeorge anomaly associated abnormalities include what? • The severity and extent of the developmental defect can be quite variable in this disease. The immunodeficiency associated DiGeorge anomaly is a quantitative defect in what type of cells? Insufficient types of these are made, but those that are present are functionally normal. One immunodeficiency state for which a specific enzymatic basis has been defined is what? The condition presents in what age group and has recurrent or chronic pulmonary infections, oral or cutaneous candidiasis, diarrhea, skin infections, urinary tract infections, and failure to thrive. An enzyme involved in the metabolism of purines is what affects this deficiency. What causes the number of T cells to progressively decrease because of the accumulation of this toxic purine metabolite? This can be caused by a defect that affects development of both types of lymphocytes or a defective interaction between the two limbs of the immune system. A severe defect in the T-cell system. GvH disease can occur in any individual with a severe defect in cell-mediated immunity (e.g., in bone marrow transplant recipients) and can be fatal. A bone marrow transplant. DiGeorge anomaly is a developmental abnormality of the third and fourth pharyngeal pouches that affects thymic development. Embryonic structures Mental retardation, absence of ossification of the hyoid bone, cardiac anomalies, abnormal facial development, and thymic hypoplasia. DiGeorge anomaly Thymocytes Mature T cells Purine nucleoside phosphorylase (PNP) deficiency, a rare autosomal recessive trait. The condition presents in infancy PNP- Purine nucleoside phosphorylase Deoxyguanosine triphosphate Defects in both humoral (B cell) and cell-mediated (T cell) immunity 22 Immuno PPT Flashcards Unit 3 a) What are the combined deficiencies are referred to? b) The most serious of the congenital immune deficiencies is this? c) SCID is actually a group of related diseases that all affect what? d) What is the most common form of the SCID disease? e) The abnormal gene involves codes for a protein chain called the common gamma chain, which is common to these Il receptors. f) What chromosome is the gene that is referred to as the IL2RG gene located? g) Normal signaling cannot occur in cells with defective receptors, thus halting what? h) This gene is required for processing an interleukin binding signal from the cell membrane to the nucleus. i) Depending on the presence of any additional defect in the JAK3 gene, may result is these phenotypes? j) In such cases, no antibody production or lymphocyte proliferative response follows this. k) Caused of SCID can also be identified as what type of defects? l) Patients with this immune deficiency generally present early in infancy with infection by nearly any type of organism, including oral candidal infections, pneumonia, and diarrhea. m) This is a rare is a rare X-linked recessive syndrome. n) It is defined by the triad of what? o) WAS is usually lethal in childhood because of? p) Abnormalities exist in both the cellular and humoral arms of the immune system, related to a general defect in what? q) This manifests as a severe deficiency of the naturally occurring antibodies to what antigens? using a shorthand of T+-B+-NK+-, with the superscript +- denoting whether each cell type is deficient. Severe combined immunodeficiency (SCID). T- and B-cell function but with differing causes X-linked SCID Interleukins 2, 4, 7, 9, 15, and 21. X chromosome natural maturation The JAK3 gene Either a T-B+NK+ or a T-B+NK- phenotype An antigen or mitogen challenge. Other molecular defects SCID Severe combined immunodeficiency Wiskott-Aldrich syndrome (WAS) Immunodeficiency, eczema, and thrombocytopenia. Infection, hemorrhage, or malignancy. Antigen processing Blood group antigens (isohemagglutinins). 23 Immuno PPT Flashcards Unit 3 r) In addition, these patients have persistently increased levels of what? s) What is the primary molecular defect in the syndrome? t) Abnormalities cause defective in what? u) It also affects its signal transduction in what? v) The laboratory features of WAS include what? w) This is a rare autosomal recessive syndrome characterized by cerebellar ataxia and telangiectasias, especially on the earlobes and conjunctiva. x) Blood vessels in the sclera of the eyes may be dilated, and there may also be this characteristic rash on part of the face. y) What disease do 95 percent of patients’ exhibit increased levels of serum alphafetoprotein? z) Abnormal genes produce a combined defect in this type of immunity. aa) Antibody response to antigens, especially to this, is blunted. bb) What levels immunoglobulin’s are often low or absent, although the pattern can be quite variable? cc) In addition, the number of circulating what type of cells is often decreased. dd) This is a group of disorders inherited as either an X-linked or autosomal recessive gene that affects neutrophil microbicidal function. ee) This disease accounts for 70 percent of the cases, and it tends to be more severe. ff) Symptoms of CGD include recurrent what? Serum alpha-fetoprotein. It appears to be an abnormality of the integral membrane protein CD43, which is involved in the regulation of protein glycosylation. Actin polymerization Lymphocytes and platelets A decrease in platelet number and size, prolonged bleeding time, and bone marrow changes with a normal or somewhat increased number of megakaryocytes Ataxia-telangiectasia (AT) Reddish butterfly area on the face and ears. WAS or Ataxia-telangiectasia (AT) Check book Both humoral and cellular immunity polysaccharides IgG2, IgA, and IgE T cells Chronic granulomatous disease (CGD) X-linked disease Suppurative infections, pneumonia, osteomyelitis, draining adenopathy, liver abscesses, dermatitis, and hypergammaglobulinemia. The neutrophil abnormalities gg) CGD is the most common and best characterized of this type of abnormalities? hh) There are three different autosomal Nicotinamide adenine dinucleotide phosphate recessive genes involved, and all of these (NADPH) oxidase. 24 Immuno PPT Flashcards Unit 3 affect subunits of what? ii) What normally leads to the production of reactive oxygen molecules, such as hydrogen peroxide (H2O2), by NADPH oxidase on the plasma membrane? jj) These granules fuse with, and release their contents into, the forming phagosome, as organisms are phagocytized. kk) What is used by the granule enzyme myeloperoxidase to generate the potent microbicidal agent hypochlorous acid. ll) The process of generating partially reduced forms of oxygen by stimulated neutrophils was first detected as what? mm) This response was originally termed the neutrophil “respiratory burst”; a more correct term is called? • In CGD, neutrophils are unable to do what? nn) • CGD was historically diagnosed by measuring the ability of a patient’s neutrophils to reduce what dye? 1. • More recently, this assay has become available. 1. 1. In this assay, what are neutrophils labeled with? • DHR will do what when it is reduced. 2. 1. The neutrophils are then activated using this, which is mitogenic for neutrophils. 2. The resultant oxidative burst will reduce the DHR, resulting in what? • Neutrophils from CGD patients will be unable to undergo this reaction and will show less fluorescence than normal neutrophils. 3. 1. This deficiency leads to an inability to generate enough NADPH to supply reducing Normally, neutrophil stimulation Neutrophil granules Hydrogen peroxide An increase in oxygen consumption. “oxidative burst.” undergo the oxidative burst The dye nitro-blue tetrazolium (NBT) a flow cytometric assay dihydrorhodamine (DHR) fluoresce Phorbol myristate acetate (PMA) Fluorescence that may be quantified by flow cytometry. oxidative burst Neutrophil glucose-6-phosphate dehydrogenase deficiency. 25 Immuno PPT Flashcards Unit 3 • • • • • equivalents to the NADPH oxidase system. 2. This deficiency leads to a defect in hydrogen peroxide production and a clinical picture similar to that of what other disease? Even if this is normal, neutrophils cannot perform their functions properly if they fail to leave the vasculature and migrate to a site of incipient infection. 3. These play important roles in microbicidal activity. 1. What causes a protein deficiency in a component of adhesion receptors on neutrophils, monocytes, and T cells? What proteins does LAD affect in neutrophils, monocytes, and T cells? • How are the leukocytes affected with LAD? What is the clinical manifestation with LAD? • How can a CD18 defect be diagnosed? • What can lead to deficiencies in each of the major complement components and lead to various clinical sequelae? Deficiencies in early complement components (C1q, C4 and C2) are associated with what type of syndrome? Which is the most common complement component deficiency? What differentiates C3 deficiency from other lupus-like clinical presentation? What infection is associated with deficiencies in the later components of complement (C5-C9)? Measurement of the levels of are used to screen for defects in antibody production. What is easily performed by the transfusion service? An overall assessment of the antibody- • • • • • • • CGD (Chronic granulomatous disease) microbicidal activity Adhesion receptors on leukocytes and their counterreceptors on endothelial cells and extracellular matrix LAD: Leukocyte adhesion deficiency Neutrophils: CD18 Monocytes: CD11b or CD11c T cells: CD11a Abnormal adhesion, motility, aggregation, chemotaxis, and endocytosis Delayed wound healing, chronic skin infections, intestinal and respiratory tract infections, and periodontitis By detecting a decreased amount of CD11/18 antigen with flow cytometry. LAD: Leukocyte adhesion deficiency Lupus-like syndrome A deficiency in C2 And increased likeliness of recurrent encapsulated organism infection. Neisseria meningitidis Serum IgG, IgM, IgA, and levels of the subclasses of IgG Assay for isohemagglutinins Antibody response to antigens that the population is 26 Immuno PPT Flashcards Unit 3 • • mediated immunity can be made by measuring: Delayed-hypersensitivity- type skin reactions can be used to screen for defects in: True or False: Immunodeficiency Disease test are generally performed by laboratory personnel. Screening for complement deficiencies begins with? CH50 assay can determine? A flow cytometric assay can detect what defect in neutrophil activity? When is more specialized testing probably be necessary to precisely identify an immune abnormality? Flow cytometry can also enumerate in the peripheral blood, bone marrow, and lymph nodes. An absence or profound decrease in the number of CD3 positive cell is consistent with: When CD19 positive B cells are absent it suggest? True or False: Genetic testing is available for many immunodeficiency conditions. By assessing the ability of isolated T cells to proliferate in response to an antigenic stimulus or to nonspecific mitogens in culture, what can be measured? An increase in uptake suggest cell division and activation. What can be measured without the use of radioactive materials? As of August 2008, three assays to measure antigen- or mitogen-stimulated T-cell activation for diagnostic use was cleared by which federal entity? What is the measured in a workup of both immunodeficiency states and some lymphoproliferative disorders? What is used to make the quantitative measurements of serum and urine exposed normally or following vaccination. Cell-mediated immunity False: The screenings are done by the clinician. CH50 assay The level of functional complement in an individual. Defect in neutrophil oxidative burst activity 1. The screening tests detect an abnormality. 2. The clinical suspicion is high. Classes of lymphocytes DiGeorge Syndrome Bruton’s agammaglobulinemia True T-cell function. Thymidine Antigen- or mitogen-stimulated T-cell activation FDA Quantitative measurements of serum and urine immunoglobulins. Protein electrophoresis 27 Immuno PPT Flashcards Unit 3 immuoglobulins? What method allows for reproducible separation of the major plasma proteins> What determines if additional evaluation of the serum is necessary? Immunofixation electrophoresis (IFE) is another method to characterize: When does immunofixation electrophoresis result in areas of diffuse staining? What produces narrow, intensely stained bands in IFE? What does IFE with a lack of bands indicate in immunodeficiencies? How can specific immunoglobulin isotype levels be determined? How are monoclonal gammopathies or immunodeficiencies evaluated? What is the transfer of tissue from one area of the body to another of the same individual the graft is called? What is the graft called when there is transfer of cells or tissues between identical twins? Where is an allograft tissue/cell transferred? Where is a xenograft tissue/cell transferred? Why is transplantation utilized? In 2006, how many solid organ transplants performed in the United States? How many stem cell transplants were performed world wide in 2006? What is the testament to the numerous developments over the past few decades in patient management before and after transplant? What else does the number of transplant performed illustrate in advancements? What critically important immunologic mechanisms require continued clarification? Protein electrophoresis. 1. SPE shows monoclonal component -OR2. A significant quantitative abnormality of serum immunoglobulins. Immune deficiencies. Polyclonal immunoglobulins. Monoclonal immunoglobulins One or more immunoglobulin classes. Nephelometry A bone aspirate and biopsy. An autograft Syngeneic graft To another individual of the same species. To another individual of a different species. It can potentially be a life saving treatment for end stage organ failure, cancers, autoimmune diseases, immune deficiencies, and a variety of other diseases. Over $28,000 $50,000 The number of transplants performed The technologies for organ and stem cells acquisition and sharing. Mechanisms of graft rejection and graft-versusdisease. 28 Immuno PPT Flashcards Unit 3 Specifically, what two components of the immune system that promote sustained graft survival are being researched? Transplantation immunology is the largest immunologic barrier to successful: When does cell surface proteins play a central role in immune recognition and initiation of immune responses? Why do allergenic responses result in graft rejection in solid-organ and stem cell transplantation or graft-versus-host disease in stem cell transplantation? When would an allogeneic response within the recipient occur? Classical (transplant) HLA antigens are also know as: What are the Class I HLA antigens? What are the Class II HLA antigens? Where is the encoding for HLA proteins located? HLA genes are inherited as from parental chromosomes. Offspring receive HLA haplotype from each parent. According to Mendelian inhertance, there is a chance of two siblings inheriting the same two haplotypes, 50% chance of being HLA , and a chance of not sharing neither HLA haplotype. What does it meant to be: 1. HLA identical 2. HLA haploidentical 3. HLA non-identical HLA proteins are molecules. Where are class I proteins expressed? What is the product of the HLA-A,B, and C genes? What are co-dominantly expressed on virtually all nucleated cells? What is the products of the HLA-DRB1 1. The role of human leukocyte antigens (HLA) 2. The development of pharmacological agents that interfere with various components of the immune system Allogeneic organ transplantation Transplantation Immunology The ubiquitous presence of cell surface proteins on the surface of nucleated cells and their extensive degree of polymorphism. When there is a graft rejection in solid-organ and stem cell transplantation or graft-versus-host disease in stem cell transplantation. Major histocompatibility antigens. HLA-A, B, and C HLA-DR, DQ, and DP On the short arm of chromosome 6 in a set of closely linked genes of the major histocompatibility complex (MHC). Haplotypes One 1. 25% 2. haploidentical 3. 25% 1. Siblings share the same two haplotypes. 2. Siblings share one of two HLA haplotypes. 3. Siblings do not share HLA haplotypes. Heterodimeric On the cell surface covalently bound to beta-2microglobulin. Class I Proteins Class I heterodimers Class II heterodimers. 29 Immuno PPT Flashcards Unit 3 + DRA1, HLA-DQB1 + DQA1, and DPB1 + DPA1 genes? Where are Class II heterodimers codominantly expressed? Where do HLA proteins play a critical role for the development and function of the system? How do HLA initiate adaptive immune responses? What serves as ligands for regulatory receptors on natural killer cells in the innate immune response? The genes encoding the HLA proteins is an extensive degree of: What system is the most polymorphic genetic system in humans? Why polymorphism both considered an advantage and disadvantage? How were the second set of transplantation antigens identified? What disease was developed in the studies that identified the second set of transplantation antigens? What results in a “slower” rejection pace? What is the name of second set of transplantation antigens? What are mHAs? Where has encoding for mHAs been identified? How can you induce a recipient immune response to the donor variant? Primarily on antigen-presenting cells (example: dendritic cells, monocytes, macrophages, B lymphocytes.) The innate and adaptive immune system. They serve as recognition elements for antigen receptors on T lymphocytes. HLA proteins Allelic polymorphism HLA system Enables populations to survive infectious challenges, but severely restricts the ability to transplant foreign tissue or cells between any two individuals. Studies demonstrated tissue rejection in MHCidentical transplants and human stem cell transplants between HLA-identical siblings. Graft-versus-host disease Minor Histocompatibility antigens (mHAs) Minor Histocompatibility antigens (mHAs) Non-HLA proteins that demonstrate polymorphism in amino acid sequence within a species. Both X-linked and autosomally. By introducing a polymorphic variant of one of these proteins from one individual into another individual who possesses a different polymorphic variant. Why does the recipient immune response CD4 and/or CD8 T cells recognize a variant protein occur? in the context of the recipient MHC molecule. What is the recipient immune response Foreign microbial antigen reaction to the mHAs analogous to? What mHAs have been identified? 1. Proteins encoded by the male Y chromosome 2. Proteins for which the recipient has homozygous gene deletion. 3.Proteins that are autosomally encoded. 4. Proteins that are mitochondrial DNA encoded. 30 Immuno PPT Flashcards Unit 3 Where are surface proteins that are involved in gamma/delta T-cells responses encoded? Where can MIC proteins be expressed? Where can’t MIC proteins be expressed? When can MICA proteins serve as targets? Antibodies to MICA antigens have been detected in as many as % of kidney transplant patients. What are MICA antibodies associated with? What is the only blood group system that impacts clinical transplantation? Anti-A or anti- B antibodies develop in individuals lacking: Why is ABO blood group incompatibility a barrier to solid-organ transplantation? What can lead to hyperacute rejection of the transplanted organ? Why must recipient-donor pairs be ABO identical or compatible? An individual of blood group A will posses anti-B antibodies, and can only receive organ from an donor. A B-expressing individual has anti-A antibodies and can only receive an orgam from an donor. What has allowed the successful transplantation of kidneys from ABOincompatible donors? How is successful transplantation of kidneys from ABO-incompatible donors possible? What other polymorphic genetic system impacts allogeneic transplantation? Who do the KIRs regulate? How do KIRs regulate NK lymphocytes? What governs the activity of the NK cell? What do NK cells do? What class of MHC molecules are ligans MHC class I-related chain A (MICA) Endothelial cells, keratinocytes, fibroblasts, epithelial cells, dendritic cells, and monocytes. T or B lymphocytes Allograft immune responses. 11% Rejection episodes and decreased graft survival. The ABO system. The corresponding blood group antigens. The antibodies can bind corresponding antigens expressed on the vascular endothelium. The complement cascade activated by ABO blood group antibodies. The antibodies can bind corresponding antigens expressed on the vascular endothelium. ABO-A or O ABO-B or O Plasma exchange and intravenous immunoglobulin administration. By lowering ABO antibody to levels that allow transplantation to proceed without risk of hyperacute rejection. The killer Immunoglobulin-like receptor (KIR) system. Natural killer (NK) lymphocytes. With the activating and inhibitory receptors that vary in number and type on the any individual NK cell. The balance of signals received by the activating and inhibitory receptors. NK cells secrete cytokines and non-MHC restricted cytotoxicity. MHC class I 31 Immuno PPT Flashcards Unit 3 for the inhibitory KIRs? As the NK cells encounter self class I MHC proteins as it circulates the body, what interaction allows for the NK cells to maintain a quiet state? How is the NK signal activated? Where is the regulatory role of KIRs being exploited? How is the regulatory role of KIRs helping in stem cell transplantation? What is the result of receiving donor inhibitory KIR? What has shown to mediate a graftversus-leukemia reaction and prevent relapse after transplantation? Transplantation of cells or tissues between two individuals is classified by: Most transplantation falls into the category of: What will result in a vigorous immune response to foreign MHC antigens and is the primary stimulus to graft rejection? How is the response to foreign MHC antigens characterized? What two distinct mechanisms enable the recipient immune system to recognize foreign HLA proteins? What occurs in direct allorecognition? How does direct allorecognition differ from a typical T cell response to a foreign antigen? What factors can lead to a high frequency T cell response? How are T cells affected in a high frequency response? The (MLR) is an invitro correlate of direct allorecognition. Other than direct allorecognition, how does the immune system recognize foreign HLA protein? The interaction between MHC proteins and inhibitory KIRs. The NK cell encounters a reduction/lack of class I expression, which allows for unoccupied inhibitory receptors and an inhibitory signal loss occurs. Haploidentical stem cell transplantation. Recipients who lack corresponding class I MHC protein receive the donor inhibitory KIR. Alloreactivity by NK cells that repopulate the recipient after transplantation. Alloreactive NK cells Genetic relatedness of the donor and the recipient. Allografting. HLA disparity between donor and recipient. Strong cellular and humoral responses. Direct and Indirect allorecognition. Recipient T cells bind and respond directly to foreign (allo) HLA proteins on graft cells. The response is high frequency, up to 2% more T cells respond. Recognition of multiple amino acid disparities by multiple T cell clones, the presence of multiple different peptides on allogeneic that are each recognized by different T cell clones, and the presence of many foreign molecules per cells. Activation with low affinity, which normally would not be stimulated. Mixed lymphocyte response. The second pathway: indirect allorecognition. 32 Immuno PPT Flashcards Unit 3 How is indirect allorecognition analogous to the normal mechanism of recognition of foreign antigens? Indirect allorecognition plays a predominant role in: What does the effector response against transplanted allogeneic tissue include? How may an antibody result in cell death? What is variable in a rejection episode? Name the three types of transplantation rejection. When does hyperacute rejection occur? What mediates hyperacute rejection? What may elicit a hyperacute rejection? How does a hyperacute rejection lead to a thrombus formation? How does a thrombus formation affect the transplanted tissue? When is hyperacute rejection seldom encountered? Why are hyperacute rejection seldom encountered in clinical transplantation? How is the absence of donor HLA specific antibodies confirmed prior to transplantation? What effect has crossmatch testing, choosing ABO identical, and screening for the presence of pre-formed HLA antibodies on hyperacute rejection episodes? What complications can some individuals who possess very low levels of donor-specific antibody in the pretransplant period encounter? What has the antibody-mediated rejection that may take place over several days termed? It involves the uptake, processing, and presentation of foreign HLA proteins by recipient antigenpresenting cells to recipient T cells. Acute and chronic rejection. Direct cytotoxicity, delayed-type hypersensitivity responses, and antibody-mediated mechanisms. It may mediate antibody-dependent cellular cytotoxicity reactions and may fix complement. The time of occurrence and the effector mechanism that is operative. 1. hyperacute rejection 2. acute cellular rejection 3. chronic rejection Within minutes to hours after the vascular supply to the transplanted organ is established. It is mediated by pre-formed antibody that react with donor vascular endothelium. ABO, HLA, and certain endothelial antigens. With the binding of pre-formed antibodies to the alloantigens that activate the complement cascade and clotting mechanisms. It can result in ischemia and necrosis of the transplanted issue. In a clinical transplantation. Donor-recipient pairs are chosen to be ABO identical or compatible, and patients awaiting transplantation are screened for the presence of preformed HLA antibodies. The performance of a crossmatch test. These approaches have virtually eliminated hyperacute rejection episodes. Antibody-mediated rejection may take place over several days. Accelerated rejection. 33 Immuno PPT Flashcards Unit 3 What do hyperacute rejection and accelerated rejection have in common? How long does acute cellular rejection take to develop? Though acute cellular rejection is a cellular-type rejection, what other immunologic participant is also involved? What is characteristic of acute rejection? What types of immunological cells are predominately are found in interstitial cellular infiltrates? What roles do CD8+ and CD4 T cells play in interstitial cellular infiltrates? They both involve intravascular thrombosis and necrosis of donor tissue. Days to weeks after transplant. Antibodies. Parenchymal and vascular injury. CD8+ T cells, CD4 T cells, and macrophages. CD8+=Mediate cytotoxic reactions to foreign MHCexpressing cells CD4= Produce cytokines and induce delayed-type hypersensitivity (DTH) reactions. What role do antibodies play in acute Antibodies bind to vessel walls, activate graft rejection? complement, and induce transmural necrosis and inflammation. Do antibodies in hyperacute rejection No. and acute graft rejection play the same Hyperacute rejection= create a thrombosis. role? Acute graft rejection= bind to vessel walls, activate complement, and induce transmural necrosis and inflammation How has the development and The response to alloantigens has improved early graft application of potent immunosuppressive survival by reducing the incidence of acute rejection drugs that target multiple pathways in and providing approaches for its effective treatment. the immune response affected solidorgan transplants? What remains the most significant cause Chronic rejection. of graft loss after the first year posttransplant? Why is chronic rejection a significant It is not readily amendable to treatment. cause of graft loss? What is characteristic of chronic It is a process of graft arteriosclerosis characterized rejection? by progressive fibrosis, and scarring with narrowing of the vessel lumen due to proliferation of smooth muscle cells. What are the predisposing factors that Prolonged cold ischemia. impact the development of chronic Reperfusion. rejection? Acute rejection episodes. Toxicity from immunosuppressive drugs. What is chronic rejection’s suspected a) Delayed-type hypersensitivity reaction to immunologic component? foreign HLA proteins. What allogeneic response uniquely b) Graft-versus-host disease (GVHD). complicates stem cell transplants, and 34 Immuno PPT Flashcards Unit 3 less commonly, lung and liver transplants? Why do recipients of stem cells transplants for hematologic malignancies typically have depleted bone marrow prior to transplantation? Where do the stem cells that are infused for a transplant originate? What is the benefit of the infused products to contain some mature T cells? How would mature T cells have a negative effect to the transplant? When does acute GVHD occur? What is targeted in acute GVHD? Compare what occurs if there is an allogeneric mismatched stem cell transplantation versus a matched stem cell transplantation with GVHD. How do infused T cells can mediate GVHD? What correlates the incidence and severity of GVHD? Why are all the below actions done? immunosuppressive therapy in the early post-transplant. removal of T lymphocytes from the graph How can T cell reduction have a negative effect on the graft when it so effective in lowering the incidence of GVHD? What can occur beyond 100 days posttransplant? How does chronic GVHD resemble an autoimmune disease? What are some ways that immunosuppressive agents are used? How are immunosuppressive agents usually used to prevent graft rejection? Where is the growing list of agents used? How are the immunosuppressive agents used? What are the negative effects of using c) The chemotherapy used to treat the malignancy. d) Bone marrow or, more commonly, peripheral blood stem cells. e) Promotion of engraftment, reconstitution of immunity, and mediation of a graft-versusleukemia effect. f) Mature T cells may also mediate GVHD. g) The first 100 days of post-infusion. h) The skin, gastrointestinal tract, and liver. Mismatched: mismatched HLA proteins targeted. i) Matched: minor histocompatibility antigens are targeted. With massive release of cytokines due to large-scale activation of the donor cells by MHC mismatched proteins, and by infiltration and destruction of tissue. The match status of the donor and recipient, and other factors. Reduce the incidence and severity of GVHD. It can also reduce the graft-versus-leukemia (GBL) effect of the infused cells, and increase the incidence of graft failure. Patients may experience chronic GVHD. Fibrosis affects the skin, eyes, mouth, and other mucosal surfaces. Induction and maintenance of immune suppression and treatment of rejection. In combination of different immunosuppressive agents. To suppress anti-graft immune response in solidorgan and stem cell transplantation. Induction and maintenance of immune suppression and treatment of rejection. Increased susceptibility to infection, malignancies, 35 Immuno PPT Flashcards Unit 3 immunosuppressive agents? What do the following have in common? -corticosteroids -Anti-metabolic agents -calcineurin inhibitors -polyclonal antibodies What are corticosteroids? What are corticosteroids use for in high doses? How do corticosteroids function in immunosuppression? What effect do corticosteroids have on macrophages and leukocytes? What complications may arise from long-term use corticosteroids? What interferes with the maturation of lymphocytes and kills proliferating cells? What was the first anti-metabolic agent employed? Why has mycophenolate mofetil replaced the use of Azathioprine? What do calineurin inhibitors do? Name an example of a calcineurin inhibitor. How does inhibition of cytokine synthesis affect T cells? How does the block of T cell growth and differentiation beneficial for graft survival? How does Rapamycin inhibit T cell proliferation? What binds to cell surface molecules on the lymphocytes as induction agents and to treat severe rejection episodes? OKT3 is a mouse monoclonal antibody that binds to the on human lymphocytes. True or False. The binding of OKT3 to the CD3 T-cells surface has one outcome. What may render the affected T cells nonfunctional? and other associated toxic side effects. All are immunosuppressive antibodies. Potent anti-inflammatory and immunosuppressive agents used for immunosuppression maintenance. To treat acute rejection episodes. By blocking production and secretion of cytokines, inflammatory mediators, chemo-attractants, and adhesion molecules. Decrease macrophage function and alter leukocytetrafficking patterns. Hypertension and diabetes mellitus. Anti-metabolic agents. Azathioprine. Mycophenolate mofetil has a more selective effect on lymphocytes, and fewer side effects. Block signal transduction in T lymphocytes, resulting in impairment of cytokine synthesis, including IL-2, 3, 4, and interferon-Gamma. Cyclosporine and FK-506 (tacrolimus) Inhibition of cytokine synthesis blocks the growth and differentiation of T cells. It impairs the anti-graft response. By binding to specific intracellular proteins, including mammalian target of rapamycin (mTOR). Monoclonal antibodies. CD3 receptor False. Binding may modulate CD3 from the cell surface. 36 Immuno PPT Flashcards Unit 3 How do higher doses of antibody deplete T cells from circulation? What problem is there with monoclonal antibody preparations administered to patient? When are two polyclonal anti-T-cell antibody preparations used? Thymoglobulin is a an anti-thymocyte antibody prepared in . ATGAM is a polyclonal antiserum prepared from immunization of . Name the two immunosuppressive agents that are potent enough to deplete lymphocytes from the circulation. What activity can the development of these anti-mouse antibodies interfere with? What is the drawback associated with administration of polyclonal antibody preparations? What are the two main activities carried out by histocompatibility laboratories in support of transplantation? What is HLA typing? For clinical HLA testing, of the classical transplant antigens or genes are determined (HLA-A, B, Cw, DR, DQ). What information is used to find the most suitable donor–recipient combination from an immunologic standpoint? True or False. Histocompatibility is the only consideration given into the choice of a particular donor for any given patient. What is the classic procedure for determining the HLA phenotype? How are individuals HLA typed? Purified lymphocytes are used for HLA class I typing. Purified B lymphocytes are used for With complement-mediated lysis or opsonization for removal by phagocytic cells. The development of anti-mouse antibodies by the patient. To treat severe rejection. Rabbit. Horses. Thymoglobulin and ATGAM. The activity of the monoclonal antibody. The development of serum sickness due to antibody responses to the foreign immunoglobulin. HLA typing and HLA antibody screening/identification. The phenotypic or genotypic definition of the HLA antigens or genes in a transplant candidate or donor. Phenotypes or genotypes. Histocomplatibility. False. The complement-dependent cytotoxicity (CDC) test. Panels of antisera or monoclonal antibodies that define individual or groups of immunologically related HLA antigens are incubated with lymphocytes from the individual. T Class II. 37 Immuno PPT Flashcards Unit 3 HLA typing. When is the complement added in the complement-dependent cytotoxicity (CDC) test? Why is the dye added in the complement-dependent cytotoxicity (CDC) test? What can provide an extensive array of HLA antigens can be defined? True or False. There are several limitation to the CDC method for HLA typing. Why does the CDC method need viable lymphocytes? Separation of is required for definition of class I versus class II antigens. True or False. The source of anti-sera for HLA typing is not always consistent or reliable. What effect does the source of anti-sera have on reagents? What is the ability to distinguished too closely related yet distinct HLA antigens called? True or False. The level of resolution is limited Do the limits of resolution significantly impact the role of HLA phenotyping for matching solid-organ donors and recipients? When is a higher level of resolution required? Why are DNA-based (molecular) HLA typing methods are now commonly employed in histocompatibility laboratories? In clinical histocompatibility testing, amplification is detected by: Molecular-based HLA genotyping methods use polymerase chain reaction (PCR)–based amplification of HLA genes followed by: Which common approach to analysis amplifies specific alleles or related allele groups? After incubation with antisera. To distinguish live cells form dead when they are viewed microscopically. Complement-dependent cytotoxicity (CDC) test True. The CDC method demands timely performance of the assay. T and B lymphocytes True. The quality or quantity over time varies. The level of resolution. True. No. Unrelated stem cell transplantation. They address the limitations of CDC-based methods. Agarose gel electrophoresis. Analysis of the amplified DNA to identify the specific HLA allele or group of alleles. PCR amplification of HLA genes with panels of primer pairs. 38 Immuno PPT Flashcards Unit 3 What detects the amplification of the alleles or allele groups? Which primer pairs result in the detection of an amplification product? How is the HLA type(s) determined? What is referred to as generic amplification? What is the second common approach for HLA approaching? How is each specific or unique HLA allele identified after amplification? True or False. Only those probes that specifically hybridize to the amplified DNA will be detected. How is the HLA genotype determined? What is the third common method for HLA genotyping? True or False. HLA genotyping overcomes the limitation of CDC-based HLA phenotyping. Do cells need to be viable to obtain DNA for HLA genotyping? What is the benefit of HLA genotyping using chemically synthesized reagents? HLA genotyping can provide varying ( ) that can be tailored to the specific clinical need. What results can DNA-based testing provide? What is required for matching of unrelated stem cell donors and recipients? Antibodies to can be detected in candidates and recipients of solid-organ transplants. When can antibodies against HLA antigens develop? Why are patients awaiting solid-organ transplantation are screened periodically Agarose gel electrophoresis. The primer pairs that bind to the target gene. By indentifying which primers resulted in amplification. Performing a single PCR reaction that will amplify all HLA gene variants at a specific locus. Generic amplification. The amplified gene is then subjected to hybridization with a panel of DNA probes. True. Assessing which probes hybridized. Sequencing of PCR-amplified HLA genes. True. No. There is no reliance on human donors of anti-sera. Levels of resolution Results at a level of resolution comparable to CDCbased typing (antigen equivalent) or can provide allele-level results. Allele- level results from HLA genotyping. HLA antigens In response to multiple blood transfusions; two prior HLA-mismatched transplants; and, in women, to multiple pregnancies. Because of the potential adverse impact HLA antibodies can have on graft survival. 39 Immuno PPT Flashcards Unit 3 for HLA antibodies? When is a donor eliminated for consideration for donation to a specific patient with specific HLA antibodies? How often are patients tested for the presence of HLA antibodies while they are waiting for an organ offer? Why is antibody screening and identification also performed posttransplantation? True or False. The methods used for antibody detection and identification have changed significantly in recent years. The CDC method used for is also used for HLA antibody detection and identification. When the CDC method is used for HLA antibody detection and identification, panels of lymphocytes with defined HLA phenotypes are incubated with: When will the cognate HLA antigen be expressed? How is the binding of the HLA antibody to the panel of lymphocytes detected? True or False. In some scenarios, the level of antibody in a patient serum may be below a level detectable by the CDC assay. When the donor has those HLA antigens that the recipient possesses antibodies. Monthly. To aid in the diagnosis of antibody-mediated rejection, and to assess the effectiveness of therapy for antibody-mediated rejection. True. HLA typing The patient’s serum. When the patient serum contains HLA antibodies, and binds with the panel of lymphocytes. By addition of complement and a vital dye to assess cell death microscopically. True. Why is anti-human globular (AHG) added to a CDC assay? To increase the test sensitivity because the AGHCDC assay can detect lower levels of antibody as wells as isotypes of bound antibody that don’t activate complement and thus wouldn't normally be detected in the standard CDC assay. What is referred as percent panel reactive The proportion of lymphocytes in the panel that are antibody (%PRA)? killed by the patient’s serum. Usually how many unique lymphocyte 30-60 preparations are included in the panel? How can the specificity of the antibodies Evaluating the phenotype of the panel cells. be determined? What has been developed as a substitute Enzyme-linked immunosorbent assay (ELISA) for CDC-based HLA antibody testing? What utilizes purified HLA antigens ELISA assays bound to the wells of microtiter plates? 40 Immuno PPT Flashcards Unit 3 When will patient serum added to the wells of the plate bind to the antigen? How is the bound antibody detected? When is there a color change in an ELISA assay? What do the wells of the ELISA plate provide because it may contain a pool of HLA antigens? How can ELISA be analogous to a CDCbased analysis by allowing percent PRA and specificity to be determined? Name another approach, not previously discussed, for antibody detection and identification. Antibody in patient serum can be incubated with latex beads that are coated with: True or False. Flow cytometry can incubate either single donor or a single purified HLA protein. How is the bound antibody in flow cytometry detected? What is the most sensitive method for detecting HLA antibodies? When flow cytometric methods can provide the most specific determination of the specificity of HLA antibodies? What test is performed once a donor has been identified for a particular patient? Why donor–recipient crossmatch test is performed? Why donor lymphocytes are incubated with recipient serum in a CDC assay? What is the alternative way to detect binding of antibody? As for antibody screening and identification, what is the most sensitive method for detecting donor-specific antibody? How to define tumor immunology? How is understood tumor immunology? HLA-specific antibody is present. With the addition of an enzyme-labeled antiimmunoglobulin reagent. When the addition of the substrate detects bound antibody in the wells. Serve as a qualitative screen for the presence of HLA antibody in a serum. Each well of the ELISA may contain HLA antigens representing a single donor. Flow cytometry. HLA antigens. True. By adding an FITC-labeled anti-IgG reagant. Flow cytometric methods When beads coated with a single HLA antigenic type are used. A donor–recipient crossmatch test. To confirm the absence of donor-specific antibody. To verify a lack of binding as detected by microscopic analysis after addition of a vital dye. By flow cytometry using an FITC-labeled anti- IgG reagent. The flow cytometric crossmatch It is a study of the antigens associated with tumors, the immune response to tumors, the tumor’s effect on the host’s immune status, and the use of the immune system to help eradicate the tumor It is best understood with the background on 41 Immuno PPT Flashcards Unit 3 Why normal cell growth and division are regulated processes? How do we name the regulatory genes that promote cell division? What protooncogenes can cause? What can cause tumors? What cells form tumors? If a tumor does not invade surrounding tissue and normal body function is largely preserved, it is said to be? What tumors invade surrounding tissues and greatly disrupt normal body function? What is the stage when the malignant cells travel through the body, causing new foci of malignancy until body function is so disrupted that death occurs? How malignant cells typically differ visually from normal cells? differences between tumor cells and normal cells. It is designed to rapidly produce new cells when necessary, inhibit cell division when sufficient cells are present, and limit cell lifespan (programmed cell death, or apoptosis). Protooncogenes They uninhibit cell division if their expression is altered or if they are mutated into oncogenes. Mutations or malfunctions in tumor suppressor genes that remove growth-inhibitory signals. Cells that possess many of the attributes of the normal cells from which they arose but have accelerated or dysregulated growth. Benign tumor. Malignant tumors. Metastasis. They are metabolically more active to support their growth, and express different genes or different levels of gene products as compared to normal cells. Leukemic cells. What cells have aberrant morphology and express different surface antigens either in type or amount? Is the conversion of a normal cell to a It is a process. malignant cell is typically a process, or an event? What is the phase when cells are exposed Induction phase. to a variety of environmental insults, including chemical carcinogens, oncogenic viruses, and radiation (ionizing and ultraviolet)? Why cancer is developed? It is the result of multiple mutations caused by these insults. In what cells cancer can develop faster? It more readily develops in cells genetically predisposed to mutations. How long takes the induction phase? It may take months to years. What happens during the induction Cells exhibit dysplasia or abnormal growth that is not 42 Immuno PPT Flashcards Unit 3 phase? What is the phase of cancer when neoplastic cells have formed but are confined to the tissue of origin? When cells are malignant, the cancer proceeds to what phase? What happens during the invasion phase? Why detection is difficult in the early stages? yet considered neoplasia, or consistent with a tumor. In situ phase. Invasion phase. Cancer proceeds to dissemination throughout the body, usually via the blood and lymphatics. There are fewer cells to detect and they more closely resemble normal cells if they are dysplastic rather than neoplastic. The progeny of the cell that undergoes transformation are monoclonal in origin. Rapid uncontrolled proliferation. Why cells are initially identical phenotypically and genotypically? What is the cause of DNA replication, developing cellular phenotypic and genotypic heterogeneity? What helps cancer cells escape from both The ability to mutate. the immune system and from chemotherapeutic agen? What is the complication of mutation? It complicates identification of reliable tumor markers, as marker expression may change over time. What is the classification of tumors that Poorly differentiated, or anaplastic tumors. are more similar to fetal or embryonic tissue? What is the classification of tumors that Well-differentiated tumors. are more similar to normal tissue? What tumors are more aggressive and Poorly differentiated tumors. lead to poorer patient prognosis? What is the meaning of the TNM system. Classification of tumors by the size of the primary tumor (T), the involvement of adjacent lymph nodes (N), and the detection of metastasis (M). What is the term used to describe the Immunosurveillance. processes by which cells of the immune system look for and recognise foreign pathoges such as bacteria and viruses, or pre-cancerous and cancerous cells in the body? Where do we see increased incidence of In individuals with deficient immune systems such as tumors formation? the elderly and in immunosuppressed individuals, but this is not proof of the existence of Immunosurveillance. What is the cause of tumors Increased lifespan implies increased exposure to development? carcinogens. In what individuals many tumors are In immunosuppressed people. essentially infections, as they are of viral 43 Immuno PPT Flashcards Unit 3 rather than spontaneous origin? Why tumors in immunosuppressed people are infectious? Why would the incidence of nonviral tumors in T cell-deficient individuals be not increased? What cell are present in some tumors, and are associated with a better prognosis? What is the common characteristic of many tumors that allows tumor cells to escape from T cells? What is the work of some successful therapeutic advances? What do we observe in certain therapeutic advances? Why it is possible that Immunosurveillance itself is ultimately responsible for tumors that can escape the immune system? When it is important to determine mechanisms by which tumors escape? When some tumor antigens may be poorly immunogenic? What tumor cell may lack? What kind of resistance can be observed in tumors in people with deficient immune systems? What prevents interaction with the tumor cell? What other elements cause some tumors to be immunosuppressive? What are the local environments? In what phase of immunosurveillance, tumors are sufficiently immunogenic to be eliminated by the immune system? During what stage as mutations occur over time, cells that are less immunogenic have a growth advantage? In what phase cancer cells have mutated beyond the immune system's ability to control them? What research has been made of tumor immunosurveillance? Because they are of viral rather than spontaneous origin. This may be due to adequate NK cell activity, although these topics are still under study. NK cells, T lymphocytes (tumor infiltrating lymphocytes [TIL]), and macrophage infiltrates. Loss of MHC expression and subsequent poor antigen presentation. They are directed toward upregulating the immune system to fight a particular cancer. Spontaneous regression of some tumors. It is because of immunoediting. If Immunosurveillance is indeed occurring. If they are very similar to normal self antigens and induce immune tolerance. MHC class I, class II, or accessory molecule expression. Resistant to the immune response, or the tumor's growth rate regulation by the immune system. When soluble antigen released by the tumor may bind to the T cell receptor. Local environment. Immunosuppressive cytokines such as transforming growth factor-beta. Elimination phase. Equilibrium stage. Escape phase. To immediately determine the extent and precise mechanisms. 44 Immuno PPT Flashcards Unit 3 What research is still ongoing? What antigens are present in the tumor tissue in higher amounts than in normal tissue? What are the products of mutated genes and viruses? What is the other way that tumorassociated antigens can be present? What antigens are most highly expressed in both normally developing fetal tissue and in certain kinds of cancers? Why virtually no tumor-associated antigens are tumor specific? What is the perfect tumor-associated antigen needed for detection? What tests are used in ostensibly normal people to detect occult cancer? What tests are those that help determine differential diagnosis, tumor stage, prognosis, and therapy selection? What profoundly impacts the test’s usefulness? What supports the probability calculation? What are the points in Bayes’ theorem? What it means 99% sensitivity and 95% specificity? What if the cancer rate in the population is 0.1%? What if the cancer rate in the population is 1%? What if a clinician can identify this cancer by signs and symptoms 75% of the time? Why tests for differential diagnosis, generally perform relatively well? What are the presumptions for screening tests? Research into the manipulation of the immune system to fight cancers. Tumor-associated antigens (TAA). Tumor-associated antigens (TAA). They can also arise from aberrant expression of normal genes. Oncofetal tumor antigens. Because they also have been found in some noncancerous human tissue. It should be unique to a particular timber could aid in the screening, diagnosis, history of pathic evaluation, staging, monitoring, localization, and immunotherapy of various malignancies Screening tests. Diagnostic tests. Disease prevalence. Bayes’ theorem. A “good” cancer test with 99% sensitivity and 95% specificity. Test will be positive in 99 out of 100 people with disease, and it will be negative in 95 out of 100 people without disease. Then 98 percent of positives would be false positives. The false-positive rate is still 83 percent. The false-positive rate is 1.7 percent. Because the clinical suspicion of cancer translates to a higher cancer prevalence in the population being tested. Relatively low number of people being screened actually have cancer and that it would be worse to miss a cancer then to do further testing on a normal 45 Immuno PPT Flashcards Unit 3 Why the concept of a normal or reference range does not really apply? What type of values are typically selected above the point at which further testing will be done? How are the cutoff values for screening tests generally set? person to exclude cancer. It may be difficult to determine with certainty that a reference population does not have cancer, and values from normal and cancerous populations may overlap. Cutoff values for tumor markers. These are set with the expectation that there will be an extremely high number of false positives due to low disease prevalence. How can the additional testing be? Invasive, costly, or anxiety-provoking. What conditions are needed for The tumor is an important health problem, there is a widespread use of a laboratory test to recognizable early symptom or marker that can be screen for cancer? used for screening with reasonably high sensitivity and specificity What is included in the cost of laboratory Longer morbidity in patients whose prognosis is not tests? changed, overtreatment of questionable diagnoses, misleading reassurance for those with false-negative results, and anxiety and possible morbidity from more invasive testing for those with false positive results. What is the principle of lab test? It is a tumor for which treatment at an early stage is more successful than at a later stage. What are the advantages of tests? Costs and benefits of the screening test are acceptable to the population; including improved survival time, less radical treatment needed for tumors detected earlier, and reassurance for those with negative results. What includes cost of lab tests? Longer morbidity in patients whose prognosis is not changed, over treatment of questionable diagnoses, misleading reassurance for those with false-negative results, anxiety and possible morbidity from more invasive testing for those with false-positive results, the actual physical hazards of the screening test, and the actual dollar costs of the screening test. What needs to be done to improve the Selected subgroups, such as patients with a family cost-to-benefit ratio? history of cancer, should be screened when possible instead of the entire population. How differential diagnosis of tumor type By tissue/cell morphology and detection of tumor can be done? markers directly from tumor tissue. What techniques are required for Immunohistochemistry; detection of expressed detection of tumor antigens? antigens using labeled antibodies; and fluorescent in situ hybridization (FISH). What can be detected by Expressed antigens using labeled antibodies, and immunohistochemistry? molecular techniques such as fluorescent in situ 46 Immuno PPT Flashcards Unit 3 What can be detected by FISH? What is the principle of lab test? What can be helpful in pathological diagnosis? Why markers must be combined with other clinical results? What is relatively common in performing lab test using markers? What can happen if the DNA changes in malignant transformation? How is done the disease management with laboratory tests? What is established for the lab test? What is done if the disease and treatments progress? What is important in clinical usage of tumor markers? What must be done by the same methodology so that changes are due to actual alterations in the patient, not differences in methods? What are the dilemmas associated with tumor markers. Why detection of PSA is very specific for the prostate gland and increases in almost all prostate cancers? How is the production of PSA related in a healthy men? What may happen when men age? hybridization (FISH). Normal gene expression using nucleic acid probes. Differential diagnosis by the pathologist are less stringent than the requirements for using tests for widespread screening. The marker must be differentially expressed in the tumor of origin and other tumors, which may have similar appearance histologically. The differentiation that occurs with transformation sometimes can result in loss of the marker. False-negative results. This sometimes can cause expression of a marker that is not normally associated with the tumor type in question, although this occurrence is relatively uncommon. It is typically done with serial determinations of a tumor marker. A baseline level at initial diagnosis. Additional levels are determined to establish prognosis, monitor the results of therapy, and detect recurrence. It is not the absolute value of the tumor marker that is important but rather the upward or downward trend when the marker’s biological half-life is considered. Serial determinations done to aid the clinician in making important decisions concerning the therapeutic regimen. Problems with prostate-specific antigen (PSA). It is because no other tissue in men is known to produce PSA. The amount of PSA produced is directly related to the glands size. Many men developed benign enlarged prostate, further, they are more likely to develop prostate cancer, but they are less likely to die from it. What sometimes should be done if as There are prostate cancers that can and should be left men age and develop prostate cancers? alone. What is recommended for PSA screening It should be done once a man's remaining life cease? expectancy is less than 10 years. What has been done in lab testing for It is possible to discriminate between benign PSA? prostatic hypertrophy, weekly aggressive cancers, and highly aggressive cancers using PSA. 47 Immuno PPT Flashcards Unit 3 What is more associated with cancer and his justification for a biopsy? Why the net benefit to the widespread PSA screening currently done in the United States a be questionable? What are the variety of methods that clinicians screen for the presence of malignancies? What is the advantage of laboratory tests? What are the three types of laboratory methods for cancer screening and diagnosis? Why the choice of method often depends on convenience, cost, sensitivity, and specificity? How pathologist and histology labs process suspected tumor tissue? What is the process to enhance the visible features? What is the feature of evaluation of morphology and staining patterns? What is required to accurately diagnose cancer by morphology alone? How is the final diagnosis often made? What include some of the molecular diagnostic techniques that have become increasingly routine? What is the purpose of cytogenetics studies? What is the purpose of nucleic acid amplification techniques? What is the purpose of fluorescent in situ If the free-to-bound ratio of PSA is low or the rate of PSA is increasing at a rate that exceeds 0.5 NG/ML per year (PSA velocity). It is due to the fact that an increased PSA does not always indicate a cancerous state or an aggressive cancer that must be treated. Commonly used tests include stool occult blood and colonoscopy for colorectal carcinoma, tests for cervical cancer, self-exams for breast and testicular cancer, mammogram for breast cancer, and digital rectal exam for prostate cancer. These tests can provide important adjunct information to patient histories and physical examinations. These are gross and microscopic morphology of tumors; detection of antigen/protein tumor markers; and DNA/RNA molecular diagnostics. Because these techniques are complementary in that many of the DNA changes and subsequent mRNA expression result in the altered antigens/proteins detected or morphology visualized. It is done with gross dissection and preparation of slides for microscopic analysis. A variety of special stains, nucleic acid probes, and tumor marker antibodies can be applied to the slides. It can be very subjective, and classification categories can be rather broad. Considerable skill. It is done with supplemental clinical information and additional testing. These are cytogenetic studies; nucleic acid amplification techniques by polymerase chain reaction (PCR) and its variants; and fluorescent in situ hybridization (FISH). More precise knowledge of the exact gene defects present in various cancers is gained, testing for the aberrant genes is becoming prevalent. Polymerize chain reaction (PCR) and its variants increase the inherent level of DNA or RNA, allowing the detection of small populations of cancer cells (including circulating cells in metastatic sis) and the detection of mutagens, deletions, and gene rearrangements/translocations. Nucleic acid probes capable of binding to sequences 48 Immuno PPT Flashcards Unit 3 hybridization (FISH)? What are other similar techniques using non-fluorescent labels? What tests for genetic screening of cancers are available? What available marker for CML is a well-respected? What is almost exclusively present in multiple myeloma or other lymphoid malignancy? What is the cause of most other phenotypically related cancers? What are the future tests that are currently being developed with multiple nucleic acid tests contained on a single chip to allow for simultaneous testing of a sample for multiple genes? What is the potential use of micro-array tests? What are the genetic abnormalities associated with an increased risk of developing a cancer or with a poorer prognosis? What is an example of a prognostic marker? What is the feature of Her2/neu oncogene in breast cancers? What are the characteristics of ideal tumor marker? What are other characteristics of ideal tumor marker? What are other characteristics of ideal tumor marker? What are the characteristics of ideal tumor marker? What are the seven categories of tumor markers detection? of interest are tagged with fluorophores and applied to cells. Cells containing the sequence of interest can be visualized with fluorescent microscopes. Enzymes and silver stains. DNA/RNA sequences. The BCR-ABL translocation. Monoclonal expression of B cell DNA rearrangement. They have heterogeneous genetic causes, so universal and reliable genetic abnormalities are not yet described. Micro-array test. Detection and semi quantitation of mRNA expression in cells to distinguish patterns (rather than single markers) consistent with cancer. Susceptibility genes like the BRCA-1 and BRCA-2 mutations linked with an increased risk of breast, ovarian, and prostate cancers. Overexpression of the Her2/neu oncogene. It tend to be more aggressive but will more likely respond to certain therapies (trastuzumab). It must be produced by the tumor or as a result of the tumor and must be secreted into some biological fluid for analysis. Its circulating half-life must be long enough to permit its concentration to rise with increasing tumor load. It must increase to clinically significant levels (above background control levels) while the disease is still treatable and with few false negatives (sufficient sensitivity). The antigen must be absent from or at background levels in all individuals without the malignant disease in question to minimize false-positive test results (sufficient specificity). Cell surface markers, proteins, oncofetal antigens, carbohydrate antigens, blood group androgens, 49 Immuno PPT Flashcards Unit 3 How are most of these makers detected? Why tumor markers are not always directly associated with the malignant transformation? What is an example of these tumors? How many tumor markers are approved by FDA? What tests are used with a notation on the lab report stating that the results are for research use only Who has developed a set of very useful consensus guidelines regarding the clinical use of tumor markers? What the National Academy of Clinical Biochemistry has on their list? What current testing guidelines recommend? What is used to identify and quantify an array of proteins simultaneously present in a sample? What is the new field in tumor markers this is currently only at the research stage? What is the purpose of protein profiling in cancer patients? enzymes/iso enzymes, and hormones. By immunologic methods with antibodies to distinct epitopes on the molecules. Often, they are the normal products of tissue of origin being expressed, and this is more likely if the tumor is well differentiated. Endocrine gland tumors often produce generous amounts of hormone that the tissue of origin produces. Less than a dozen. Non-FDA-approved markers. The National Academy of Clinical Biochemistry. Methods and markers for a variety of purposes that have acceptable evidence of validity. Very few markers for screening/early detection and still recommend using adjunct tests or screening high-risk populations. Mass spectrometry (MS). Oncopeptidomics. It will aid in the discovery of new tumor markers or patterns of protein expression that are consistent with cancer. What is the purpose of oncopeptidomics? It may allow more subtle increases of tumor markers to have diagnostic significance, since multiple markers can be measured and the overall pattern assessed, but this is currently only at the research stage. What are some important aspects to Most tumor markers are detected using antibodies laboratory testing for tumor markers? because of the specificity of antibodies and the general reliability of immunoassays. Why there are some important Antibodies are directed at specific epitopes, and the limitations to using antibodies as antibodies from different manufacturers may vary reagents? greatly in terms of what is measured, particularly if monoclonal antibodies are used. Why it important to use the same method Because antibodies from different manufacturers for monitoring patients over time, and may vary greatly in terms of what is measured. 50 Immuno PPT Flashcards Unit 3 clinicians should be aware of this if patients change clinics or laboratories? What must be done if laboratories switch methods? What is the specificity of antibodies employed in tumor marker assays? What is particularly problematic when antibodies are employed in tumor marker assays? What some tumors may produce? What is the phenomenon similar to the prozone in immunoassays? Why it is critical that criteria be developed to identify situations in which the hook effect may be present? What are other related problem of antigen excess in automated systems? Why heterophile antibodies in specimens can interfere profoundly with results? What happened in a tragic case involving false-positive hCG results from an automated analyzer? With what antibodies false increases and false decreases are associated? What is the purpose of commercially available antibody-blocking reagents? Why specimen that may have heterophile antibodies should not be reported until the issue is resolved? Whatis the final aspect of tumor immunology to be discussed? What aspect has long intrigued scientist? What are the two types of immunotherapeutic methods? What is the method that involves transfer of antibody, cytokines, or cells to patients who may not be able to mount an immune response? What is the method that patients are treated in a manner that stimulates them They must provide a transition period during which specimens are measured by both methods and specimens are archived until new data is established for each patient. It is not absolute. Antibodies will cross-react with similar structures and there is problem when these are in excessive amounts, as can occur in cancer. Massive amounts of tumor marker molecules. It has been called the high-dose hook effect. Specimens can be diluted and accurate results obtained. It is specimen carryover, so in addition to diluting the specimen with excessive antigen, the specimen being tested immediately after it may need to be repeated. Because many of the antibodies used in immunoassays are animal in origin. Several women had unnecessary chemotherapy or hysterectomies for presumed undetected cancer. Heterophile antibodies. They block heterophile antibodies in suspicious specimens. Specimens exhibiting nonlinear behavior on dilution or with discrepant results using different methods or after applying antibody-blocking reagents. Immunotherapy. The possibility of stimulating the patient’s own immune system to respond to tumor-associated antigens. Passive or active immunotherapy. Passive immunotherapy. Active immunotherapy. 51 Immuno PPT Flashcards Unit 3 to mount immune responses to their tumors? Why passive transfer of allogeneric cellular immunity from one person to another to fight cancer has many barriers? What is more likely to be successful than passive transfer? What method brings improved patient prognosis? What method is theoretically possible? What is the model of adoptive T-cell therapy? What is the reason for recipients to be immunosuppressed? What is the one strategy in this model to treat GVHD? What happens when allergenic T-cells are genetically engineered? What are the other strategies for adoptive T-cell therapy? Why patient is lymphodepleted? What other cells can be harvested? Why new lines attempts have also been made? What is mostly used for passive transfer of antibody to treat cancer? What could be induced against "Naked" monoclonal antibodies against cancer? What could trigger antibodies if they are directed towards particular receptors? What are the antibodies conjugated to toxins or radioisotopes on the premise that they can kill cancer cells while leaving adjacent cells intact. What is needed for the passive immunotherapy to work? What is needed for the passive immunotherapy to work? What is needed for the passive Because of possible recipient rejection of foreign cells, graft-versus-host disease, and the fragility of live cells, although research models are being studied. Inducing a patient's own cellular immunity. GVHD called graft versus leukemia that has been demonstrated with transfer of allogeneric T cells. Successful passive transfer of anticancer T cells. T cells from allogeneric donors can be immunized against tumors. They receive T-cells to prevent rejection and to eliminate T suppressor mechanisms. It is to genetically engineer the allergenic T cells with a "suicide switch". This genes make cells vulnerable to a drug that will immediately eliminate them in the event of GVHD. Use of autologous T cells, tumor-infiltrating lymphocytes (TILs) can be harvested and expanded in vitro using IL-2. To remove T suppressor cells, and high concentration of TILs are transfused. Autologous T cells that are exposed to cancer antigens, expanded with IL-2, and then returned to the patient. To insert genetically engineered T-cell receptors into autologous T cells. Monoclonal antibodies. Antibody -dependent cell-mediated cytolysis (ADCC), complement-mediated lysis, or opsonization. Desirable action in the cell such as inducing apoptosis or inhibiting growth signals. Antibody conjugates, or immunotoxins. Antibodies must be directed at a cell surface antigen with high density. The antigen must be present on the primary tumor and on all the metastatic foci. Normal tissues must be free from the antigen or not 52 Immuno PPT Flashcards Unit 3 immunotherapy to work? What is needed for the passive immunotherapy to work? What are some obstacles involved in immunotherapy with antibodies? What other obstacles could be involved in immunotherapy with antibodies? What is significant in patients receiving therapy? Immunotherapeutic antibodies are most effective against what diseases? Why antibodies poorly penetrate tumor mass? Why antibodies are rarely, if ever, used alone? What is usually recommended in treating tumors? Why radiolabeled antibodies are particularly effective? Why radiolabeled antibodies are advantageous for tumors with heterogeneous antigen expression? What is the additional use for radiolabeled antibodies? Why the usage of radiolabeled antibodies must be managed? Are there any FDA-approved antibodytoxin conjugates available? How conjugation can theoretically allow the use of ”ultratoxic" drugs and some extreme cytotoxins? What cytotoxins are under study? Why antibodies must bypass the normal susceptible to the toxin. The antibodies must have sufficient access to the tumor tissue. Tumor heterogeneity with regard to antigenic expression; antigenic modulation or the loss of antigen from the tumor cells; failure of antibodies to penetrate tumor tissue and failure of antibody-toxin conjugates to internalize into the cell after binding and release of toxins. Toxic effects on other tissues, particularly the hematopoietic organs; the limited amount of toxin that can be linked to the antibody without destruction of binding activity; host immune response to the injected antibody and circulating antigen forming immune complexes with the antibodies, removing them from circulation. Development of heterophile antibodies. Hematologic malignancies, small tumors, and micro metastases, not bulky tumors. Because they are large molecules, and they bind to the first available antigen encountered on the outside of the tumor. Since there is usually more than one path for cell growth and surgical removal or debulking of a tumor is also possible. Combination therapy with chemotherapeutic agents or other treatments. Because of the "bystander" or "crossfire" effect seen with high-energy isotopes that can kill up to several hundred cells. It could allow antibodies to kill cells that are not expressing antigen at all. Imaging studies to locate foci of cancer. To minimize bone marrow toxicity, although this toxicity is generally reversible. No, besides one substance for T cell lymphoma. Because the agents delivery is limited and focused by the antibody. Diphtheria toxin, Pseudomonas exotoxin, abrin, ricin and saporin. Because toxins have their own binding mechanisms. 53 Immuno PPT Flashcards Unit 3 mechanism or the toxin must be modified? Why some cytotoxins must be internalized to be effective? What is the goal of active immunotherapy? What is used as nonspecific stimulation in active immunotherapy? What is still treated by Bacillus Calmette Guerin (BCG)? What is the use of novel adjuvants and selective use of stimulatory cytokines (TNF-α, IFN-γ, IL-1, IL-2)? What are other attempts at stimulating host immune systems? What is used for stimulation of immune system? Why cancer vaccinations have been of great interest to researchers? So the antibody must target an epitope that would be internalized. It is to have the patient develop an immune response that will help eliminate the tumor. Adjuvants such as Bacillus Calmette Guerin (BCG). Superficial bladder cancer. In immunocompetent patients to enhance the natural antitumor response and the artificial vaccine-induced response. Transfection of normal cells or isolated tumor cells with genes for cytokine production and injection of the modified cells into or around the tumor. This has been done with many cytokines. When specific viruses are associated with the cancer, vaccine construction is relatively straightforward, since viral antigens are obviously foreign. What is an excellent example of cancer The vaccine for human papilloma virus "HPV" to vaccines? prevent cervical cancer. Why vaccines must be protective against Many viruses have several serotypes and not all of the appropriate epitopes? which may be associated with cancer. What is the feature of HPV vaccines? They are directed epitopes that prevent initial infection with carcinogenic serotypes but do not help treat established cervical cancer, as these epitopes are down regulated in cancer cells. Is there a distinction between Yes. prophylactic vaccines and therapeutic ones? Why prophylactic vaccination is more Since many of the antigens expressed on tumors, difficult in the absence of a viral cause of appear to some degree on normal tissue. cancers? What cells are often deleted by tolerance Hi-affinity cytotoxic T lymphocytes against tumorpathways? associated antigens (TAA). Why the expression of an antigen on a Since coexpression with MHC I and obligatory tumor does not automatically make it a accessory molecules is required for adequate T cell suitable vaccine target? response. Why vaccination with tumor lysates and Due to the heterogeneity of antigens presented on peptide antigen vaccines have had tumors limited success? Why vaccination with tumor lysates and Due to the few "public antigens" common to all peptide antigen vaccines have had tumors limited success? 54 Immuno PPT Flashcards Unit 3 Why vaccination with tumor lysates and peptide antigen vaccines have had limited success? What is more difficult in designing vaccines? What various strategies have been attempted to identify sufficiently immunogenic antigens and how to present them to T cells? What is prime dendritic cells? What immunity can stimulate the strategy to prime dendritic cells? What can stimulate the strategy to prime dendritic cells? What is the general principle of prime dendritic cells technique? How should be done antigen exposure in prime dendritic cells technique? How should be done antigen exposure in prime dendritic cells technique? How should be done antigen exposure in prime dendritic cells technique? How should be done antigen exposure in prime dendritic cells technique? How should be done antigen exposure in prime dendritic cells technique? How the DC's are reintroduced in a patient? What are needed to demonstrate completely success vaccines? What are needed to demonstrate completely success vaccines? What are needed to demonstrate completely success vaccines? Why are immunization protocols important? What is the first step of traditional tumor therapy? In tumor therapy what will eradicate immune system after tumors will be debulked? What is the reason of active study and increased optimism in recent years? The specific immune response to bacterial infections includes formation of what? Due to the many "private antigens" you need to an individual's tumor. Designing custom vaccines for each individual The strategy to prime dendritic cells Particularly potent antigen-presenting cells Both: humoral and cellular Immune tolerance reactions DC line is cultured from the patient and then exposed to tumor antigen By using co-culture with purified tumor antigens By using co-culture with purified tumor lysate By using fusion of DC's with tumor cells By using DC phagocytosis of dead tumor cells By using transfection of RNA Intravenously, subcutaneously, etc. as a vaccine The details of optimal antigens DC priming Modes of DC delivery Protocols are important adjunct to traditional therapies Tumors will first be de-bulked Residual tumor and micro metastases The increased understanding of tumor immunology antibodies 55 Immuno PPT Flashcards Unit 3 Antibodies in a response to bacterial infection are produced to what? Antibody formation is the main defense against what bacteria? What is helpful in attacking intracellular bacteria? Why Bacteria have developed several ways? Why Bacteria have developed several ways? What is one of the mechanism of bacterial development to inhibit immune response? What is one of the mechanism of bacterial development to inhibit immune response? What is one of the mechanism of bacterial development to inhibit immune response? How does the mechanism of avoiding the effects of antibody occur? The mechanism of avoiding the effects of antibody through altering bacterial antigens (epitopes) as a result of what? How some bacteria can avoid effect of antibodies? How some bacteria can avoid effect of antibodies? What is a target of most of the evasion mechanisms of bacteria? What are the stages of bacterial defense in the process of phagocytosis? What is an additional mechanism of resisting digestion? What are trigger the release of lysosomal contents into the cytoplasm of the phagocytic cells? What is a result of the release of lysosomal contents into the cytoplasm of the phagocytic cells? What is the major defense of some bacteria? Gram-positive spherical, ovoid, or lancet-shaped organisms are Bacteria that catalase negative and are often seen in pairs or chains are to exotoxins or other secreted bacterial products extracellular bacteria cell-mediated immunity to inhibit the immune response make it more difficult for the immune response to occur avoiding antibody blocking phagocytosis inactivating the complement cascade through altering bacterial antigens (epitopes) genetic mutations By down-regulation of MHC molecules produce proteases that degrade IgA the process of phagocytosis chemotaxis, adhesion, and digestion production of toxins production of toxins Killing these cells to block the action of complement Streptococci Streptococci 56 Immuno PPT Flashcards Unit 3 Streptococci are divided into groups or serotypes on the basis of what? What cell wall components are the basis for dividing Streptococci into groups? Interior to the protein layer is How many defined groups are divided Streptococci by the group-specific carbohydrate? How are 20 groups of Streptococci designated? What is the name of Streptococci groups that are divided by group-specific carbohydrate? What do some strains possess outside the cell wall? What does contribute to the bacterium’s antiphagocytic properties? What are additional virulence factors? What are exoantigens or exotoxins? Proteins excreted by the bacterial cells as they metabolize during the course of streptococcal infections are Detection of host antibodies to exotoxins is important in the diagnosis of what disease? Antibodies are produced to what exoantigens or exotoxins? Antibodies are produced to what exoantigens or exotoxins? Antibodies are produced to what exoantigens or exotoxins? Antibodies are produced to what exoantigens or exotoxins? Antibodies are produced to what exoantigens or exotoxins? What diagnosis must be used to identify rheumatic fever and glomerulonephritis? Why do serological diagnosis used to identify rheumatic fever and glomerulonephritis? What do group A streptococci elaborate? The antibody response to one or more of exotoxins of group A streptococci is used as The antibody response to streptococcal products is variable due to what factor? certain cell wall components M and T proteins the group-specific carbohydrate 20 A–H and K–V Lancefield groups hyaluronic acid capsule a hyaluronic acid capsule outside the cell wall Exoantigens or exotoxins proteins excreted by the bacterial cells Exoantigens or exotoxins glomerulonephritis and acute rheumatic fever streptolysin O deoxyribonuclease B (DNase B) Hyaluronidase nicotinamide adenine dinucleotidase (NADase) Streptokinase Serological Because the organism is unlikely to be present in the pharynx or on the skin at the time symptoms appear more than 20 exotoxins documentation of nonsuppurative disease age of onset 57 Immuno PPT Flashcards Unit 3 The antibody response to streptococcal products is variable due to what factor? The antibody response to streptococcal products is variable due to what factor? What is one of the most diagnostically important antibody? What is one of the most diagnostically important antibody? What is one of the most diagnostically important antibody? What is one of the most diagnostically important antibody? Assays for detection of antibodies can be performed individually or by using what kit? Streptozyme kit is useful because The onset of clinical symptoms of rheumatic fever or glomerulonephritis typically coincides with what? What is considered significant if acute and convalescent phase sera are tested in parallel? Why using of at least two tests for antibodies to different exotoxins is recommended? The most commonly used tests are Antihyaluronidase tests are available for Presence of what factor does indicate recent streptococcal infection in patients suspected of having acute rheumatic fever or poststreptococcal glomerulonephritis? The classic hemolytic method for determining what factor was the first test developed to measure streptococcal antibodies? What test is based on the ability of patient antibodies to neutralize the hemolytic activity of streptolysin O? What standard is used when ASO titer is expressed in Todd units? What standard is used when ASO titer is expressed in international units? The ASO titer may be expressed in what unit? The ASO titer may be expressed in what site of infection timeliness of antibiotic treatment antistreptolysin O (ASO) anti-DNase B anti-NADase antihyaluronidase Streptozyme kit detects antibodies to all streptococcal products with the peak of antibody response fourfold rise in titer because production of detectable ASO does not occur in all patients antistreptolysin O (ASO) and anti-DNase B research or reference laboratories antibodies to streptolysin O the ASO titer The classic hemolytic method for determining the ASO titer streptolysin reagent the WHO international standard Todd unit International unit 58 Immuno PPT Flashcards Unit 3 unit? The range of expected normal values of ASO titer is depends on what? The range of expected normal values of ASO titer is depends on what? The range of expected normal values of ASO titer is depends on what? Single ASO titer is considered to be moderately elevated if the titer is Single ASO titer is considered to be moderately elevated if the titer is ASO testing is currently more commonly performed by what method? When do ASO titers typically increase? When is the peak of ASO titer? Testing for the presence of what factor is clinically useful in patients suspected of having glomerulonephritis preceded by streptococcal skin infections? What factors are not stimulated in patients with glomerulonephritis preceded by streptococcal skin infections? What factors are detected in patients with acute rheumatic fever who have a negative ASO test result? Why testing for anti-DNase B is highly specific for group A streptococcal sequelae? What method has been developed for anti-DNase testing? What method has been developed for anti-DNase testing? What method has been developed for anti-DNase testing? What method has been developed for anti-DNase testing? The classic test for the measurement of anti-DNase B activity is based on what? Presence of DNase is measured by its effect on what factor? If a DNA-methyl conjugate is intact, what color does it retain? A green color intensity of between 2+ and 4+ are demonstrating What is normal anti-DNase B titers for patient’s age the geographic location the season of the year at least 240 Todd units in an adult at least 320 Todd units in a child nephelometric within 1 to 2 weeks after infection between 3 to 6 weeks following the initial symptoms anti-DNase B ASO antibodies antibodies to DNase B DNase B is mainly produced by group A streptococci Macrotiter microtiter EIA nephelometric methods a neutralization methodology a DNA-methyl green conjugate Green Positive result 240 to 640 units 59 Immuno PPT Flashcards Unit 3 children between the ages of 2 and 12 years? What test can be used for rapid quantitation of anti-DNase B? What is a slide agglutination screening test for the detection of antibodies to several streptococcal antigens? In Streptozyme test what are coated with streptolysin, streptokinase, hyaluronidase, DNase, and NADase? What does sheep red blood cells coated with streptolysin, streptokinase, hyaluronidase, DNase, and NADase for? What test is rapid and simple to perform, but less reproducible? In what test more false positives and false negatives have been reported? What titrations are performed at weekly or biweekly intervals following the onset of symptoms in Streptozyme testing? What is a gram-negative, microaerophilic spiral bacterium, cause of both gastric and duodenal ulcers? What method is used to determine presence of the H. pylori? Endoscopy used to determine presence of H. pylori include: Endoscopy used to determine presence of H. pylori include: Endoscopy used to determine presence of H. pylori include: The most specific test to detect H. pylori infection is The sensitivity of culture test is usually lower than other methods because: Procedures that do not require the use of endoscopy include: Procedures that do not require the use of endoscopy include: Procedures that do not require the use of endoscopy include: Procedures that do not require the use of endoscopy include: What is the primary screening method of determining infection with H. pylori? Infections from H. pylori result in what Nephelometry The Streptozyme test sheep red blood cells antibodies to any of the streptococcal antigens can be detected Streptozyme test Streptozyme test Several titrations Helicobacter pylori Stomach endoscopy histologic examination of gastric biopsy tissue urease biopsy test some molecular assays Culture H. pylori is not evenly distributed throughout the tissue urea breath testing enzyme immunoassays for bacterial antigens in the feces molecular tests for H. pylori DNA antibody tests Serological testing IgG, IgA, and IgM 60 Immuno PPT Flashcards Unit 3 antibodies production? The presence of antibody in the blood of an untreated patient indicates what? The presence of antibody in the blood of an untreated patient indicates an active infection because: In treated individuals, how is changed the antibody concentrations after about 6 months? If treatment considered successful, how is changed the concentration of antibody? What is the most serological test in clinical use of detection H. pylori? Testing for presence of what antibody does lack clinical value, since most infections have become chronic before diagnosis? Measurement of the antibodies may be done by what technique? Measurement of the antibodies may be done by what technique? What is used in rapid test of measurement antibodies? What is used in rapid test of measurement antibodies? What technique is reliable and accurate for the detection of H. pylori antibodies? Tests employing antigens from a pooled extract from what strain yield the best sensitivity? Why do tests employing antigens from a pooled extract from multiple and genetically diverse strains yield the best sensitivity? Most patients produce antibodies against what proteins? What is indicating a severe case of gastritis or gastric carcinoma? What is a member of a unique group of organisms that belong to the class Mollicutes? What organisms do lack cell walls and have complex growth requirements? What does make culture of Mycoplasma organisms difficult and time-consuming? an active infection the bacterium does not spontaneously clear Decrease about 50 percent A decrease of more than 25 percent H. pylori–specific antibodies of the IgG class IgM antibody ELISA Immunoblot latex agglutination flow-through membrane-based enzyme immunoassay. ELISA technique from multiple and genetically diverse strains H. pylori is heterogeneous CagA and VacA proteins antibodies against the CagA and VacA proteins Mycoplasma Mycoplasma lack cell walls and complex growth requirements 61 Immuno PPT Flashcards Unit 3 What difficulties can occur in culture of Mycoplasma? What infection are found in all age groups and can often spread through households? What infection have following symptoms: sore throat, chills, hoarseness, tracheobronchitis, and headache What infection may remain in the respiratory tract for several months, causing chronic inflammation? Laboratory diagnosis of Mycoplasma pneumoniae involved testing for what factor that are present in about 50 percent of patients with the infection? What are autoantibodies that react with the I/i antigens on red blood cells and cause their agglutination at temperatures below 37°C? Testing for presence of what factor is no longer recommended for the detection of M. pneumoniae infections? In what diseases cold agglutinins are also produced? What M. pneumoniae–specific serological tests have been developed? What M. pneumoniae–specific serological tests have been developed? What M. pneumoniae–specific serological tests have been developed? What M. pneumoniae–specific serological tests have been developed? What antibodies to M. pneumoniae may be detected by M. pneumoniae–specific serological tests? What tests are the most widely used method of detection M. pneumonia? What test do require a small sample volume and can test large numbers of specimens in an automated format? It is better to test for the presence of what antibodies for greater accuracy, but separately? What test can also detect IgM or IgG classes of antibody to M. pneumonia? growth may take several weeks and requires specialized media Mycoplasma pneumoniae infections Mycoplasma pneumoniae infection Mycoplasma pneumoniae infection cold agglutinins cold agglutinins cold agglutinins some viral infections and collagen vascular diseases enzyme immunoassay particle agglutination indirect immunofluorescence complement fixation IgM, IgG, and IgA EIA EIA IgG and IgM The slide-based indirect fluorescent assay (IFA) 62 Immuno PPT Flashcards Unit 3 If the screening test is positive, what should be done to quantify the amount of antibody present? What test may be performed using throat swabs, nasopharyngeal swabs, sputum, fixed tissue, and cultures? What test is obtaining rapid results, only one specimen is required, and live organisms are not required (the organism is subject to rapid drying with no cell walls)? What are short rods, or coccobacilli, obligate, intracellular, gram-negative bacteria? The genus Rickettsia is made up what groups? What diseases are associated with arthropods, spend at least part of their life cycle in an arthropod host before being transmitted to humans? Arthropod hosts ticks, mites, lice, and fleas are for what diseases? Humans are accidental hosts for Rickettsiae except for what organism which causes epidemic typhus? What are the main rickettsial diseases in the United States? Typhus endemic is caused by: Typhus epidemic is caused by: Rocky Mountain spotted fever is caused by: What is the method of choice for detecting rickettsial infections? What method may be used to detect rickettsial infections? What method may be used to detect rickettsial infections? Antibodies produced in patients with rickettsial infections were detected by an agglutination test known as what test? Weil-Felix test was based on what? Weil-Felix test was based on crossreactivity of the patient’s antibodies with polysaccharide antigens present on the OX-19 and OX-2 strains of __________ and the OX-K strain of____________: serial dilution PCR testing for Mycoplasma PCR testing for Mycoplasma Rickettsiae the spotted fever group (SFG) and the typhus group (TG) Rickettsial diseases Rickettsial diseases Rickettsia prowazekii Typhus (endemic and epidemic) and Rocky Mountain spotted fever R. typhi R. felis R. rickettsii Serodiagnosis probe-based immunoassays agglutination assays Weil-Felix test cross-reactivity Proteus vulgaris Proteus mirabilis 63 Immuno PPT Flashcards Unit 3 What is the one of organism-specific serological assay for rickettsial antibodies? What is the one of organism-specific serological assay for rickettsial antibodies? What is the one of organism-specific serological assay for rickettsial antibodies? What is the one of organism-specific serological assay for rickettsial antibodies? What is the one of organism-specific serological assay for rickettsial antibodies? What tests are currently considered the gold standard for detecting rickettsial antibodies? Testing by what methods can detect significant titers of antibodies in Rocky Mountain spotted fever by the second week of infection? Testing by IFA and micro-IF can detect titers of antibodies in Rocky Mountain spotted fever by when? Antirickettsial treatment needs to be started by what day of illness in order to be successful? indirect fluorescent assays (IFA) microimmunofluorescent assays (micro-IF) immunoperoxidase assays (IPA) ELISA immunoblot assays (IBA) IFA and micro-IF IFA and micro-IF by the second week of infection By the fifth day of infection 64
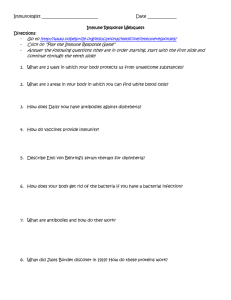




![Immune Sys Quiz[1] - kyoussef-mci](http://s3.studylib.net/store/data/006621981_1-02033c62cab9330a6e1312a8f53a74c4-300x300.png)